Brown Rice vs Wild Rice – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing brown rice to wild rice, we picked the wild.
Why?
It’s close! But there are important distinctions.
First let’s clarify: despite the name and appearance, wild rice is botanically quite different from rice per se; it’s not the same species, it’s not even the same genus, though it is the same umbrella family. In other words, they’re about as closely related as humans and gorillas are to each other.
In terms of macros, wild rice has considerably more protein and a little more fiber, for slightly lower carbs.
Notably, however, wild rice’s carbs are a close-to-even mix of sucrose, fructose, and glucose, while brown rice’s carbs are 99% starch. Given the carb to fiber ratio, it’s worth noting that wild rice also has lower net carbs, and the lower glycemic index.
In the category of vitamins, wild rice leads with more of vitamins A, B2, B9, E, K, and choline. In contrast, brown rice has more of vitamins B1, B3, and B5. So, a moderate win for wild rice.
When it comes to minerals, brown rice finally gets a tally in its favor, even if only slightly: brown rice has more magnesium, manganese, phosphorus, and selenium, while wild rice has more copper, potassium, and zinc. They’re equal in calcium and iron, by the way. Still, this category stands as a 4:3 win for brown rice.
Adding up the categories makes a modest win for wild rice, and additionally, if we had to consider one of these things more important than the others, it’d be wild rice being higher in fiber and protein and lower in total carbs and net carbs.
Still, enjoy either or both, per your preference!
Want to learn more?
You might like to read:
- Brown Rice Protein: Strengths & Weaknesses
- Rice vs Buckwheat – Which is Healthier? ← it’s worth noting, by the way, that buckwheat is so unrelated from wheat that it’s not even the same family of plants. They are about as closely related as a lion and a lionfish are to each other.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cannabis & Heart Attacks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For many, cannabis use has taken the place that alcohol used to have when it comes to wanting a “downer”, that is to say, a drug that relaxes us as opposed to stimulating us.
Indeed, it is generally considered safer than alcohol ← however this is not a strong claim, because alcohol is much more dangerous than one would think given its ubiquity and (in many places, at least) social acceptability.
We’ve talked a bit about cannabis use before, in its various forms, for example:
Cannabis Myths vs Reality ← a very good starting point for the curious
And one specifically about the use of THC gummies (THC is the psychoactive compound in cannabis, i.e. it’s the chemical that gets people high, as opposed to CBD, which is not psychoactive) as a sleep aid:
Sweet Dreams Are Made of THC (Or Are They?)
And for those skipping the THC, we’ve also written about CBD use, including:
CBD Oil: What Does The Science Say? and Do CBD Gummies Work?
So, about cannabis and heart attacks
Alcohol is a relaxant, and yet it can contribute to heart disease (amongst many other things, of course):
Can We Drink To Good Health? ← this is mostly about red wine’s putative heart health benefits, how the idea got popularized, and how it doesn’t stand up to scrutiny when actually looking at the evidence.
And cannabis, another relaxant? Not so good either!
New research has shown that cannabis users have a higher risk of heart attacks, even among younger and otherwise healthy individuals. This is based on analyzing data from 4,636,628 relatively healthy adults.
Specifically, the data showed that even young healthy cannabis users get:
- Sixfold increased risk of heart attack
- Fourfold increased risk of ischemic stroke
- Threefold increased risk of cardiovascular death, heart attack, or stroke
We mention the otherwise “relatively healthy” nature of the participants, because it’s important to note that less healthy people (who were perhaps using cannabis to self-medicate for some serious condition) were not included in the dataset, as it’d skew the data unhelpfully and it’d make the risk look a lot higher than the risk levels we mentioned above.
The mechanisms by which cannabis affects heart health are not fully understood, but hypotheses include:
- Disrupting heart rhythm regulation
- Increasing oxygen demand in the heart muscle
- Causing endothelial dysfunction, which affects blood vessel function
Further, heart attack risk peaked one hour after cannabis use, and while this doesn’t prove causality, it certainly doesn’t make cannabis look safe.
You can read the paper in its entirety here:
Want a safer way to relax?
We recommend:
- No-Frills, Evidence-Based Mindfulness
- Meditation Games That You’ll Actually Enjoy
- Which Style Of Yoga Is Best For You?
- 7 Kinds Of Rest When Sleep Is Not Enough
- Better Sex = Longer Life (Here’s How)
Enjoy!
Share This Post
-
Brain Food – by Dr. Lisa Mosconi
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know that we should eat for brain health, but often that knowledge doesn’t go a lot further than “we should eat some nuts… but also not the wrong nuts, which would be bad”.
However, as Dr. Lisa Mosconi lays out for us, there’s a lot more than that!
This book is as much a treatise of brain health in the context of nutrition, as it is a “eat this and avoid that” guide.
Which is good, because our brains don’t exist in isolation, and nor do the nutrients that we consume. Put it this way:
We have a tendecy to think of our diets as a set of slider-bars, “ok, that’s 104% of my daily intake of fiber, I need another 10g protein and that’ll be at 100%, I’ve had 80% of the vitamin C that I need, and…”
Whereas in reality: much of what we eat interacts positively or negatively with other things, and thus needs to be kept in balance. And not only that, but other peri-nutritional factors play a big part too! From obvious things like hydration, to less obvious things like maintaining good gut microbiota, our brains rely on us to do a lot of things for them.
This book is very easy-reading, though a weakness is it doesn’t tend to summarise key ideas much, give cheat-sheets, that sort of thing. We recommend reading this book with a notebook to the side, to jot down things you want to attend to in your own dietary habits.
Bottom line: this is an excellent overview of brain health in the context of nutrition, and is more comprehensive than most “eat this for good brain health and avoid that” books.
Click here to check out “Brain Food” on Amazon and treat your brain like it deserves!
Share This Post
-
Get Better Sleep: Beyond “Sleep Hygiene”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Better Sleep, Better Life!
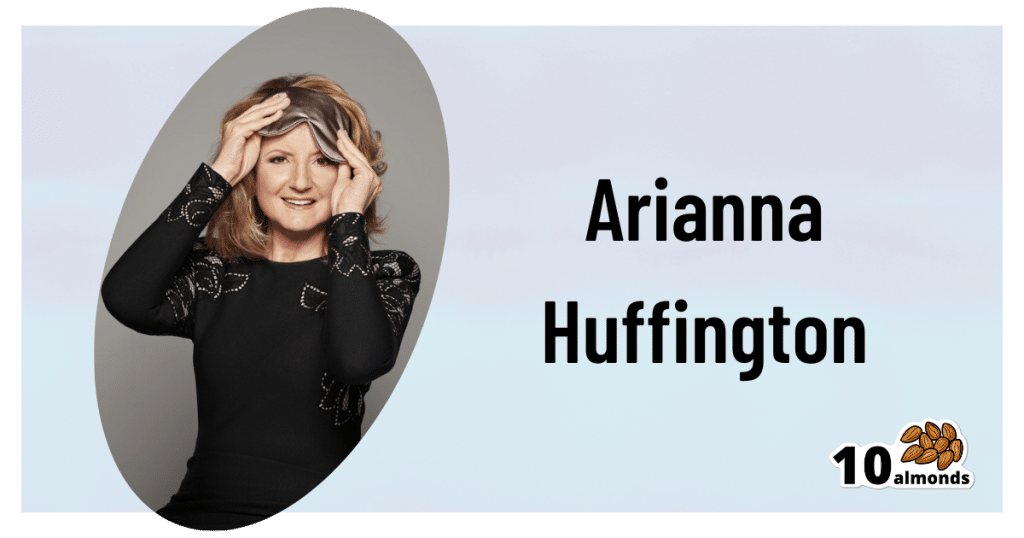
This is Arianna Huffington. Yes, that Huffington, of the Huffington Post. But! She’s also the CEO of Thrive Global, a behavior change tech company with the mission of changing the way we work and live—in particular, by challenging the idea that burnout is the required price of success.
The power of better sleep
Sleep is a very important, but most often neglected, part of good health. Here are some of Huffington’s top insights from her tech company Thrive, and as per her “Sleep Revolution” initiative.
Follow your circadian rhythm
Are you a night owl or a morning lark? Whichever it is, roll with it, and plan around that if your lifestyle allows for such. While it is possible to change from one to the other, we do have a predisposition towards one or the other, and will generally function best when not fighting it.
This came about, by the way, because we evolved to have half of us awake in the mornings and half in the evenings, to keep us all safe. Socially we’ve marched onwards from that point in evolutionary history, but our bodies are about a hundred generations behind the times, and that’s just what we have to work with!
Don’t be afraid (or ashamed!) to take naps
Naps, done right, can be very good for the health—especially if we had a bad night’s sleep the previous night.
Thrive found that workers are more productive when they have nap rooms, and (following on a little from the previous point) are allowed to sleep in or work from home.
See also: How To Nap Like A Pro (No More “Sleep Hangovers”!)
Make sure you have personal space available in bed
The correlation between relationship satisfaction and sleeping close to one’s partner has been found to be so high that it’s even proportional: the further away a couple sleeps from each other, the less happy they are. But…
Partners who got good sleep the previous night, will be more likely to want intimacy on any given night—at a rate of an extra 14% per extra hour of sleep the previous night. So, there’s a trade-off, as having more room in bed tends to result in better sleep. Time to get a bigger bed?
What gets measured, gets done
This goes for sleep, too! Not only does dream-journaling in the morning cue your subconscious to prepare to dream well the following night, but also, sleep trackers and sleep monitoring apps go a very long way to improving sleep quality, even if no extra steps are consciously taken to “score better”.
We’ve previously reviewed some of the most popular sleep apps; you can check out for yourself how they measured up:
Share This Post
Related Posts
-
Is It Possible To Lose Weight Quickly?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In Victorian England, weight-loss trends like the dangerous tapeworm diet were popular. While modern fad diets can seem less extreme, they often promise similarly fast results. However, these quick fixes can have similarly harmful consequences:
Not so fast
To illustrate the difference between gradual and extreme dieting, the video bids us consider two identical twins, Sam and Felix:
- Sam adopts a gradual approach, slowly reducing calorie intake and exercising regularly. This causes his body to burn glycogen stores before transitioning to fat as an energy source. Regular exercise helps Sam maintain muscle mass, which boosts his metabolism and supports sustained weight loss.
- Felix drastically cuts calories, forcing his body into starvation mode. He quickly depletes glycogen stores, loses muscle mass, and burns fewer calories, making long-term weight loss more difficult. Although Felix might initially lose water weight, this is temporary and unsustainable.
You cannot “just lose it quickly now, and then worry about healthiness once the weight’s gone”, because you will lose health much more quickly than you will lose fat, and that will sabotage, rather than help, your fat loss journey.Healthy weight loss requires gradual, balanced changes in diet and exercise tailored to individual needs. Extreme diets, whether through calorie restriction or things like elimination of carbs or fats, are unsustainable and shock the body. It’s important to prioritize long-term health over societal pressures for quick weight loss and focus on developing a sustainable, healthy lifestyle.
In short, the quickest way to lose weight and keep it off (without dying), is to lose it slowly.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Lose Weight (Healthily)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cordyceps: Friend Or Foe?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cordyceps: friend or foe?
Cordyceps is a famously frightening fungus. It’s the one responsible for “zombie ants” and other zombie creatures, and it’s the basis for the existential threat to humanity in the TV show The Last of Us.
It’s a parasitic fungus that controls the central and peripheral nervous systems of its host, slowly replacing the host’s body, as well as growing distinctive spines that erupt out of the host’s body. Taking over motor functions, it compels the host to do two main things, which are to eat more food, and climb to a position that will be good to release spores from.
Fortunately, none of that matters to humans. Cordyceps does not (unlike in the TV show) affect humans that way.
What does Cordyceps do in humans?
Cordyceps (in various strains) is enjoyed as a health supplement, based on a long history of use in Traditional Chinese Medicine, and nowadays it’s coming under a scientific spotlight too.
The main health claims for it are:
- Against inflammation
- Against aging
- Against cancer
- For blood sugar management
- For heart health
- For exercise performance
Sounds great! What does the science say?
There’s a lot more science for the first three (which are all closely related to each other, and often overlapping in mechanism and effect).
So let’s take a look:
Against inflammation
The science looks promising for this, but studies so far have either been in vitro (cell cultures in petri dishes), or else murine in vivo (mouse studies), for example:
- Anti-inflammatory effects of Cordyceps mycelium in murine macrophages
- Cordyceps sinensis as an immunomodulatory agent
- Immunomodulatory functions of extracts from Cordyceps cicadae
- Cordyceps pruinosa inhibits in vitro and in vivo inflammatory mediators
In summary: we can see that it has anti-inflammatory properties for mice and in the lab; we’d love to see the results of studies done on humans, though. Also, while it has anti-inflammatory properties, it performed less well than commonly-prescribed anti-inflammatory drugs, for example:
❝C. militaris can modulate airway inflammation in asthma, but it is less effective than prednisolone or montelukast.❞
Against aging
Because examining the anti-aging effects of a substance requires measuring lifespans and repeating the experiment, anti-aging studies do not tend to be done on humans, because they would take lifetimes to perform. To this end, it’s inconvenient, but not a criticism of Cordyceps, that studies have been either mouse studies (short lifespan, mammals like us) or fruit fly studies (very short lifespan, genetically surprisingly similar to us).
The studies have had positive results, with typical lifespan extensions of 15–20%:
- The lifespan-extending effect of Cordyceps sinensis in normal mice
- Cordyceps sinensis oral liquid prolongs the lifespan of the fruit fly, Drosophila melanogaster
- Anti-aging activity of polysaccharides from Cordyceps militaris
- Anti-aging effect of Cordyceps sinensis extract
Against cancer
Once again, the studies here have been in vitro, or murine in vivo. They do look good though:
In vitro (human cell cultures in a lab):
In vivo (mouse studies):
Summary of these is: Cordyceps quite reliably inhibits tumor growth in vitro (human cell cultures) and in vivo (mouse studies). However, trials in human cancer patients are so far conspicuous by their absence.
For blood sugar management
Cordyceps appears to mimic the action of insulin, without triggering insulin sensitivity. For example:
The anti-hyperglycemic activity of the fruiting body of Cordyceps in diabetic rats
There were some other rat/mouse studies with similar results. No studies in humans yet.
For heart health
Cordyceps contains adenosine. You may remember that caffeine owes part of its stimulant effect to blocking adenosine, the hormone that makes us feel sleepy. So in this way, Cordyceps partially does the opposite of what caffeine does, and may be useful against arrhythmia:
Cardiovascular protection of Cordyceps sinensis act partially via adenosine receptors
For exercise performance
A small (30 elderly participants) study found that Cordyceps supplementation improved VO2 max by 7% over the course of six weeks:
However, another small study (22 young athletes) failed to reproduce those results:
Cordyceps Sinensis supplementation does not improve endurance exercise performance
In summary…
Cordyceps almost certainly has anti-inflammation, anti-aging, and anti-cancer benefits.
Cordyceps may have other benefits too, but the evidence is thinner on the ground for those, so far.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Pillars of Weight Loss Explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Surprise, diet is #6 and exercise is #7:
How many do you do?
If your body is a temple, these are its eight pillars:
- Emotional freedom and resilience: understanding how the mind works and using techniques such as CBT, neurolinguistic programming, and meditation to reduce psychological stress and improve self-awareness.
- Vagal tone improvement: techniques to get the body out of fight-or-flight mode, improving blood flow, digestion, and reducing chronic pain.
- Lymphatic system support: to enhance your body’s internal cleanup system, boost energy, and alleviate pain.
- Gut health optimization: supporting digestion and gut health, so that your gut can work efficiently.
- Hormonal balance: addressing hormone imbalances to improve overall health, as well as supporting a healthy metabolism and weight loss.
- Dietary choices: choosing a sustainable diet that balances blood sugar, boosts metabolism, and suits your personal needs.
- Exercise and mobility: developing a sustainable workout plan that promotes fat loss, joint health, and muscle building.
- Habit formation: developing routines and habits to maintain progress and prevent relapse into old patterns.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Lose Weight (Healthily!) ← our own main feature on the topic, detailing the best kinds of diet and exercise adjustments, as well as how to go about tending to some of the other factors mentioned above
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: