Sweet Dreams Are Made of THC (Or Are They?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I’m one of those older folks that have a hard time getting 7 hrs. I know a lot of it my fault…like a few beers at nite…🥰am now trying THC gummies for anxiety, instead of alcohol……less calories 😁how does THC affect our sleep,? Safer than alcohol…..I know your next article 😊😊😊😊❣️😊alot of us older kids do take gummies 😲😲😲thank you❞
Great question! We wrote a little about CBD gummies (not THC) before:
…and went on to explore THC’s health benefits and risks here:
For starters, let’s go ahead and say: you’re right that it’s safer (for most people) than alcohol—but that’s not a strong claim, because alcohol is very bad for pretty much everything, including sleep.
So how does THC measure up when it comes to sleep quality?
Good news: it affects the architecture of sleep in such a way that you will spend longer in deep sleep (delta wave activity), which means you get more restorative and restful sleep!
See also: Alpha, beta, theta: what are brain states and brain waves? And can we control them?
Bad news: it does so at the cost of reducing your REM sleep, which is also necessary for good brain health, and will cause cognitive impairment if you skip too much. Normally, if you are sleep-deprived, the brain will prioritize REM sleep at the cost of other kinds of sleep; it’s that important. However, if you are chemically impaired from getting healthy REM sleep, there’s not much your brain can do to save you from the effects of REM sleep loss.
See: Cannabis, Cannabinoids, and Sleep: a Review of the Literature
This is, by the way, a reason that THC gets prescribed for some sleep disorders, in cases where the initial sleep disruption was because of nightmares, as it will reduce those (along with any other dreams, as collateral damage):
One thing to be careful of if using THC as a sleep aid is that withdrawal may make your symptoms worse than they were to start with:
Updates in the use of cannabis for insomnia
With all that in mind, you might consider (if you haven’t already tried it) seeing whether CBD alone improves your sleep, as while it does also extend time in deep sleep, it doesn’t reduce REM nearly as much as THC does:
👆 this study was paid for by the brand being tested, so do be aware of potential publication bias. That’s not to say the study is necessarily corrupt, and indeed it probably wasn’t, but rather, the publication of the results was dependent on the company paying for them (so hypothetically they could have pulled funding from any number of other research groups that didn’t get the results they wanted, leaving this one to be the only one published). That being said, the study is interesting, which is why we’ve linked it, and it’s a good jumping-off-point for finding a lot of related papers, which you can see listed beneath it.
CBD also has other benefits of its own, even without THC:
CBD Oil: What Does The Science Say?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Herbs For Evidence-Based Health & Healing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Herbs have been used since prehistoric times to treat injuries and illnesses, but which ones actually work, as opposed to being “old wives’ tales”?
Even today, in pharmacies herbals products may come with a disclaimer “based on traditional use only”, which, in scientific terms, means it likely performs no better than placebo.
This is a “Saturday Life Hacks” edition, not a “Research Review Monday”, so we won’t be doing any deep-dives today, and will instead keep things short and snappy. We’ll also spotlight one main benefit, rather than trying to cover all bases, as we often have room to do on a Monday!
Basil
Helps boost immunity:
Chamomile
Significantly reduces symptoms of osteoarthritis:
(This one challenged your writer’s resolve as it does so many things, it was hard to pick just one. So, she went with one that’s less known that “settling the stomach” and “relieving PMS” and “relaxation” and so forth)
Echinacea
Significantly reduces the risk of catching a cold (but won’t help once you’ve caught it):
Echinacea for preventing and treating the common cold
Elderberry
Significantly hastens recovery from upper respiratory viral infections:
Evening Primrose
Fights neuropathy, along with many other benefits:
An updated review on pharmacological activities and phytochemical constituents of evening primrose
Fennel
Antinflammatory, along with many other benefits:
Ginkgo biloba
Antioxidant effects provide anti-aging benefits:
Advances in the Studies of Ginkgo Biloba Leaves Extract on Aging-Related Diseases
Ginseng
Combats fatigue:
Ginseng as a Treatment for Fatigue: A Systematic Review
Lavender
Enjoyed for its sedative effects, which is really does have:
Evidence for Sedative Effects of the Essential Oil of Lavender after Inhalation
Sage
Helps fight HIV type 1 and Herpes simplex type 2 (and probably other viruses, but that’s what we have the science for right now):
Aqueous extracts from peppermint, sage and lemon balm leaves display potent anti-HIV-1 activity
Valerian
Inconclusive data; “traditional use only” for restful sleep.
Can’t have everything!
Share This Post
-
The Blue Zones Kitchen – by Dan Buettner
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Buettner’s other book, The Blue Zones: 9 Lessons For Living Longer From The People Who’ve Lived The Longest, and with this one, it’s now time to focus on the dietary aspect.
As the title and subtitle promises, we get 100 recipes, inspired by Blue Zone cuisines. The recipes themselves have been tweaked a little for maximum healthiness, eliminating some ingredients that do crop up in the Blue Zones but are exceptions to their higher average healthiness rather than the rule.
The recipes are arranged by geographic zone rather than by meal type, so it might take a full read-through before knowing where to find everything, but it makes it a very enjoyable “coffee-table book” to browse, as well as being practical in the kitchen. The ingredients are mostly easy to find globally, and most can be acquired at a large supermarket and/or health food store. In the case of substitutions, most are obvious, e.g. if you don’t have wild fennel where you are, use cultivated, for example.
In the category of criticism, it appears that Buettner is very unfamiliar with spices, and so has skipped them almost entirely. We at 10almonds could never skip them, and heartily recommend adding your own spices, for their health benefits and flavors. It may take a little experimentation to know what will work with what recipes, but if you’re accustomed to cooking with spices normally, it’s unlikely that you’ll err by going with your heart here.
Bottom line: we’d give this book a once-over for spice additions, but aside from that, it’s a fine book of cuisine-by-location cooking.
Click here to check out The Blue Zones Kitchen, and get cooking into your own three digits!
Share This Post
-
How Useful Are Our Dreams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s In A Dream?
We were recently asked:
❝I have a question or a suggestion for coverage in your “Psychology Sunday”. Dreams: their relevance, meanings ( if any) interpretations? I just wondered what the modern psychological opinions are about dreams in general.❞
~ 10almonds subscriber
There are two main schools of thought, and one main effort to reconcile those two. The third one hasn’t quite caught on so far as to be considered a “school of thought” yet though.
The Top-Down Model (Psychoanalysts)
Psychoanalysts broadly follow the theories of Freud, or at least evolved from there. Freud was demonstrably wrong about very many things. Most of his theories have been debunked and ditched—hence the charitable “or at least evolved from there” phrasing when it comes to modern psychoanalytic schools of thought. Perhaps another day, we’ll go into all the ways Freud went wrong. However, for today, one thing he wasn’t bad at…
According to Freud, our dreams reveal our subconscious desires and fears, sometimes directly and sometimes dressed in metaphor.
Examples of literal representations might be:
- sex dreams (revealing our subconscious desires; perhaps consciously we had not thought about that person that way, or had not considered that sex act desirable)
- getting killed and dying (revealing our subconscious fear of death, not something most people give a lot of conscious thought to most of the time)
Examples of metaphorical representations might be:
- dreams of childhood (revealing our subconscious desires to feel safe and nurtured, or perhaps something else depending on the nature of the dream; maybe a return to innocence, or a clean slate)
- dreams of being pursued (revealing our subconscious fear of bad consequences of our actions/inactions, for example, responsibilities to which we have not attended, debts are a good example for many people; or social contact where the ball was left in our court and we dropped it, that kind of thing)
One can read all kinds of guides to dream symbology, and learn such arcane lore as “if you dream of your teeth crumbling, you have financial worries”, but the truth is that “this thing means that other thing” symbolic equations are not only highly personal, but also incredibly culture-bound.
For example:
- To one person, bees could be a symbol of feeling plagued by uncountable small threats; to another, they could be a symbol of abundance, or of teamwork
- One culture’s “crow as an omen of death” is another culture’s “crow as a symbol of wisdom”
- For that matter, in some cultures, white means purity; in others, it means death.
Even such classically Freudian things as dreaming of one’s mother and/or father (in whatever context) will be strongly informed by one’s own waking-world relationship (or lack thereof) with same. Even in Freud’s own psychoanalysis, the “mother” for the sake of such analysis was the person who nurtured, and the “father” was the person who drew the nurturer’s attention away, so they could be switched gender roles, or even different people entirely than one’s parents.
The only real way to know what, if anything, your dreams are trying to tell you, is to ask yourself. You can do that…
- by reflection and personal interrogation (see for example: The Easiest Way To Take Up Journaling)
- or by externalising parts of your subconscious (as in Internal Family Systems therapy)
- or by talking directly to your subconscious where it is, by means of lucid dreaming.
The idea with lucid dreaming is that since any dream character is a facet of your subconscious generated by your own mind, by talking to that character you can ask questions directly of your subconscious (the popular 2010 movie “Inception” was actually quite accurate in this regard, by the way).
To read more about how to do this kind of self-therapy through lucid dreaming, you might want to check out this book we reviewed previously; it is the go-to book of lucid dreaming enthusiasts, and will honestly give you everything you need in one go:
Lucid Dreaming: A Concise Guide to Awakening in Your Dreams and in Your Life – by Dr. Stephen LaBerge
The Bottom-Up Model (Neuroscientists)
This will take a lot less writing, because it’s practically a null hypothesis (i.e., the simplest default assumption before considering any additional evidence that might support or refute it; usually some variant of “nothing unusual going on here”).
The Bottom-Up model holds that our brains run regular maintenance cycles during REM sleep (a biological equivalent of defragging a computer), and the brain interprets these pieces of information flying by and, because of the mind’s tendency to look for patterns, fills in the rest (much like how modern generative AI can “expand” a source image to create more of the same and fill in the blanks), resulting in the often narratively wacky, but ultimately random, vivid hallucinations that we call dreams.
The Hybrid Model (per Cartwright, 2012)
This is really just one woman’s vision, but it’s an incredibly compelling one, that takes the Bottom-Up model and asks “what if we did all that bio-stuff, and then our subconscious mind influenced the interpretation of the random patterns, to create dreams that are subjectively meaningful, and thus do indeed represent our subconscious?
It’s best explained in her own words, though, so it’s time for another book recommendation (we’ve reviewed this one before, too):
Enjoy!
Share This Post
Related Posts
-
The Drug & Supplement Combo That Reverses Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So far, its effects have been dramatic (in a good way) in mice; human trials are now underway.
How does it work?
It builds from previous work, in which a Japanese research team created an “anti-aging vaccine”, that responded to a problem more specific than aging as a whole, namely atherosclerosis.
They found that a certain* protein was upregulated (i.e., it was made at a greater rate resulting in greater quantities) in patients (mouse and human alike) with atherosclerosis. So, they immunized the mice against that protein, and long story short, everything improved for them, from their atherosclerosis to general markers of aging—including growing back fur that had been lost due to age-related balding (just like in humans). They also lived longer, as is to be expected of a mouse who is now biologically younger.
*To avoid being mysterious: it was glycoprotein nonmetastatic melanoma protein B, known to its friends as GPNMB.
You may be wondering: how can one be immunized against a protein? If so, do bear in mind, a virus is also a protein. In this case, they developed an RNA vaccine, that works in a similar way to the COVID vaccines we all know and love (albeit with a different target).
You can read about this in abundant detail here: Senolytic vaccination improves normal and pathological age-related phenotypes and increases lifespan in progeroid mice
Hot on the heels of that, new approaches were found, including…
The combination
We’ll not keep you waiting; the combination is dasatinib plus quercetin, or else fisetin alone.
It’s about killing senescent (aging) “zombie cells” while sparing healthy cells, which that drug (dasatinib) and those supplements (quercetin and fisetin) do.
The researchers noted:
❝Senescent cells are resistant to apoptosis, which is governed through the upregulation of senescent cell anti-apoptotic pathways (SCAPs). Compounds were subsequently identified that disrupted the SCAPs, inducing death of senescent cells while leaving healthy cells unaffected. Forty-six potential senolytic agents were discovered through this process. To advance translational efforts, the majority of research has focused on agents with known safety profiles and limited off-target effects (Kirkland and Tchkonia, 2020).
The best characterized senolytic agents are dasatinib, a tyrosine kinase inhibitor approved for use in humans for cancer treatment, and quercetin, a naturally occurring plant flavonoid. The agents have a synergistic effect, making their combination more potent for senescent cell clearance (Zhu et al., 2015). As senescent cells do not divide and accumulate over a period of weeks, they can be administered using an intermittent approach, which further serves to reduce the risk of side effects (Kirkland and Tchkonia, 2020).
In preclinical trials, the combination of dasatinib and quercetin (D + Q) have been found to alleviate numerous chronic medical conditions including vascular stiffness, osteoporosis, frailty, and hepatic stenosis❞
Source: A geroscience motivated approach to treat Alzheimer’s disease: Senolytics move to clinical trials
As to how they expanded on this research:
❝In our study, oral D + Q were intermittently administered to tau transgenic mice with late-stage pathology (approximated to a 70-year-old human with advanced AD) (Musi et al., 2018). The treatment effectively reduced cellular senescence and associated senescence-associated secretory phenotype incidence. The 35 % reduction in neurofibrillary tangles was accompanied by enhanced neuron density, decreased ventricular enlargement, diminished tau accumulation, and restoration of aberrant cerebral blood flow. A subsequent preclinical study validated the findings, reporting that intermittently administered D + Q cleared senescent cells in the central nervous system, reduced amyloid-β plaques, attenuated neuroinflammation, and enhanced cognition❞
Source: Ibid.
And now taking it to humans:
❝The first clinical trial of D + Q for early-stage Alzheimer’s Disease (AD) has completed enrollment (Gonzales et al., 2021). The primary aim of the open-label pilot study was to examine the central nervous system penetrance of D and Q in a small sample of older adults with early-stage AD (NCT04063124). In addition, two placebo-controlled trials of D + Q for neurodegenerative disease are underway (NCT04685590 and NCT04785300).
One of the trials in development is a multi-site, double-blind, randomized, placebo-controlled study of senolytic therapy in older adults with amnestic mild cognitive impairment (MCI) or early-stage dementia (Clinical Dementia Rating Scale (CDR) Global 0.5–1) due to AD (elevated CSF total tau/Aβ42 ratio).
The treatment regimen will consist of 12-weeks of intermittently administered oral D + Q.❞
Source: Ibid.
The study is actually completed now, but its results are not yet published (again, at time of writing). Which means: they have the data, and now they’re writing the paper.
We look forward to providing an update about that, when the paper is published!
In the meantime…
Dasatinib is a drug usually prescribed to people with certain kinds of leukemia, and suffice it to say, it’s prescription-only. And unlike drugs that are often prescribed off-label (such as metformin for weight loss), getting your doctor to prescribe you an anticancer drug is unlikely unless you have the cancer in question.
You may be wondering: how is an anticancer drug helpful against aging? And the answer is that cancer and aging are very interrelated, and both have to do with “these old cells just won’t die, and are using the resources needed for young healthy cells”. So in both cases, killing those “zombie cells” while sparing healthy ones, is what’s needed. However, your doctor will probably not buy that as a reason to prescribe you a drug that is technically chemotherapy.
Quercetin, on the other hand, is a readily-available supplement, as is fisetin, and both have glowing (in a good way) safety profiles.
Want to know more?
You can read more about each of quercetin and fisetin (including how to get them), here:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
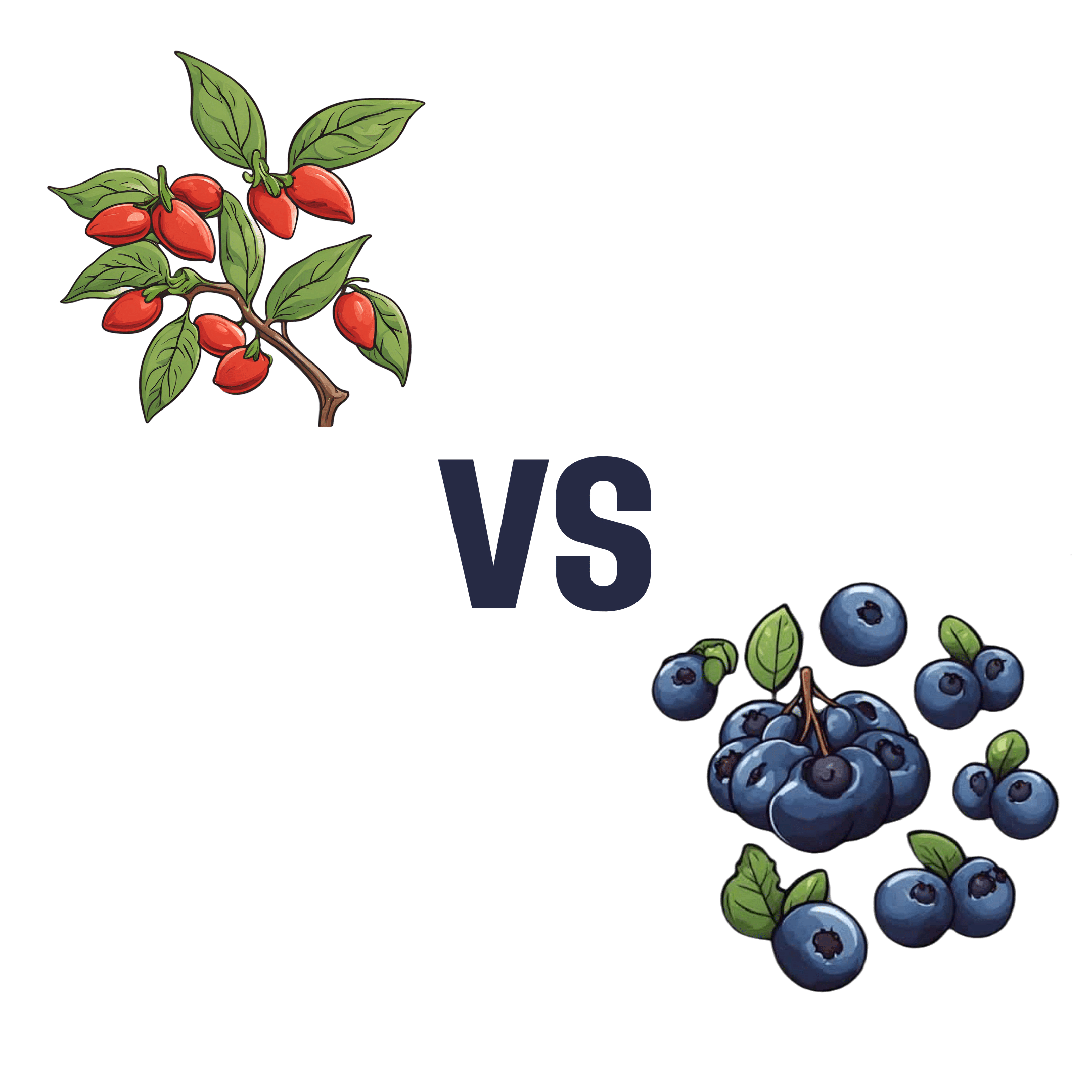
Goji Berries vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing goji berries to blueberries, we picked the goji berries.
Why?
As you might have guessed, both are very good options:
- Both have plenty of vitamins and minerals, and/but goji berries have more. How much more? It varies, but for example about 5x more vitamin C, about 25x more iron, about 30x more calcium, about 50x more vitamin A.
- Blueberries beat goji berries with some vitamins (B, E, K), but only in quite small amounts.
- Both are great sources of antioxidants, and/but goji berries have 2–4 times the antioxidants that blueberries do.
- Goji berries do have more sugar, but since they have about 4x more sugar and 5x more fiber, we’re still calling this a win for goji berries on the glycemic index front (and indeed, the GI of goji berries is lower).
In short: blueberries are great, but goji berries beat them in most metrics.
Want to read more?
Check out our previous main features, detailing some of the science, and also where to get them:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Women’s Strength Training Anatomy Workouts – by Frédéric Delavier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed another book of Delavier’s, “Women’s Strength Training Anatomy“, which itself is great. This book adds a lot of practical advice to that one’s more informational format, but to gain full benefit of this one does not require having read that one.
A common reason that many women avoid strength-training is because they do not want to look muscular. Largely this is based on a faulty assumption, since you will never look like a bodybuilder unless you also eat like a bodybuilder, for example.
However, for those for whom the concern remains, today’s book is an excellent guide to strength-training with aesthetics in mind as well as functionality.
The exercises are divided into sections, thus: round your glutes / tone your quadriceps / shape your hamstrings / trim your calves / flatten your abs / curve your shoulders / develop a pain-free upper back / protect your lower back / enhance your chest / firm up your arms.
As you can see, a lot of these are mindful of aesthetics, but there’s nothing here that’s antithetical to function, and some (especially for example “develop a pain-free upper back” and “protect your lower back“) are very functional indeed.
Bottom line: Delavier’s anatomy and exercise books are top-tier, and this one is no exception. If you are a woman and would like to strength-train (or perhaps you already do, and would like to refine your training), then this book is an excellent choice.
Click here to check out Women’s Strength Training Anatomy Workouts, and have the body you want!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: