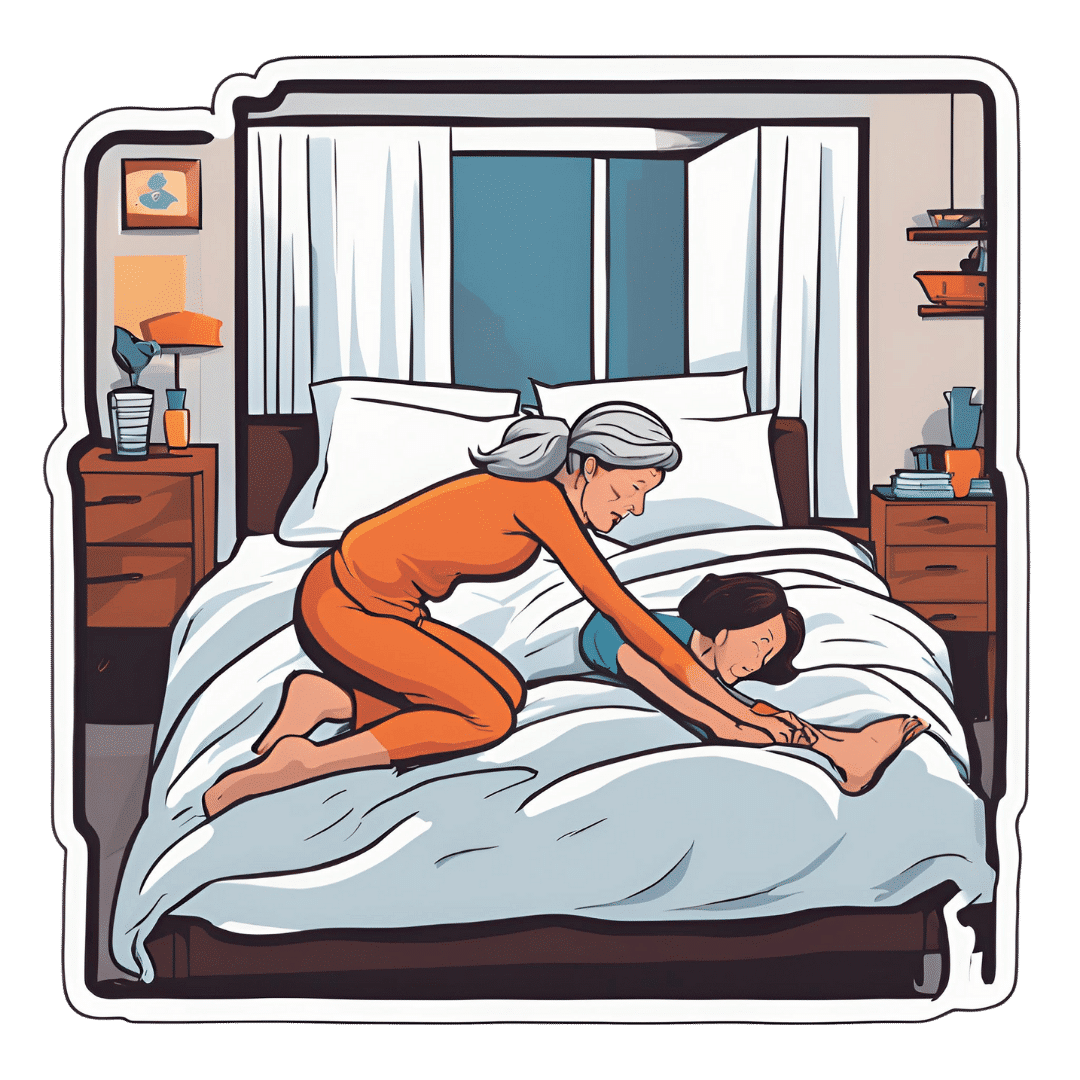
Over 50? Do These 3 Stretches Every Morning To Avoid Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Will Harlow, over-50s specialist physiotherapist, recommends these three stretches be done daily for cumulative benefits over time, especially if you have arthritis, stiff joints, or similar morning pain:
The good-morning routine
These stretches are designed for people with arthritis and stiff joints, but if you experience any extra pain, or are aware of having some musculoskeletal irregularity, do seek professional advice (such as from a local physiotherapist). Otherwise, the three stretches he recommends are:
Quad hip flexor stretch
This one is performed while lying on your side in bed:
- Bring the top leg up toward your body, grab the shin, and pull the leg backward to stretch.
- Feel the stretch in the front of the leg (quadriceps and hip flexor).
- Hold for 30 seconds and repeat on both sides.
- Use a towel or band if you can’t reach your shin.
Book-opener
This one helps improve mobility in the lower and mid-back:
- Lie on your side with arms at a 90-degree angle in front of your body.
- Roll backward, opening the top arm while keeping legs in place.
- Hold for 20–30 seconds or repeat the movement several times.
- Optionally, allow your head to rotate for a neck stretch.
Calf stretch with chest-opener
This one combines a calf and chest stretch:
- Stand in a lunged position, keeping the back leg straight and heel down for the calf stretch.
- Place hands behind your head, open elbows, and lift your head slightly for a chest stretch.
- Hold for 20–30 seconds, then switch legs.
For more on all the above plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
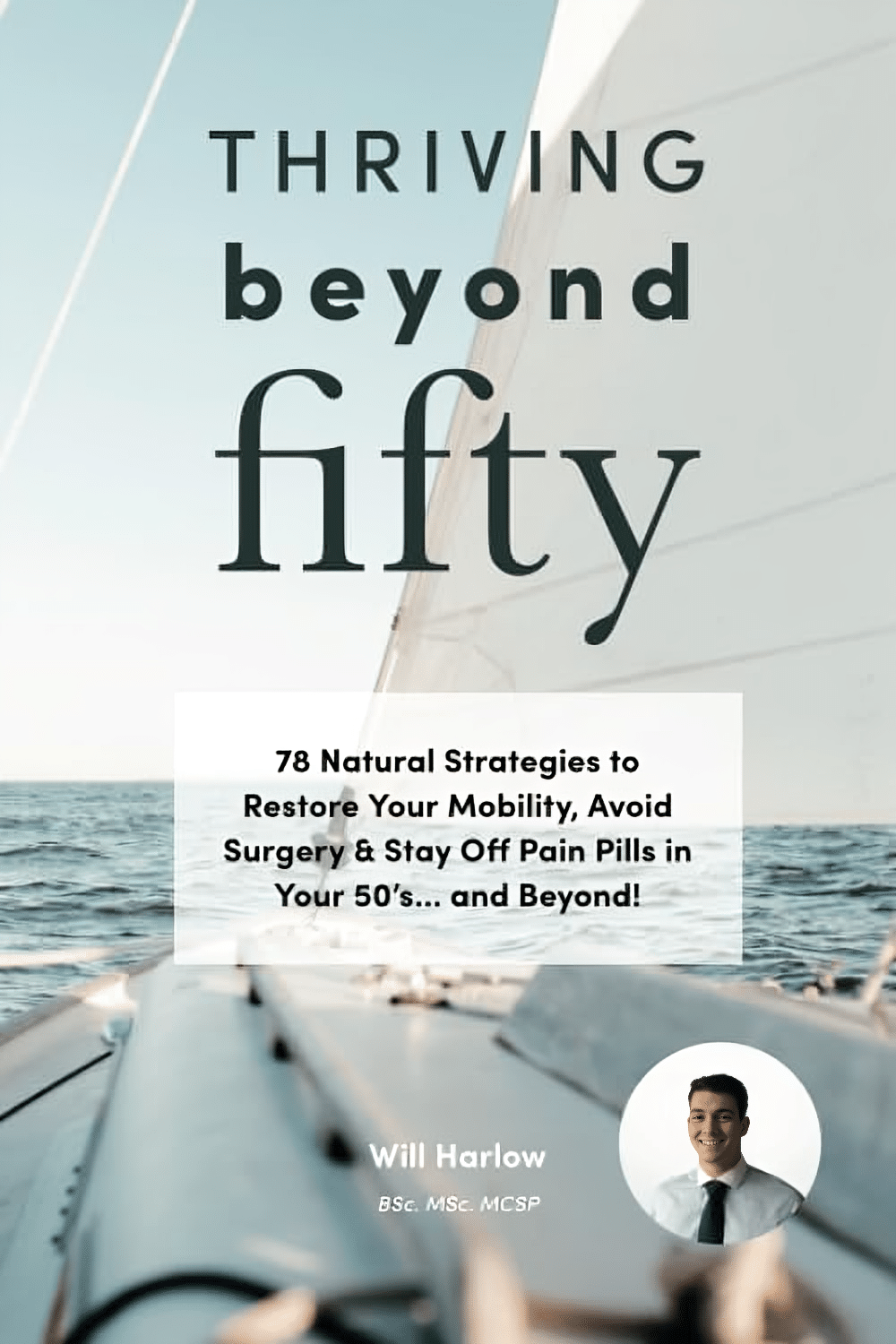
Thriving Beyond Fifty – by Will Harlow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve featured this author sometimes in our video section; he’s an over-50s specialist physiotherapist with a lot of very functional advice to offer.
In this book, Harlow focusses heavily on three things: mobility, strength, endurance.
You may not want to be a gymnast, powerlifter, or marathon-runner, but these things are important for us all to maintain to at least a fair degree:
- Mobility can be the difference between tweaking one’s shoulder getting something from a high shelf, or not
- Strength can be the difference between being able to get back up, or not
- Endurance can be the difference between coming back from a long day on your feet and thinking “that was a good day; I’m looking forward to tomorrow now”, or not
One of the greatest strengths of this book is its comprehensive troubleshooting aspect; if you have a weak spot, chances are this book has the remedy.
As for the style, it’s quite casual/conversational in tone, but without skimping on science and detail. It’s clear, explanatory, and helpful throughout.
Bottom line: if you’d like to maintain/improve mobility, strength, and endurance, then this book is a very recommendable resource.
Click here to check out Thriving Beyond Fifty, and keep thriving at every age!
Share This Post
-
The Other Circadian Rhythms
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked before about how circadian rhythm pertains not just to when it is ideal for us to sleep or be awake, but also at what times it is best to eat, exercise, and so forth:
The Circadian Rhythm: Far More Than Most People Know
Most people just know about the light consideration, per for example:
- How light can shift your mood and mental health, and
- How light tells you when to sleep, focus and poo
When your body parts clock on and off at the wrong time…
Now, new research has brought attention to how these things and more are governed by different physiological clocks within our bodies—and what this means for our health. In other words, if you are doing the various things at different times than you “should”, you will be training the different parts of your body (each with their independent clocks) to be on a different schedule, and so the different parts of your body will out of temporal sync with each other.
To put this in jet-lag terms: if your brain is in New York, while your heart is in Istanbul (not Constantinople) and your gut is in Tokyo, then this arrangement is not good for the health.
As for how it is not good for your health (i.e. the consequences) there’s still research to be done on some of the longer-term implications, but in the short term, one of the biggest effects is on our mood—most notably, increasing depression scores significantly.
And even more importantly, this is in the real world. That is to say, until quite recently, most data we had from studies on the circadian rhythm was from sleep clinic laboratories, which is great for RCTs but will always have as a limitation that someone sleeping in a lab is going to have some differences than someone sleeping in their own bed at home.
As the researchers said:
❝A critical step to addressing this is the noninvasive collection of physiological time-series data outside laboratory settings in large populations. Digital tools offer promise in this endeavor. Here, using wearable data, we first quantify the degrees of circadian disruption, both between different internal rhythms and between each internal rhythm and the sleep-wake cycle. Our analysis, based on over 50,000 days of data from over 800 first-year training physicians, reveals bidirectional links between digital markers of circadian disruption and mood both before and after they began shift work, while accounting for confounders such as demographic and geographic variables. We further validate this by finding clinically relevant changes in the 9-item Patient Health Questionnaire score.❞
Read in full: The real-world association between digital markers of circadian disruption and mental health risks
That questionnaire by the way sounds like an arbitrary thing they just made up, but the PHQ-9 (as it is known to its friends) is in fact the current intentional gold standard for measuring depression; we share it at the top of our article about depression, here:
The Mental Health First-Aid That You’ll Hopefully Never Need ← the test takes 2 minutes and you get immediate results
Want to know more?
For more about getting one’s entire self back into temporal sync (hey, wasn’t that the plot of a Star Trek episode?), sleep specialist Dr. Michael Breus wrote this excellent book that we reviewed a little while back:
Enjoy!
Share This Post
-
Garden Cress vs Watercress – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing garden cress to watercress, we picked the garden cress.
Why?
While watercress is (rightly!) popularly viewed as a superfood for its nutritional density, the garden variety actually outperforms it.
In terms of macros first, garden cress has more protein, carbs, and fiber, while also having the lower glycemic index. Not that anyone’s getting blood sugar spikes from eating any kind of cress, but still, by the numbers, this is a clear win on the whole for garden cress in the category of macros.
When it comes to vitamins, garden cress has a lot (tens of times) more of vitamins A, B2, B3, B6, B7, B9, C, K, and choline, while watercress has (slightly) more of vitamins B1, B5, and E. An easy win for garden cress.
In the category of minerals, garden cress has more copper, iron, magnesium, manganese, phosphorus, and potassium, while watercress has more calcium. Another clear win for garden cress.
Taking a quick peep at polyphenols in case there’s anything to offset the above, garden cress has 13x more kaempferol (13mg/100g to watercress’s 1mg/100g), and/but watercress, in its favor, has quercetin (at 4mg/100g), which garden cress doesn’t. So, we say this category is also a win for garden cress, but watercress has its merits too.
👆 Let’s clarify: those numbers are all very good, and garden cress’s 13mg/100g kaempferol is absurdly high; most such quotients of most edible plants are orders of magnitude smaller; not to shoehorn in another vegetable, but just to give an example, savoy cabbage, which won on nutritional density vs bok choi recently, has 0.26mg/100g kaempferol and 0.12mg/100g quercetin (which were already very respectable numbers), so you see the difference in cress’s exceptionally generous delivery of these polyphenols!
Adding up the sections makes for an overwhelming win for garden cress!
Want to learn more?
You might like to read:
Sprout Your Seeds, Grains, Beans, Etc ← cress is a great example of this!
Take care!
Share This Post
Related Posts
-
Apple vs Apricot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apple to apricot, we picked the apricot.
Why?
In terms of macros, there’s not too much between them; apples are higher in carbs and only a little higher in fiber, which disparity makes for a slightly higher glycemic index, but it’s not a big difference and they are both low GI foods.
Micronutrients, however, set these two fruits apart:
In the category of vitamins, apple is a tiny bit higher in choline, while apricots are higher in vitamins A, B1, B2, B3, B5, B6, B9, C, E, and K—in most cases, by quite large margins, too. All in all, a clear and easy win for apricots.
When it comes to minerals, apples are not higher in any minerals, while apricots are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. There’s simply no contest here.
In short, if an apple a day keeps the doctor away, then an apricot will give the doctor a nice weekend break somewhere.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Black Beans vs Fava Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing black beans to fava beans, we picked the black beans.
Why?
In terms of macros, black beans have more protein, carbs, and notably more fiber, the ratio of the latter two also being such that black beans enjoy the lower glycemic index (but both are still good). All in all, a clear win for black beans in this category.
In the category of vitamins, black beans have more of vitamins B1, B5, B6, E, K, and choline, while fava beans have more of vitamins A, B2, B3, B9, and C. That’s a marginal 6:5 win for black beans, before we take into account that they also have 43x as much vitamin E, which is quite a margin, while fava beans doesn’t have any similarly stand-out nutrient. So, another clear win for black beans.
When it comes to minerals, black beans have more calcium, copper, iron, magnesium, phosphorus, and potassium, while fava beans have more manganese, selenium, and zinc. Superficially this is a 6:3 win for black beans; it’s worth noting however that the margins aren’t high on either side in the case of any mineral, so this one’s closer than it looks. Still a win for black beans, though.
Adding up the sections makes for an easy overall win for black beans, but by all means, enjoy either or both—diversity is good!
Want to learn more?
You might like to read:
Eat More (Of This) For Lower Blood Pressure
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why do I need to take some medicines with food?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever been instructed to take your medicine with food and wondered why? Perhaps you’ve wondered if you really need to?
There are varied reasons, and sometimes complex science and chemistry, behind why you may be advised to take a medicine with food.
To complicate matters, some similar medicines need to be taken differently. The antibiotic amoxicillin with clavulanic acid (sold as Amoxil Duo Forte), for example, is recommended to be taken with food, while amoxicillin alone (sold as Amoxil), can be taken with or without food.
Different brands of the same medicine may also have different recommendations when it comes to taking it with food.
Ron Lach/Pexels Food impacts drug absorption
Food can affect how fast and how much a drug is absorbed into the body in up to 40% of medicines taken orally.
When you have food in your stomach, the makeup of the digestive juices change. This includes things like the fluid volume, thickness, pH (which becomes less acidic with food), surface tension, movement and how much salt is in your bile. These changes can impair or enhance drug absorption.
Eating a meal also delays how fast the contents of the stomach move into the small intestine – this is known as gastric emptying. The small intestine has a large surface area and rich blood supply – and this is the primary site of drug absorption.
Eating a meal with medicine will delay its onset. Farhad/Pexels Eating a larger meal, or one with lots of fibre, delays gastric emptying more than a smaller meal. Sometimes, health professionals will advise you to take a medicine with food, to help your body absorb the drug more slowly.
But if a drug can be taken with or without food – such as paracetamol – and you want it to work faster, take it on an empty stomach.
Food can make medicines more tolerable
Have you ever taken a medicine on an empty stomach and felt nauseated soon after? Some medicines can cause stomach upsets.
Metformin, for example, is a drug that reduces blood glucose and treats type 2 diabetes and polycystic ovary syndrome. It commonly causes gastrointestinal symptoms, with one in four users affected. To combat these side effects, it is generally recommended to be taken with food.
The same advice is given for corticosteroids (such as prednisolone/prednisone) and certain antibiotics (such as doxycycline).
Taking some medicines with food makes them more tolerable and improves the chance you’ll take it for the duration it’s prescribed.
Can food make medicines safer?
Ibuprofen is one of the most widely used over-the-counter medicines, with around one in five Australians reporting use within a two-week period.
While effective for pain and inflammation, ibuprofen can impact the stomach by inhibiting protective prostaglandins, increasing the risk of bleeding, ulceration and perforation with long-term use.
But there isn’t enough research to show taking ibuprofen with food reduces this risk.
Prolonged use may also affect kidney function, particularly in those with pre-existing conditions or dehydration.
The Australian Medicines Handbook, which guides prescribers about medicine usage and dosage, advises taking ibuprofen (sold as Nurofen and Advil) with a glass of water – or with a meal if it upsets your stomach.
If it doesn’t upset your stomach, ibuprofen can be taken with water. Tbel Abuseridze/Unsplash A systematic review published in 2015 found food delays the transit of ibuprofen to the small intestine and absorption, which delays therapeutic effect and the time before pain relief. It also found taking short courses of ibuprofen without food reduced the need for additional doses.
To reduce the risk of ibuprofen causing damage to your stomach or kidneys, use the lowest effective dose for the shortest duration, stay hydrated and avoid taking other non-steroidal anti-inflammatory medicines at the same time.
For people who use ibuprofen for prolonged periods and are at higher risk of gastrointestinal side effects (such as people with a history of ulcers or older adults), your prescriber may start you on a proton pump inhibitor, a medicine that reduces stomach acid and protects the stomach lining.
How much food do you need?
When you need to take a medicine with food, how much is enough?
Sometimes a full glass of milk or a couple of crackers may be enough, for medicines such as prednisone/prednisolone.
However, most head-to-head studies that compare the effects of a medicine “with food” and without, usually use a heavy meal to define “with food”. So, a cracker may not be enough, particularly for those with a sensitive stomach. A more substantial meal that includes a mix of fat, protein and carbohydrates is generally advised.
Your health professional can advise you on which of your medicines need to be taken with food and how they interact with your digestive system.
Mary Bushell, Clinical Associate Professor in Pharmacy, University of Canberra
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: