Top 5 Anti-Aging Exercises
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are some exercises that get called such things as “The King of Exercises!”, but how well-earned is that title and could it be that actually a mix of the top few is best?
The Exercises
While you don’t have to do all 5, your body will thank you if you are able to:
- Plank: strengthens most of the body, and can reduce back pain while improving posture.
- Squats: another core-strengthening exercise, this time with an emphasis on the lower body, which makes for strong foundations (including strong ankles, knees, and hips). Improves circulation also, and what’s good for circulation is good for the organs, including the brain!
- Push-ups: promotes very functional strength and fitness; great for alternating with planks, as despite their similar appearance, they work the abs and back more, respectively.
- Lunges: these are great for lower body strength and stability, and doing these greatly reduces the risk of falling.
- Glute Bridges: this nicely rounds off one’s core strength, increasing stability and improving posture, as well as reducing lower back pain too.
If the benefits of these seem to overlap a little, it’s because they do! But each does some things that the others don’t, so put together, they make for a very well-balanced workout.
For advice on how to do each of them, plus more about the muscles being used and the benefits, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Wholesome Threesome Protein Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This soup has two protein– and fiber-rich pseudo-grains, one real wholegrain, and nutrient-dense cashews for yet even more protein, and all of the above are full of many great vitamins and minerals. All in all, a well-balanced and highly-nutritious light meal!
You will need
- ⅓ cup quinoa
- ⅓ cup green lentils
- ⅓ cup wholegrain rice
- 5 cups low-sodium vegetable stock (ideally you made this yourself from offcuts of vegetables, but failing that, low-sodium stock cubes can be bought in most large supermarkets)
- ¼ cup cashews
- 1 tbsp dried thyme
- 1 tbsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
Optional topping:
- ⅓ cup pine nuts
- ⅓ cup finely chopped fresh mint leaves
- 2 tbsp coconut oil
Method
(we suggest you read everything at least once before doing anything)
1) Rinse the quinoa, lentils, and rice.
2) Boil 4 cups of the stock and add the grains and seasonings (MSG/salt, pepper, thyme); simmer for about 25 minutes.
3) Blend the cashews with the other cup of vegetable stock, until smooth. Add the cashew mixture to the soup, stirring it in, and allow to simmer for another 5 minutes.
4) Heat the coconut oil in a skillet and add the pine nuts, stirring until they are golden brown.
5) Serve the soup into bowls, adding the mint and pine nuts to each.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Give Us This Day Our Daily Dozen
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Why You Should Diversify Your Nuts!
Take care!
Share This Post
-
Creamy Fortifying Cauliflower Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As delicious as it is super-easy to make, this one is full of protein, fiber, healthy fats, and some of the most health-giving spices around.
You will need
- 1 quart low-sodium vegetable stock
- 1 large cauliflower, cut into florets
- 1 large onion, finely chopped
- 2 cans cannellini (or other white) beans, drained and rinsed
- 1 cup raw cashews, soaked in hot water for at least 5 minutes, and drained (if allergic, substitute chickpeas)
- 1 bulb (yes, a whole bulb) garlic, roughly chopped
- 5 tbsp nutritional yeast
- 10 fresh sprigs of thyme (keep them whole!)
- 1 large fresh sprig of rosemary (keep this whole too!)
- zest of 1 lemon
- 1 tbsp red chili flakes
- 1 tbsp black pepper, coarse ground
- 1 tsp MSG or 2 tsp low-sodium salt
- ½ tsp ground turmeric
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Tightly tie up the sprigs of rosemary and thyme with kitchen twine (shining a bright light on it and asking it invasive questions is optional)
2) Heat some olive oil to a medium heat in your biggest sauté pan or similar. Add the onions, and cook for about 10 minutes, stirring as necessary. We are not trying to outright caramelize them here, but we do want them browned a little.
3) Add the garlic and cook for another 2 minutes, stirring frequently.
4) Add the vegetable stock, and stir, ensuring no onion is stuck to the base of the pan. Add the cauliflower, cashews, beans, nooch, pepper, turmeric, and MSG/salt, stirring to combine. Don’t worry if the cauliflower isn’t all submerged; it’ll be fine in a little while.
5) Add the herbs, submerging them in the soup (still tied up bouquet garni style).
6) Bring to a boil, reduce to a simmer and cook for 15–20 minutes; the cauliflower will be soft when it’s ready.
7) Remove the bouquet garni, and blend the soup until thick and creamy. You can do this with an immersion blender, but to get the smoothest soup, you’ll need to use a stand blender. Either ensure yours is safe for hot liquids, or else allow to cool, blend, and reheat later. This is important, as otherwise your blender could explode.
8) Serve, using the lemon zest and chili for the garnish:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Some Surprising Truths About Hunger And Satiety
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
7 Minutes, 30 Days, Honest Review: How Does The 7-Minute Workout Stack Up?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those who don’t like exercising, “the 7-minute workout” (developed by exercise scientists Chris Jordan and Bret Klika) has a lot of allure. After all, it’s just 7 minutes and then you’re done! But how well does it stand up, outside of the lab?
Down-to-Earth
Business Insider’s Kelly Reilly is not a health guru, and here he reviews the workout for us, so that we can get a real view of what it’s really like in the real world. What does he want us to know?
- It’s basically an optimized kind of circuit training, and can be done with no equipment aside from a floor, a wall, and a chair
- It’s one exercise for 30 seconds, then 10 seconds rest, then onto the next exercise
- He found it a lot easier to find the motivation to do this, than go to the gym. After all “it’s just 7 minutes” is less offputting than getting in the car, driving someplace, using public facilities, driving back, etc. Instead, it’s just him in the comfort of his home
- The exercise did make him sweat and felt like a “real” workout in that regard
- He didn’t like missing out on training his biceps, though, since there are no pulling movements
- He lost a little weight over the course of the month, though that wasn’t his main goal (and indeed, he was not eating healthily)
- He did feel better each day after working out, and at the end of the month, he enjoyed feeling self-confident in a tux that now fitted him better than it did before
For more details, his own words, and down-to-earth visuals of what this looked like for him, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Want to know more? Check out…
- How To Do HIIT (Without Wrecking Your Body)
- HIIT, But Make It HIRT ← this is about high-intensity resistance training!
Take care!
Share This Post
Related Posts
-
What Curiosity Really Kills
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Curiosity Kills The Neurodegeneration
Of the seven things that Leonardo da Vinci considered most important for developing and maintaining the mind, number one on his list was curiosity, and we’re going to be focussing on that today.
In case you are curious about what seven things made Leonardo’s* list, they were:
- Curiosità: an insatiably curious approach to life and an unrelenting quest for continuous learning
- Dimostrazione: a commitment to test knowledge through experience, persistence, and a willingness to learn from mistakes
- Sensazione: the continual refinement of the senses, especially sight, as a means to enliven experience
- Sfumato: (lit: “gone up in smoke”) a willingness to embrace ambiguity, paradox, and uncertainty
- Arte/Scienza: the curated balance of art and science, imagination and logic
- Corporalità: the cultivation of physical grace, ambidexterity, and fitness
- Connessione: a recognition of and appreciation for the interconnectedness of phenomena (systems-based thinking)
*In case you are curious why we wrote “Leonardo” and not “da Vinci” as per our usual convention of shortening names to last names, da Vinci is not technically a name, in much the same way as “of Nazareth” was not a name.
You can read more about all 7 of these in a book that we’ve reviewed previously:
How to Think Like Leonardo da Vinci: Seven Steps to Genius Every Day – by Michael J. Gelb
But for now, let’s take on “curiosity”!
If you need an extra reason to focus on growing and nurturing your curiosity, it was also #1 of Dr. Daniel Levitin’s list of…
The Five Keys Of Aging Healthily
…and that’s from a modern-day neuroscientist whose research focuses on aging, the brain, health, productivity, and creativity.
But how do we foster curiosity in the age of Google?
Curiosity is like a muscle: use it or lose it
While it’s true that many things can be Googled to satisfy one’s curiosity in an instant…
- do you? It’s only useful if you do use it
- is the top result on Google reliable?
- there are many things that aren’t available there
In short: douse “fast
foodinformation” sources, but don’t rely on them! Not just for the sake of having correct information, but also: for the actual brain benefits which is what we are aiming for here with today’s article.If you want the best brain benefits, dive in, and go deep
Here at 10almonds we often present superficial information, with links to deeper information (often: scholarly articles). We do this because a) there’s only so much we can fit in our articles and b) we know you only have so much time available, and/but may choose to dive deeper.
Think of it in layers, e.g:
- Collagen is good for joints and bones
- Collagen is a protein made of these amino acids that also requires these vitamins and minerals to be present in order to formulate it
- Those amino acids are needed in these quantities, of which this particular one is usually the weakest link that might need supplementing, and those vitamins and minerals need to be within this period of time, but not these ones at the exact same time, or else it will disrupt the process of collagen synthesis
(in case you’re curious, we covered this here and here and offered a very good, very in-depth book about it here)
Now, this doesn’t mean that to have a healthy brain you need to have the equivalent knowledge of an anatomy & physiology degree, but it is good to have that level of curiosity in at least some areas of your life—and the more, the better.
Top tips for developing a habit of curiosity
As you probably know, most of our endeavors as humans go best when they are habits:
How To Really Pick Up (And Keep!) Those Habits
And as for specifically building a habit of curiosity:
- Make a deal with yourself that when someone is excited to tell you what they know about something (no matter whether it is your grandkid, or the socially awkward nerd at a party, or whoever), listen and learn, no matter the topic.
- Learn at least one language other than your native language (presumably English for most of our readers). Not only does learning a language convey a lot of brain benefits of its own, but also, it is almost impossible to separate language learning from cultural learning, and so you will learn a lot about another culture too, and have whole new worlds opened up to you. Again, more is better, but one second language is already a lot better than none.
- Make a regular habit of going to your local library, and picking out a non-fiction book to take home and read. This has an advantage over a bookshop, by the way (and not just that the library is free): since library books must be returned, you will keep going back, and build a habit of taking out books.
- Pick a skill that you’d like to make into a fully-fledged hobby, and commit to continually learning as much about it as you can. We already covered language-learning above, but others might include: gardening (perhaps a specific kind), cooking (perhaps a specific kind), needlecraft (perhaps a specific kind), dance (perhaps a specific kind). You could learn a musical instrument. Or it could be something very directly useful, like learning to be a first responder in case of emergencies, and committing to continually learning more about it (because there is always more to learn).
And when it comes to the above choices… Pick things that excite you, regardless of how practical or not they are. Because that stimulation that keeps on driving you? That’s what keeps your brain active, healthy, and sharp.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tranquility by Tuesday?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
I Know How She Does It: How Successful Women Make The Most of Their Time
This is Laura Vanderkam, author of “Tranquility By Tuesday” (amongst other books). Her “thing” is spending more time on what’s important, and less on what isn’t. Sounds simple, but she’s made a career out of it, so condensed here for you are…
Laura’s 7 Keys To Productivity
Key One: Plan your weeks on Fridays
You don’t want your Monday morning to be a “James Bond intro” (where everything is already in action and you’re just along for the ride, trying to figure out what’s going on). So, take some time last thing each Friday, to plan ahead for the following week!
Key Two: Measure what matters
Whatever that means to you. Laura tracks her use of time in half-hour blocks, and likes keeping track of streaks. For her, that means running daily and keeping a log of it. She also keeps track of the books she reads. For someone else it could be music practice, or a Duolingo streak, or eating fruit each day.
On which note…
“Dr. Greger’s Daily Dozen” is simpler than most nutrition trackers (where you must search for everything you eat, or scan barcodes for all ingredients).
Instead, it keeps track of whether you are having certain key health-giving foods often enough to maintain good health.
We might feature his method in a future edition of 10almonds, but for now, check the app out for yourself here:
Get Dr. Greger’s Daily Dozen on iOS / Get Dr. Greger’s Daily Dozen on Android
Dr. Greger’s Daily Dozen @ Nutrition Facts
Key Three: Figure out 2–3 “anchor” events for the weekend
Otherwise, it can become a bit of a haze and on Monday you find yourself thinking “where did the weekend go?”. So, plan some stuff! It doesn’t have to be anything out-of-this-world, just something that you can look forward to in advance and remember afterwards. It could be a meal out with your family, or a session doing some gardening, or a romantic night in with your partner. Whatever makes your life “living” and not passing you by!
Key Four: Tackle the toughest work first
You’ve probably heard about “swallowing frogs”. If not, there are various versions, usually attributed to Mark Twain.
Here’s one:
“If it’s your job to eat a frog, it’s best to do it first thing in the morning. And if it’s your job to eat two frogs, it’s best to eat the biggest one first.”
Top Productivity App “ToDoist” has an option for this, by the way!
Laura’s key advice here is: get the hard stuff done now! Before you get distracted or tired and postpone it to tomorrow (and then lather rinse repeat, so it never gets done)
10almonds Tip:
“But what if something’s really important but not as pressing as some less important, but more urgent tasks?”
Simple!
Set a timer (we love the Pomodoro method, by the way) and do one burst of the important-but-not-urgent task first. Then you can get to the more urgent stuff.
Repeat each day until the important-but-not-urgent task is done!
The 10almonds Team
Key Five: Use bits of time well
If, like many of us, you’ve a neverending “to read” list, use the 5–10 minute breaks that get enforced upon us periodically through the day!
- Use those few minutes before a meeting/phonecall!
- Use the time you spend waiting for public transport or riding on it!
- Use the time you spent waiting for a family member to finish doing a thing!
All those 5–10 minute bits soon add up… You might as well spend that time reading something you know will add value to your life, rather than browsing social media, for example.
Key Six: Make very short daily to-do lists
By “short”, Laura considers this “under 10 items”. Do this as the last part of your working day, ready for tomorrow. Not at bedtime! Bedtime is for winding down, not winding up
Key Seven: Have a bedtime
Laura shoots for 10:30pm, but whatever works for you and your morning responsibilities. Your morning responsibilities aren’t tied to a specific time? Lucky you, but try to keep a bedtime anyway. Otherwise, your daily rhythm can end up sliding around the clock, especially if you work from home!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
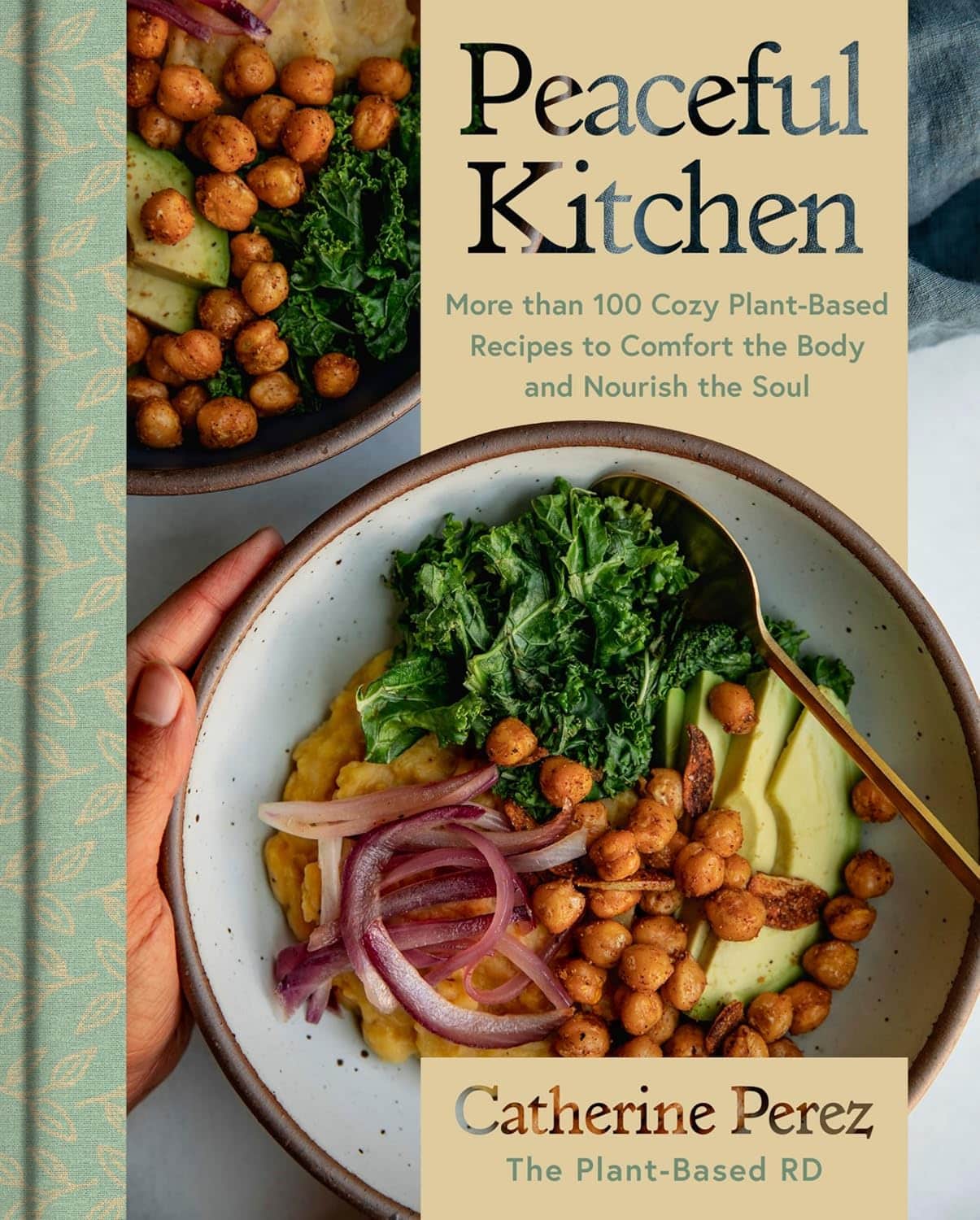
Peaceful Kitchen – by Catherine Perez
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a keen cook and Registered Dietician with a Master’s in same, covers the basics of the science of nutrition as relevant to her recipes, but first and foremost this is not a science textbook—it’s a cookbook, and its pages contain more love for the art than citations for the (perfectly respectable) science.
Mexican and Dominican cuisine are the main influences in this book, but there are dishes from around the world too.
The recipes themselves are… Comparable in difficulty to the things we often feature in our recipes section here at 10almonds. They’re probably not winning any restaurants Michelin stars, but they’re not exactly student survival recipes either. They’re made from mostly non-obscure whole foods, nutritionally-dense ingredients at that, with minimal processed foods involved.
That said, she does take a “add, don’t subtract” approach to nutrition, i.e. focussing more on adding in diversity of plants than on “don’t eat this; don’t eat that” mandates.
If there’s any criticism to be levelled at the book, it’s that in most cases we’d multiply the spices severalfold, but that’s not a big problem as readers can always judge that individually; she’s given the basic information of which spices in which proportions, which is the key knowledge.
Bottom line: if you’re looking to expand your plant-based cooking repertoire, this one is a fine choice.
Click here to check out Peaceful Kitchen, and try some new things!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: