Resistance band Training – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those who’d like a full gym workout at home, without splashing out thousands on a home gym, resistance bands provide a lot of value. But how much value, really?
As James Atkinson demonstrates, there’s more exercise available than one might think.
Did you know that you can use the same band to strengthen your triceps as well as your biceps, for instance? and the same goes for your quadriceps and biceps femoris. And core strength? You bet.
The style here is not a sales pitch (though he does, at the end, offer extra resources if desired), but rather, instructional, and this book is in and of itself already a complete guide. With clear instructions and equally clear illustrations, you don’t need to spend a dime more (unless you don’t own a resistance band, in which case then yes, you will need one of those).
Bottom line: if you’d like to give your body the workout it deserves, this book is a potent resource.
Click here to check out Resistance Band Training, and get training!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anise vs Diabetes & Menopause
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What A Daily Gram Of Anise Can Do
Anise, specifically the seed of the plant, also called aniseed, is enjoyed for its licorice taste—as well as its medicinal properties.
Let’s see how well the science lives up to the folk medicine…
What medicinal properties does it claim?
The main contenders are:
- Reduces menopause symptoms
- Reduces blood sugar levels
- Reduces inflammation
Does it reduce menopause symptoms?
At least some of them! Including hot flashes and bone density loss. This seems to be due to the estrogenic-like activity of anethole, the active compound in anise that gives it these effects:
Estrogenic activity of isolated compounds and essential oils of Pimpinella species
1g of anise/day yielded a huge reduction in frequency and severity of hot flashes, compared to placebo*:
*you may be wondering what the placebo is for 1g of a substance that has a very distinctive taste. The researchers used capsules, with 3x330g as the dose, either anise seed or potato starch.
❝In the experimental group, the frequency and severity of hot flashes before the treatment were 4.21% and 56.21% and, after that, were 1.06% and 14.44% at the end of the fourth week respectively. No change was found in the frequency and severity of hot flashes in the control group. The frequency and severity of hot flashes was decreased during 4 weeks of follow up period. P. anisum is effective on the frequency and severity of hot flashes in postmenopausal women. ❞
See for yourself: The Study on the Effects of Pimpinella anisum on Relief and Recurrence of Menopausal Hot Flashes
As for bone mineral density, we couldn’t find a good study for anise, but we did find this one for fennel, which is a plant of the same family and also with the primary active compound anethole:
The Prophylactic Effect of Fennel Essential Oil on Experimental Osteoporosis
That was a rat study, though, so we’d like to see studies done with humans.
Summary on this one: it clearly helps against hot flashes (per the very convincing human study we listed above); it probably helps against bone mineral density loss.
Does it reduce blood sugar levels?
This one got a flurry of attention all so recently, on account of this research review:
Review on Anti-diabetic Research on Two Important Spices: Trachyspermum ammi and Pimpinella anisum
If you read this (and we do recommend reading it! It has a lot more information than we can squeeze in here!) one of the most interesting things about the in vivo anti-diabetic activity of anise was that while it did lower the fasting blood glucose levels, that wasn’t the only effect:
❝Over a course of 60 days, study participants were administered seed powders (5 g/d), which resulted in significant antioxidant, anti-diabetic, and hypolipidemic effects.
Notably, significant reductions in fasting blood glucose levels were observed. This intervention also elicited alterations in the lipid profile, LPO, lipoprotein levels, and the high-density lipoprotein (HDL) level.
Moreover, the serum levels of essential antioxidants, such as beta carotene, vitamin C, vitamin A, and vitamin E, which are typically decreased in diabetic patients, underwent a reversal.❞
That’s just one of the studies cited in that review (the comments lightly edited here for brevity), but it stands out, and you can read that study in its entirety (it’s well worth reading).
Rajeshwari et al, bless them, added a “tl;dr” at the top of their already concise abstract; their “tl;dr” reads:
❝Both the seeds significantly influenced almost all the parameters without any detrimental effects by virtue of a number of phytochemicals, vitamins and minerals present in the seeds having therapeutic effects.❞
Shortest answer: yes, yes it does
Does it fight inflammation?
This one’s quick and simple enough: yes it does; it’s full of antioxidants which thus also have an anti-inflammatory effect:
Review of Pharmacological Properties and Chemical Constituents of Pimpinella anisum
…which can also be used an essential oil, applied topically, to fight both pain and the inflammation that causes it—at least in rats and mice:
❝Indomethacin and etodolac were treated reference drugs for the anti-inflammatory activity. Aspirin and morphine hydrochloride were treated reference drugs for the analgesic activity. The results showed that fixed oil of P. anisum has an anti-inflammatory action more than etodolac and this effect was as strong as indomethacin. P. anisum induces analgesic effect comparable to that of 100 mg/kg Aspirin and 10 mg/kg morphine at 30 th min. of the study❞
Summary of this section:
- Aniseeds are a potent source of antioxidants, which fight inflammation.
- Anise essential oil is probably also useful as a topical anti-inflammatory and analgesic agent, but we’d like to see human tests to know for sure.
Is it safe?
For most people, enjoyed in moderation (e.g., within the dosage parameters described in the above studies), anise is safe. However:
- If you’re allergic to it, it won’t be safe
- Its estrogen-mimicking effects could cause problems if you have (or have a higher risk factor for) breast cancer, ovarian cancer, or endometriosis.
- For most men, the main concern is that it may lower sperm count.
Where to get it?
As ever, we don’t sell it (or anything else), but for your convenience, you can buy the seeds in bulk on Amazon, or in case you prefer it, here’s an example of it available as an essential oil.
Enjoy!
Share This Post
-
Human, Bird, or Dog Waste? Scientists Parsing Poop To Aid DC’s Forgotten River
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
KFF Health News Peggy Girshman reporting fellow Jackie Fortiér joined a boat tour to spotlight a review of microbes in the Anacostia River, a step toward making the river healthier and swimmable. The story was featured on WAMU’s “Health Hub” on Feb. 26.
On a bright October day, high schoolers from Francis L. Cardozo Education Campus piled into a boat on the Anacostia River in Washington, D.C. Most had never been on the water before.
Their guide, Trey Sherard of the Anacostia Riverkeeper, started the tour with a well-rehearsed safety talk. The nonprofit advocates for the protection of the river.
A boy with tousled black hair casually dipped his fingers in the water.
“Don’t touch it!” Sherard yelled.
Why was Sherard being so stern? Was it dangerously cold? Were there biting fish?
Because of the sewage.
“We get less sewage than we used to. Sewage is a code word for what?” Sherard asked the teenagers.
“Poop!” one student piped up.
“Human poop,” Sherard said. “Notice I didn’t say we get none. I said we get what? Less.”
Tours like this are designed to get young people interested in the river’s ecology, but it’s a fine line to tread — interacting with the water can make people sick. Because of the health risks, swimming hasn’t been legal in the Anacostia for more than half a century. The polluted water can cause gastrointestinal and respiratory illnesses, as well as eye, nose, and skin infections.
The river is the cleanest it’s been in years, according to environmental experts, but they still advise you not to take a dip in the Anacostia — not yet, at least.
About 40 million people in the U.S. live in a community with a combined sewer system, where wastewater and stormwater flow through the same pipes. When pipe capacities are reached after heavy rains, the overflow sends raw wastewater into the rivers instead of to a treatment plant.
Federal regulations, including sections of the Clean Water Act, require municipalities such as Washington to reduce at least 85% of this pollution or face steep fines.
To achieve compliance, Washington launched a $2.6 billion infrastructure project in 2011. DC Water’s Clean Rivers Project will eventually build multiple miles-long underground storage basins to capture stormwater and wastewater and pump it to treatment plants once heavy rains have subsided.
The Anacostia tunnel is the first of these storage basins to be completed. It can collect 190 million gallons of bacteria-laden wastewater for later treatment, said Moussa Wone, vice president of the Clean Rivers Project.
Climate change is causing more intense rainstorms in Washington, so even after construction is complete in 2030, Wone said, untreated stormwater will be discharged into the river, though much less frequently.
“On the Anacostia, we’re going to be reducing the frequency of overflows from 82 to two in an average year,” Wone said.
But while the Anacostia sewershed covers 176 square miles, he noted, only 17% is in Washington.
“The other 83% is outside the district,” Wone said. “We can do our part, but everybody else has to do their part also.”
Upstream in Maryland’s Montgomery and Prince George’s counties, miles of sewer lines are in the process of being upgraded to divert raw sewage to a treatment plant instead of the river.
The data shows that poop is a problem for river health — but knowing what kind of poop it is matters. Scientists monitor E. coli to indicate the presence of feces in river water, but since the bacteria live in the guts of most warm-blooded animals, the source is difficult to determine.
“Is it human feces? Or is it deer? Is it gulls’? Is it dogs’?” said Amy Sapkota, a professor of environmental and occupational health at the University of Maryland.
Bacterial levels can fluctuate across the river even without rainstorms. An Anacostia Riverkeeper report found that in 2023 just three of nine sites sampled along the Washington portion of the watershed had consistently low E. coli levels throughout the summer season.
Sapkota is heading a new bacterial monitoring program measuring the amount of E. coli that different animal species deposit along the river.
The team uses microbial source tracking to analyze samples of river water taken from different locations each month by volunteers. The molecular approach enables scientists to target specific gene sequences associated with fecal bacteria and determine whether the bacteria come from humans or wildlife. Microbial source tracking also measures fecal pollution levels by source.
“We can quantify the levels of different bacterial targets that may be coming from a human fecal source or an animal fecal source,” Sapkota said.
Her team expects to have preliminary results this year.
The health risk to humans from river water will never be zero, Sapkota said, but based on her team’s research, smart city planning and retooled infrastructure could lessen the level of harmful bacteria in the water.
“Let’s say that we’re finding that actually there’s a lot of deer fecal signatures in our results,” Sapkota said. “Maybe this points to the fact that we need more green buffers along the river that can help prevent fecal contaminants from wildlife from entering the river during stormwater events.”
Washington is hoping to recoup some of the cost of building green spaces and other river cleanup. In January, the office of D.C. Attorney General Brian Schwalb filed a lawsuit seeking unspecified damages from the federal government over decades of alleged pollution of the Anacostia River.
Brenda Lee Richardson, coordinator of the Anacostia Parks & Community Collaborative, said the efforts to cut down on trash and sewage are paying off. She sees a river on the mend, with more plant and animal life sprouting up.
“The ecosystem seems a lot greener,” she said. “There’s stuff in the river now that wasn’t there before.”
But any changes to the waterfront need to be done with residents of both sides of the river in mind, she said.
“We want there to be some sense of equity as it relates to who has access,” she said. “When I look at who is recreating, it’s not people who look like me.”
Richardson has lived for 40 years in Ward 8 — a predominantly Black area on the east side of the river whose residents are generally less affluent than those on the west side. She and her neighbors don’t consider the Anacostia a place to get out and play, she said.
As the water quality slowly improves, Richardson said, she hopes the Anacostia’s reputation is also rehabilitated. Even if it’s not safe to swim in, Richardson enjoys boating trips like the one with the Anacostia Riverkeeper.
“To see all those creatures along the way and the greenery. It was comforting,” she said. “So rather than take a pill to settle my nerves, I can just go down the river.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
The Exercises That Help Keep Breast Cancer At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For women, our lifetime risk of being diagnosed with breast cancer is about 1 in 7, before we take into account any added risk or protective factors.
For men, it’s more like 1 in 556, which again, is before taking into account any added risk or protective factors.
Here’s a good place to start on improving those odds: How To Triple Your Breast Cancer Survival Chances
And for that matter, check out: 8 Signs On Your Breast You Shouldn’t Ignore
And for those concerned (or even just curious) about the pros and cons of menopausal HRT when it comes to breast cancer:
The Hormone Therapy That Reduces Breast Cancer Risk & More ← this is actually very important to understand, as otherwise it’s easy to accidentally self-sabotage and increase one’s overall mortality risk
So, what’s this about exercise and breast cancer?
There are two things to focus on
No, not those.
Well, yes, those, but also: aerobic exercise and resistance training.
A research team (Dr. Alice Avancini et al.) analysed data from 22 randomized controlled trials (total n=968 participants) that investigated the effects of exercise on various pro-inflammatory biomarkers (mostly interleukin variants, but also c-reactive proteins) that are known to increase breast cancer reoccurrence risk.
What they found was:
❝Exercise induced small to large significant reductions in IL-6 (SMD = -0.85; 95% CI = -1.68 to -0.02; p = .05) and TNF-α (SMD = -0.40; 95% CI = -0.81 to 0.01; p = .05) and a trend for a decrease in CRP.
When stratifying by exercise mode, trends toward reduction in IL-6 and TNF-α were observed for combined exercise, whilst changes were not generally affected by exercise program duration❞
The “combined exercise” mentioned?
Aerobic exercise and resistance training.
This is important, because as regular 10almonds readers may remember…
What Your Metabolism Says About How Aggressive Breast Cancer Is Likely To Be For You ← this makes a huge difference to survival chances
So, this study’s findings are very consistent with that, because:
- Aerobic training increases cardiovascular fitness, improving metabolism
- Resistance training increases muscle mass, improving metabolism*
*because muscle “costs” calories to maintain, prompting an increase in metabolism, whereas fat prompts our metabolism to slow, to conserve energy to face the obvious food shortage that must be coming
See also: Stop Cancer 20 Years Ago
Want to learn more?
Here’s the best book we’ve read on breast cancer survival:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Share This Post
Related Posts
-
The Brain-Gut Highway: A Two-Way Street
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Brain-Gut Two-Way Highway
This is Dr. Emeran Mayer. He has the rather niche dual specialty of being a gastroenterologist and a neurologist. He has published over 353 peer reviewed scientific articles, and he’s a professor in the Departments of Medicine, Physiology, and Psychiatry at UCLA. Much of his work has been pioneering medical research into gut-brain interactions.
We know the brain and gut are connected. What else does he want us to know?
First, that it is a two-way interaction. It’s about 90% “gut tells the brain things”, but it’s also 10% “brain tells the gut things”, and that 10% can make more like a 20% difference, if for example we look at the swing between “brain using that 10% communication to tell gut to do things worse” or “brain using that 10% communication to tell gut to do things better”, vs the midpoint null hypothesis of “what the gut would be doing with no direction from the brain”.
For example, if we are experiencing unmanaged chronic stress, that is going to tell our gut to do things that had an evolutionary advantage 20,000–200,000 years ago. Those things will not help us now. We do not need cortisol highs and adrenal dumping because we ate a piece of bread while stressed.
Read more (by Dr. Mayer): The Stress That Evolution Has Not Prepared Us For
With this in mind, if we want to look after our gut, then we can start before we even put anything in our mouths. Dr. Mayer recommends managing stress, anxiety, and depression from the head downwards as well as from the gut upwards.
Here’s what we at 10almonds have written previously on how to manage those things:
- No-Frills, Evidence-Based Mindfulness
- How To Set Anxiety Aside
- The Mental Health First-Aid You’ll Hopefully Never Need
Do eat for gut health! Yes, even if…
Unsurprisingly, Dr. Mayer advocates for a gut-friendly, anti-inflammatory diet. We’ve written about these things before:
…but there’s just one problem:
For some people, such as with IBS, Crohn’s, and colitis, the Mediterranean diet that we (10almonds and Dr. Mayer) generally advocate for, is inaccessible. If you (if you have those conditions) eat as we describe, a combination of the fiber in many vegetables and the FODMAPs* in many fruits, will give you a very bad time indeed.
*Fermentable Oligo-, Di-, Monosaccharides And Polyols
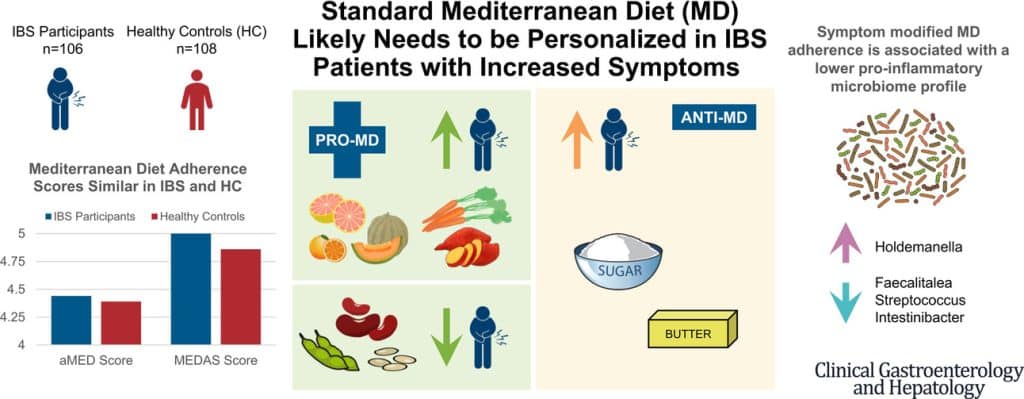
Dr. Mayer has the answer to this riddle, and he’s not just guessing; he and his team did science to it. In a study with hundreds of participants, he measured what happened with adherence (or not) to the Mediterranean diet (or modified Mediterranean diet) (or not), in participants with IBS (or not).
The results and conclusions from that study included:
❝Among IBS participants, a higher consumption of fruits, vegetables, sugar, and butter was associated with a greater severity of IBS symptoms. Multivariate analysis identified several Mediterranean Diet foods to be associated with increased IBS symptoms.
A higher adherence to symptom-modified Mediterranean Diet was associated with a lower abundance of potentially harmful Faecalitalea, Streptococcus, and Intestinibacter, and higher abundance of potentially beneficial Holdemanella from the Firmicutes phylum.
A standard Mediterranean Diet was not associated with IBS symptom severity, although certain Mediterranean Diet foods were associated with increased IBS symptoms. Our study suggests that standard Mediterranean Diet may not be suitable for all patients with IBS and likely needs to be personalized in those with increased symptoms.❞
In graphical form:
And if you’d like to read more about this (along with more details on which specific foods to include or exclude to get these results), you can do so…
- The study itself (full article): The Association Between a Mediterranean Diet and Symptoms of Irritable Bowel Syndrome
- Dr. Mayer’s blog (lay explanation): The Benefits of a Modified Mediterranean Diet for Irritable Bowel Syndrome
Want to know more?
Dr. Mayer offers many resources, including a blog, books, recipes, podcasts, and even a YouTube channel:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why scrapping the term ‘long COVID’ would be harmful for people with the condition
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The assertion from Queensland’s chief health officer John Gerrard that it’s time to stop using the term “long COVID” has made waves in Australian and international media over recent days.
Gerrard’s comments were related to new research from his team finding long-term symptoms of COVID are similar to the ongoing symptoms following other viral infections.
But there are limitations in this research, and problems with Gerrard’s argument we should drop the term “long COVID”. Here’s why.
A bit about the research
The study involved texting a survey to 5,112 Queensland adults who had experienced respiratory symptoms and had sought a PCR test in 2022. Respondents were contacted 12 months after the PCR test. Some had tested positive to COVID, while others had tested positive to influenza or had not tested positive to either disease.
Survey respondents were asked if they had experienced ongoing symptoms or any functional impairment over the previous year.
The study found people with respiratory symptoms can suffer long-term symptoms and impairment, regardless of whether they had COVID, influenza or another respiratory disease. These symptoms are often referred to as “post-viral”, as they linger after a viral infection.
Gerrard’s research will be presented in April at the European Congress of Clinical Microbiology and Infectious Diseases. It hasn’t been published in a peer-reviewed journal.
After the research was publicised last Friday, some experts highlighted flaws in the study design. For example, Steven Faux, a long COVID clinician interviewed on ABC’s television news, said the study excluded people who were hospitalised with COVID (therefore leaving out people who had the most severe symptoms). He also noted differing levels of vaccination against COVID and influenza may have influenced the findings.
In addition, Faux pointed out the survey would have excluded many older people who may not use smartphones.
The authors of the research have acknowledged some of these and other limitations in their study.
Ditching the term ‘long COVID’
Based on the research findings, Gerrard said in a press release:
We believe it is time to stop using terms like ‘long COVID’. They wrongly imply there is something unique and exceptional about longer term symptoms associated with this virus. This terminology can cause unnecessary fear, and in some cases, hypervigilance to longer symptoms that can impede recovery.
But Gerrard and his team’s findings cannot substantiate these assertions. Their survey only documented symptoms and impairment after respiratory infections. It didn’t ask people how fearful they were, or whether a term such as long COVID made them especially vigilant, for example.
Tens of thousands of Australians, and millions of people worldwide, have long COVID.
New Africa/ShutterstockIn discussing Gerrard’s conclusions about the terminology, Faux noted that even if only 3% of people develop long COVID (the survey found 3% of people had functional limitations after a year), this would equate to some 150,000 Queenslanders with the condition. He said:
To suggest that by not calling it long COVID you would be […] somehow helping those people not to focus on their symptoms is a curious conclusion from that study.
Another clinician and researcher, Philip Britton, criticised Gerrard’s conclusion about the language as “overstated and potentially unhelpful”. He noted the term “long COVID” is recognised by the World Health Organization as a valid description of the condition.
A cruel irony
An ever-growing body of research continues to show how COVID can cause harm to the body across organ systems and cells.
We know from the experiences shared by people with long COVID that the condition can be highly disabling, preventing them from engaging in study or paid work. It can also harm relationships with their friends, family members, and even their partners.
Despite all this, people with long COVID have often felt gaslit and unheard. When seeking treatment from health-care professionals, many people with long COVID report they have been dismissed or turned away.
Last Friday – the day Gerrard’s comments were made public – was actually International Long COVID Awareness Day, organised by activists to draw attention to the condition.
The response from people with long COVID was immediate. They shared their anger on social media about Gerrard’s comments, especially their timing, on a day designed to generate greater recognition for their illness.
Since the start of the COVID pandemic, patient communities have fought for recognition of the long-term symptoms many people faced.
The term “long COVID” was in fact coined by people suffering persistent symptoms after a COVID infection, who were seeking words to describe what they were going through.
The role people with long COVID have played in defining their condition and bringing medical and public attention to it demonstrates the possibilities of patient-led expertise. For decades, people with invisible or “silent” conditions such as ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) have had to fight ignorance from health-care professionals and stigma from others in their lives. They have often been told their disabling symptoms are psychosomatic.
Gerrard’s comments, and the media’s amplification of them, repudiates the term “long COVID” that community members have chosen to give their condition an identity and support each other. This is likely to cause distress and exacerbate feelings of abandonment.
Terminology matters
The words we use to describe illnesses and conditions are incredibly powerful. Naming a new condition is a step towards better recognition of people’s suffering, and hopefully, better diagnosis, health care, treatment and acceptance by others.
The term “long COVID” provides an easily understandable label to convey patients’ experiences to others. It is well known to the public. It has been routinely used in news media reporting and and in many reputable medical journal articles.
Most importantly, scrapping the label would further marginalise a large group of people with a chronic illness who have often been left to struggle behind closed doors.
Deborah Lupton, SHARP Professor, Vitalities Lab, Centre for Social Research in Health and Social Policy Centre, and the ARC Centre of Excellence for Automated Decision-Making and Society, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We’re the ‘allergy capital of the world’. But we don’t know why food allergies are so common in Australian children
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia has often been called the “allergy capital of the world”.
An estimated one in ten Australian children develop a food allergy in their first 12 months of life. Research has previously suggested food allergies are more common in infants in Australia than infants living in Europe, the United States or Asia.
So why are food allergies so common in Australia? We don’t know exactly – but local researchers are making progress in understanding childhood allergies all the time.
Miljan Zivkovic/Shutterstock What causes food allergies?
There are many different types of reactions to foods. When we refer to food allergies in this article, we’re talking about something called IgE-mediated food allergy. This type of allergy is caused by an immune response to a particular food.
Reactions can occur within minutes of eating the food and may include swelling of the face, lips or eyes, “hives” or welts on the skin, and vomiting. Signs of a severe allergic reaction (anaphylaxis) include difficulty breathing, swelling of the tongue, swelling in the throat, wheeze or persistent cough, difficulty talking or a hoarse voice, and persistent dizziness or collapse.
Recent results from Australia’s large, long-running food allergy study, HealthNuts, show one in ten one-year-olds have a food allergy, while around six in 100 children have a food allergy at age ten.
A food allergy can present with skin reactions. comzeal images/Shutterstock In Australia, the most common allergy-causing foods include eggs, peanuts, cow’s milk, shellfish (for example, prawn and lobster), fish, tree nuts (for example, walnuts and cashews), soybeans and wheat.
Allergies to foods like eggs, peanuts and cow’s milk often present for the first time in infancy, while allergies to fish and shellfish may be more common later in life. While most children will outgrow their allergies to eggs and milk, allergy to peanuts is more likely to be lifelong.
Findings from HealthNuts showed around three in ten children grew out of their peanut allergy by age six, compared to nine in ten children with an allergy to egg.
Are food allergies becoming more common?
Food allergies seem to have become more common in many countries around the world over recent decades. The exact timing of this increase is not clear, because in most countries food allergies were not well measured 40 or 50 years ago.
We don’t know exactly why food allergies are so common in Australia, or why we’re seeing a rise around the world, despite extensive research.
But possible reasons for rising allergies around the world include changes in the diets of mothers and infants and increasing sanitisation, leading to fewer infections as well as less exposure to “good” bacteria. In Australia, factors such as increasing vitamin D deficiency among infants and high levels of migration to the country could play a role.
In several Australian studies, children born in Australia to parents who were born in Asia have higher rates of food allergies compared to non-Asian children. On the other hand, children who were born in Asia and later migrated to Australia appear to have a lower risk of nut allergies.
Meanwhile, studies have shown that having pet dogs and siblings as a young child may reduce the risk of food allergies. This might be because having pet dogs and siblings increases contact with a range of bacteria and other organisms.
This evidence suggests that both genetics and environment play a role in the development of food allergies.
We also know that infants with eczema are more likely to develop a food allergy, and trials are underway to see whether this link can be broken.
Can I do anything to prevent food allergies in my kids?
One of the questions we are asked most often by parents is “can we do anything to prevent food allergies?”.
We now know introducing peanuts and eggs from around six months of age makes it less likely that an infant will develop an allergy to these foods. The Australasian Society of Clinical Immunology and Allergy introduced guidelines recommending giving common allergy-causing foods including peanut and egg in the first year of life in 2016.
Our research has shown this advice had excellent uptake and may have slowed the rise in food allergies in Australia. There was no increase in peanut allergies between 2007–11 to 2018–19.
Introducing other common allergy-causing foods in the first year of life may also be helpful, although the evidence for this is not as strong compared with peanuts and eggs.
Giving kids peanuts early can reduce the risk of a peanut allergy. Madame-Moustache/Shutterstock What next?
Unfortunately, some infants will develop food allergies even when the relevant foods are introduced in the first year of life. Managing food allergies can be a significant burden for children and families.
Several Australian trials are currently underway testing new strategies to prevent food allergies. A large trial, soon to be completed, is testing whether vitamin D supplements in infants reduce the risk of food allergies.
Another trial is testing whether the amount of eggs and peanuts a mother eats during pregnancy and breastfeeding has an influence on whether or not her baby will develop food allergies.
For most people with food allergies, avoidance of their known allergens remains the standard of care. Oral immunotherapy, which involves gradually increasing amounts of food allergen given under medical supervision, is beginning to be offered in some facilities around Australia. However, current oral immunotherapy methods have potential side effects (including allergic reactions), can involve high time commitment and cost, and don’t cure food allergies.
There is hope on the horizon for new food allergy treatments. Multiple clinical trials are underway around Australia aiming to develop safer and more effective treatments for people with food allergies.
Jennifer Koplin, Group Leader, Childhood Allergy & Epidemiology, The University of Queensland and Desalegn Markos Shifti, Postdoctoral Research Fellow, Child Health Research Centre, Faculty of Medicine, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: