The Emperor’s New Klotho, Or Something More?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
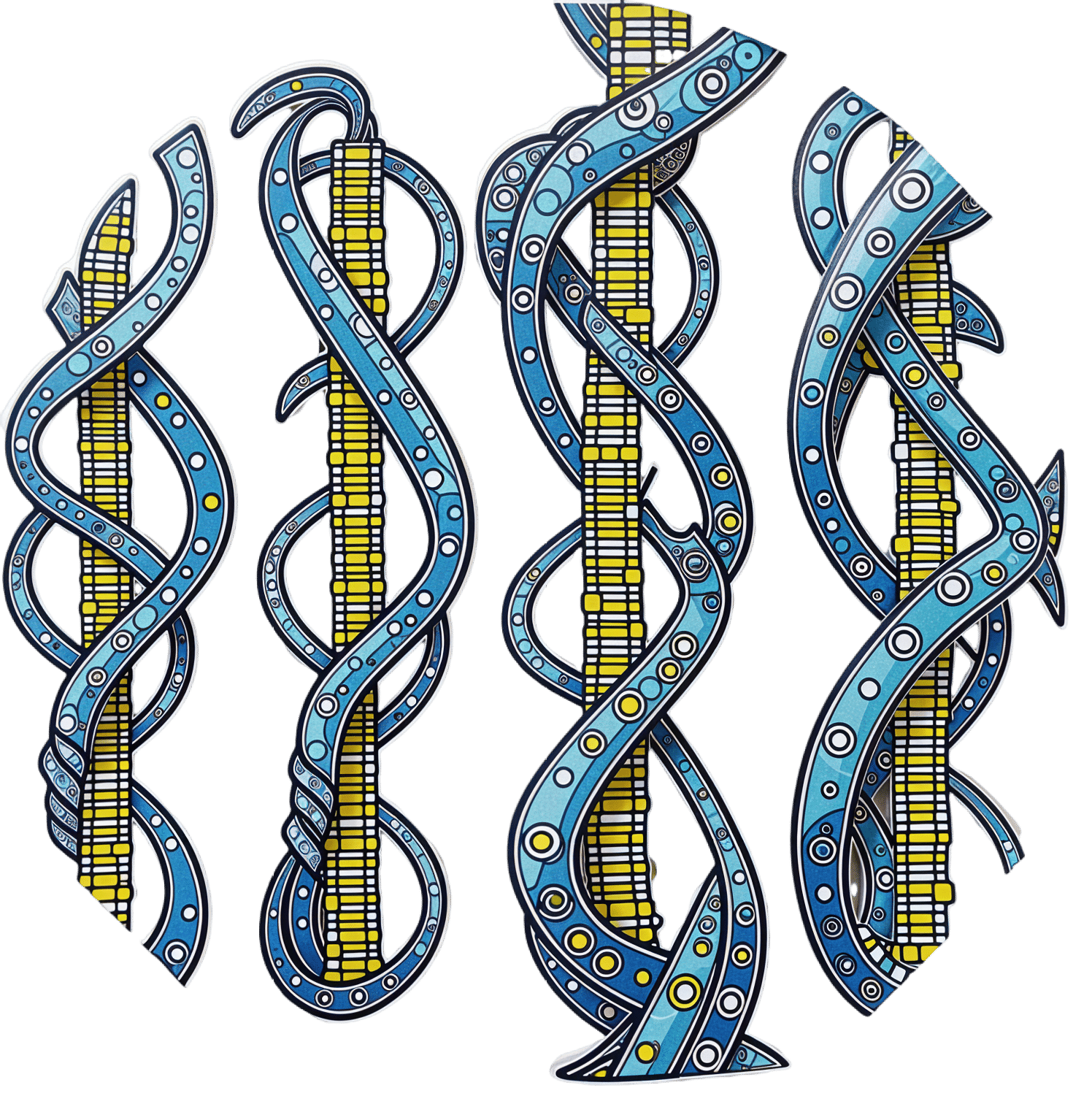
Unzipping The Genes Of Aging?
Klotho is an enzyme encoded in humans’ genes—specifically, in the KL gene.
It’s found throughout all living parts of the human body (and can even circulate about in its hormonal form, or come to rest in its membranaceous form), and its subgroups are especially found:
- α-klotho: in the brain
- β-klotho: in the liver
- γ-klotho: in the kidneys
Great! Why do we care?
Klotho, its varieties and variants, its presence or absence, are very important in aging.
Almost every biological manifestation of aging in humans has some klotho-related indicator; usually the decrease or mutation of some kind of klotho.
Which way around the cause and effect go has been the subject of much debate and research: do we get old because we don’t have enough klotho, or do we make less klotho because we’re getting old?
Of course, everything has to be tested per variant and per system, so that can take a while (punctuated by research scientists begging for more grants to do the next one). Given that it’s about aging, testing in humans would take an incredibly long while, so most studies so far have been rodent studies.
The general gist of the results of rodent studies is “reduced klotho hastens aging; increased klotho slows it”.
(this can be known by artificially increasing or decreasing the level of klotho expression, again something easier in mice as it is harder to arrange transgenic humans for the studies)
Here’s one example of many, of that vast set of rodent studies:
Suppression of Aging in Mice by the Hormone Klotho
Relevance for Alzheimer’s, and a science-based advice
A few years ago (2020), an Alzheimer’s study was undertaken; they noted that the famous apolipoprotein E4 (apoE4) allele is the strongest genetic risk factor for Alzheimer’s, and that klotho may be another. FGF21 (secreted by the liver, mostly during fasting) binds to its own receptor (FGFR1) and its co-receptor β-klotho. Since this is a known neuroprotective factor, they wondered whether klotho itself may interact with β-amyloid (Aβ), and found:
❝Aβ can enhance the ability of klotho to draw FGF21 to regions of incipient neurodegeneration in AD❞
In other words: β-amyloid, the substance whose accumulation is associated with neurodegeneration in Alzheimer’s disease, is a mediator in klotho bringing a known neuroprotective factor, FGF21, to the areas of neurodegeneration
In fewer words: klotho calls the firefighters to the scene of the fire
Read more: Alignment of Alzheimer’s disease amyloid β-peptide and klotho
The advice based on this? Consider practicing intermittent fasting, if that is viable for you, as it will give your liver more FGF21-secreting time, and the more FGF21, the more firefighters arrive when klotho sounds the alarm.
See also: Intermittent Fasting: What’s the truth?
…and while you’re at it:
Does intermittent fasting have benefits for our brain?
A more recent (2023) study with a slightly different (but connected) purpose, found results consistent with this:
Longevity factor klotho enhances cognition in aged nonhuman primates
…and, for that matter this (2023) study that found:
Associations between klotho and telomere biology in high stress caregivers
…which looks promising, but we’d like to see it repeated with a sounder method (they sorted caregiving into “high-stress” and “low-stress” depending on whether a child was diagnosed with ASD or not, which is by no means a reliable way of sorting this). They did ask for reported subjective stress levels, but to be more objective, we’d like to see clinical markers of stress (e.g. cortisol levels, blood pressure, heart rate changes, etc).
A very recent (April 2024) study found that it has implications for more aspects of aging—and this time, in humans (but using a population-based cohort study, rather than lab conditions):
Can I get it as a supplement?
Not with today’s technology and today’s paucity of clinical trials, you can’t. Maybe in the future!
However… The presence of senescent (old, badly copied, stumbling and staggering onwards when they should have been killed and eaten and recycled already) cells actively reduces klotho levels, which means that taking supplements that are senolytic (i.e., that kill those senescent cells) can increase serum klotho levels:
Orally-active, clinically-translatable senolytics restore α-Klotho in mice and humans
Ok, what can I take for that?
We wrote about a senolytic supplement that you might enjoy, recently:
Fisetin: The Anti-Aging Assassin
Want to know more?
If you have the time, Dr. Peter Attia interviews Dr. Dena Dubal (researcher in several of the above studies) here:
Click Here If The Embedded Video Doesn’t Load Automatically
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Insomnia? High blood pressure? Try these!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Your Questions, Our Answers!
Q: Recipes for insomnia and high blood pressure and good foods to eat for these conditions?
A: Insomnia can be caused by many things, and consequently can often require a very multi-vector approach to fixing it. But, we’ll start by answering the question you asked (and probably address the rest of dealing with insomnia in another day’s edition!):
- First, you want food that’s easy to digest. Broadly speaking, this means plant-based. If not plant-based, fish (unless you have an allergy, obviously) is generally good and certainly better than white meat, which is better than red meat. In the category of dairy, it depends so much on what it is, that we’re not going to try to break it down here. If in doubt, skip it.
- You also don’t want blood sugar spikes, so it’s good to lay off the added sugar and white flour (or white flour derivatives, like white pasta), especially in your last meal of the day.
- Magnesium supports healthy sleep. A fine option would be our shchi recipe, but using collard greens rather than cabbage. Cabbage is a wonderful food, but collard greens are much higher in magnesium. Remember to add plenty of mushrooms (unless you don’t like them), as they’re typically high in magnesium too.
As for blood pressure, last month we gave tips (and a book recommendation) for heart health. The book, Dr. Monique Tello’s “Healthy Habits for Your Heart: 100 Simple, Effective Ways to Lower Your Blood Pressure and Maintain Your Heart’s Health”, also has recipes!
Here’s one from the “mains” section:
Secret Ingredient Baltimore-Style Salmon Patties with Not-Oily Aioli
❝This is a family favorite, and no one knows that it features puréed pumpkin! Most salmon cake recipes all for eggs and bread crumbs as binders, but puréed pumpkin and grated carrot work just as well, lend a beautiful color, and add plenty of fiber and plant nutrients. Canned salmon is way cheaper than fresh and has just as much omega-3 PUFAs and calcium. Serve this alongside a salad (the Summer Corn, Tomato, Spinach, and Basil Salad would go perfectly) for a well-rounded meal.❞
Serves 4 (1 large patty each)
Secret Ingredient Baltimore-Style Salmon Patties:
- 1 (15-oz) can pink salmon, no salt added
- ½ cup puréed pumpkin
- ½ cup grated carrot (I use a handheld box grater)
- 2 tablespoons minced chives (Don’t have chives? Minced green onions or any onions will do)
- 2 teaspoons Old Bay Seasoning
- 1 tablespoon olive oil
- ½ large lemon, sliced, for serving
Not-Oily Aioli:
- ½ cup plain low-fat Greek yogurt
- Juice and zest from ½ large lemon
- 1 clove garlic, crushed and minced fine
- 2 tablespoons chopped fresh dill
- For the patties: mix all the ingredients for the salmon patties together in a medium bowl
- Form patties with your hands and set on a plate or tray (you should have 4 burger-sized patties)
- Heat oil in a large skillet over medium heat.
- Set patties in a skillet and brown for 4 minutes, then carefully flip.
- Brown the other side, then serve hot.
- For the Aioli: mix all the ingredients for the aioli together in a small bowl.
- Plop a dollop alongside or on top of each salmon patty and serve with a spice of lemon.
Per serving: Calories: 367 | Fat: 13.6g | Saturated Fat: 4.4g | Protein: 46g | Sodium: 519mg | Carbohydrates: 13.2g | Fiber: 1.3g | Sugars: 9g | Calcium: 505mg | Iron: 1mg | Potassium 696mg
Notes from the 10almond team:
- If you want to make it plant-based, substitute cooked red lentils (no salt added) for the tinned salmon, and plant-based yogurt for the Greek yogurt
- We recommend adding more garlic. Seriously, who uses 1 clove of garlic for anything, let alone divided between four portions?
- The salads mentioned are given as recipes elsewhere in the same book. We strongly recommend getting her book, if you’re interested in heart health!
Do you have a question you’d like to see answered here? Hit reply or use the feedback widget at the bottom; we’d love to hear from you!
Share This Post
-
What Different Kinds of Hair Loss/Thinning Say About Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Siobhan Deshauer shows us different kinds of hair loss, what causes them, and what can be done about them:
Many different causes
Here’s how to tell them apart:
- Alopecia areata is an autoimmune condition where the immune system mistakenly attacks hair follicles, causing hair loss that can occur at any age and affects about 1 in 50 people. It often presents as smooth patches of hair loss and can be treated with steroid injections. Severe cases may require high-dose prednisone, which can restore hair growth over time.
- Discoid lupus is an autoimmune disease that affects the skin, leading to inflammation, scarring, and permanent hair loss. Unlike alopecia areata, it causes visible damage to the scalp and hair follicles. This type of lupus typically does not involve internal organs, unlike systemic lupus.
- Telogen effluvium occurs when a major systemic shock, such as an infection, surgery, or significant stress, triggers many hair follicles to enter the resting phase simultaneously, resulting in delayed hair shedding. The condition is diagnosed with a “hair pull test” and is typically temporary, as the resting phase is followed by normal hair growth phases.
- Allergic reactions to products, such as hair dye containing PPD, can cause hair loss due to scalp irritation and inflammation. An allergic response may trigger hair follicles to enter a resting phase, leading to hair loss by the same mechanism as telogen effluvium. Treatment with steroids can calm the reaction, and hair usually regrows after recovery.
- Syphilis, a sexually transmitted infection, can present with varied symptoms, including hair loss in a distinct moth-eaten pattern. Hair loss due to syphilis is reversible and curable with penicillin treatment, with hair regrowth typically occurring a few months after treatment.
- Biotin deficiency is rare due to its production by gut bacteria and presence in foods such as nuts, seeds, and beans such as soybeans. Deficiency can result from excessive consumption of raw egg whites, which block absorption. Severe deficiency causes hair loss and skin issues but can be treated effectively with biotin supplements.
- Iron deficiency anemia can cause hair thinning along with symptoms like fatigue and breathlessness. It often results from inadequate dietary intake, but can also occur after heavy menstrual bleeding. Treatment with iron supplements, or blood transfusions in severe cases, can restore both hair and energy levels, leading to significant improvements.
- Trichotillomania is a psychological condition marked by an uncontrollable urge to pull out one’s hair, often associated with anxiety or depression. Hair patches may show different stages of regrowth. While it can be challenging to manage, the condition can be treated with appropriate psychological and medical support.
- Traction alopecia results from hairstyles that exert prolonged tension on the hair, causing it to thin or fall out. This type of hair loss can be prevented by reducing the strain on the hair. Loosening hairstyles and giving the scalp a break can help hair regrow over time.
- Hypothyroidism causes symptoms like fatigue, dry skin, and hair thinning due to insufficient thyroid hormone production—however, it can be managed with diet, and if necessary, thyroid medications.
- Zinc deficiency may also cause hair loss and a characteristic rash. Treatment with zinc supplements can significantly improve hair growth and other symptoms.
- Medications, such as chemotherapy drugs, Accutane, and anti-seizure medications like valproic acid, are known to cause hair loss as a side effect. This type of hair loss is often reversible once the medication is stopped.
- Male pattern hair loss, or androgenic alopecia, is influenced by testosterone and genetic risk factors—which, contrary to popular belief, can come from either or both sides of the family. Early onset, especially before age 40, is linked to an increased risk of heart disease. However, effective treatments are available, and early intervention is beneficial.
- Female pattern hair loss is basically the same thing as male pattern hair loss (indeed, it is literally still androgenic alopecia), just a) almost always much less severe and b) with a gender-appropriate name. It affects up to 40% of women by age 50 and is characterized by thinning hair at the top of the head. It’s related to hormonal imbalances involving testosterone, such as those seen in PCOS and menopause, amongst other less common causes. Early treatment can be effective, and research is ongoing to develop more targeted therapies.
Dr. Siobhan Deshauer advises, if you’re experiencing hair loss, to monitor other symptoms too if applicable, take photos for tracking, and consult a doctor early for diagnosis and potential treatment.
For more on all of this plus visual illustrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
7 Principles of Becoming a Leader – by Riku Vuorenmaa
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We urge you to overlook the cliché cover art (we don’t know what they were thinking, going for the headless suited torso) because…
This one could be the best investment you make in your career this year! You may be wondering what the titular 7 principles are. We won’t keep you guessing; they are:
- Professional development: personal excellence, productivity, and time management
- Leadership development: mindset and essential leadership skills
- Personal development: your motivation, character, and confidence as a leader
- Career management: plan your career, get promoted and paid well
- Social skills & networking: work and connect with the right people
- Business- & company-understanding: the big picture
- Commitment: make the decision and commit to becoming a great leader
A lot of leadership books repeat the same old fluff that we’ve all read many times before… padded with a lot of lengthy personal anecdotes and generally editorializing fluff. Not so here!
While yes, this book does also cover some foundational things first, it’d be remiss not to. It also covers a whole (much deeper) range of related skills, with down-to-earth, brass tacks advice on putting them into practice.
This is the kind of book you will want to set as a recurring reminder in your phone, to re-read once a year, or whatever schedule seems sensible to you.
There aren’t many books we’d put in that category!
Pick Up Your Copy of the “7 Principles of Becoming a Leader” on Amazon Today!
Share This Post
Related Posts
-
Toasted Chick’n Mango Tacos
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tacos aren’t generally held up as the world’s healthiest food, but they can be! There’s so much going on in this dish today, healthwise, in a good way, that it’s hard to know where to start. But suffice it to say, these tacos are great for your gut, heart, blood sugars, and more.
You will need
For the chickpeas:
- 1 can chickpeas, drained
- 1 tbsp ras el-hanout*
- 1 tsp red pepper flakes
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
*You can easily make this yourself; following our recipe (linked above in the ingredients list) will be better than buying it ready-made, and if you have strong feelings about any of the ingredients, you can adjust per your preference.
For the tahini sauce:
- ⅓ cup tahini
- 2 tbsp apple cider vinegar
- 2 tbsp finely chopped fresh dill
- ¼ bulb garlic, minced
- 1 tsp red pepper flakes
- ½ tsp black pepper, coarse ground
It may seem like salt is conspicuous by its absence, but there is already enough in the chickpeas component; you do not want to overwhelm the dish. Trust us that enjoying these things together will be well-balanced and delicious as written.
For the mango relish:
- ½ mango, pitted, peeled, and cubed
- 2 tsp apple cider vinegar
- 2 tsp cilantro, finely chopped (substitute with parsley if you have the “cilantro tastes like soap” gene)
- 1 tsp red pepper flakes
For building the taco:
- Soft corn tortillas
- Handful of arugula
- 1 avocado, pitted, peeled, and sliced
- ½ red onion, sliced
Method
(we suggest you read everything at least once before doing anything)
1) Heat a sauté pan with a little olive oil in; add the chickpeas and then the rest of the ingredients from the chickpea section; cook for about 5 minutes, stirring frequently, and set aside.
2) Combine the tahini sauce ingredients in a small bowl, stirring in ¼ cup water, and set aside.
3) Combine the mango relish ingredients in a separate small bowl, and set aside. You can eat the other half of the mango if you like.
4) Lightly toast the tortillas in a dry skillet, or using a grill.
5) Assemble the tacos; we recommend the order: tortillas, arugula, avocado slices, chickpeas, mango relish, red onion slices, tahini sauce.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we hit all five today! Yay!
- An Apple (Cider Vinegar) A Day…
- Coconut vs Avocado – Which is Healthier?
- Lettuce vs Arugula – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Creamy Fortifying Cauliflower Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As delicious as it is super-easy to make, this one is full of protein, fiber, healthy fats, and some of the most health-giving spices around.
You will need
- 1 quart low-sodium vegetable stock
- 1 large cauliflower, cut into florets
- 1 large onion, finely chopped
- 2 cans cannellini (or other white) beans, drained and rinsed
- 1 cup raw cashews, soaked in hot water for at least 5 minutes, and drained (if allergic, substitute chickpeas)
- 1 bulb (yes, a whole bulb) garlic, roughly chopped
- 5 tbsp nutritional yeast
- 10 fresh sprigs of thyme (keep them whole!)
- 1 large fresh sprig of rosemary (keep this whole too!)
- zest of 1 lemon
- 1 tbsp red chili flakes
- 1 tbsp black pepper, coarse ground
- 1 tsp MSG or 2 tsp low-sodium salt
- ½ tsp ground turmeric
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Tightly tie up the sprigs of rosemary and thyme with kitchen twine (shining a bright light on it and asking it invasive questions is optional)
2) Heat some olive oil to a medium heat in your biggest sauté pan or similar. Add the onions, and cook for about 10 minutes, stirring as necessary. We are not trying to outright caramelize them here, but we do want them browned a little.
3) Add the garlic and cook for another 2 minutes, stirring frequently.
4) Add the vegetable stock, and stir, ensuring no onion is stuck to the base of the pan. Add the cauliflower, cashews, beans, nooch, pepper, turmeric, and MSG/salt, stirring to combine. Don’t worry if the cauliflower isn’t all submerged; it’ll be fine in a little while.
5) Add the herbs, submerging them in the soup (still tied up bouquet garni style).
6) Bring to a boil, reduce to a simmer and cook for 15–20 minutes; the cauliflower will be soft when it’s ready.
7) Remove the bouquet garni, and blend the soup until thick and creamy. You can do this with an immersion blender, but to get the smoothest soup, you’ll need to use a stand blender. Either ensure yours is safe for hot liquids, or else allow to cool, blend, and reheat later. This is important, as otherwise your blender could explode.
8) Serve, using the lemon zest and chili for the garnish:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Some Surprising Truths About Hunger And Satiety
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sesame Chocolate Fudge
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’d like a sweet treat without skyrocketing your blood sugars with, well, rocket fuel… Today’s recipe can help you enjoy a taste of decadence that’s not bad for your blood sugars, and good for your heart and brain.
You will need
- ½ cup sesame seeds
- ¼ cup cocoa powder
- 3 tbsp maple syrup
- 1 tbsp coconut oil (plus a little extra for the pan)
Method
(we suggest you read everything at least once before doing anything)
1) Lightly toast the sesame seeds in a pan until golden brown. Remove from the heat and allow to cool.
2) Put them in a food processor, and blend on full speed until they start to form a dough-like mixture. This may take a few minutes, so be patient. We recommend doing it in 30-second sessions with a 30-second rest between them, to avoiding overheating the motor.
3) Add the rest of the ingredients and blend to combine thoroughly—this should go easily now and only take 10 seconds or so, but judge it by eye.
4) Grease an 8″ square baking tin with a little coconut oil, and add the mixture, patting it down to fill the tin, making sure it is well-compressed.
5) Allow to chill in the fridge for 6 hours, until firm.
6) Turn the fudge out onto a chopping board, and cut into the size squares you want. Serve, or store in the fridge until ready to serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tasty Polyphenols For Your Heart & Brain
- Cacao vs Carob – Which is Healthier?
- Can Saturated Fats Be Healthy?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: