What you need to know about endometriosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Endometriosis affects one in 10 people with a uterus who are of reproductive age. This condition occurs when tissue similar to the endometrium—the inner lining of the uterus—grows on organs outside of the uterus, causing severe pain that impacts patients’ quality of life.
Read on to learn more about endometriosis: What it is, how it’s diagnosed and treated, where patients can find support, and more.
What is endometriosis, and what areas of the body can it affect?
The endometrium is the tissue that lines the inside of the uterus and sheds during each menstrual cycle. Endometriosis occurs when endometrial-like tissue grows outside of the uterus.
This tissue can typically grow in the pelvic region and may affect the outside of the uterus, fallopian tubes, ovaries, vagina, bladder, intestines, and rectum. It has also been observed outside of the pelvis on the lungs, spleen, liver, and brain.
What are the symptoms?
Symptoms may include pelvic pain and cramping before or during menstrual periods, heavy menstrual bleeding, bleeding or spotting between periods, pain with bowel movements or urination, pain during or after sex or orgasm, fatigue, nausea, bloating, and infertility.
The pain associated with this condition has been linked to depression, anxiety, and eating disorders. A meta-analysis published in 2019 found that more than two-thirds of patients with endometriosis report psychological stress due to their symptoms.
Who is at risk?
Endometriosis most commonly occurs in people with a uterus between the ages of 25 and 40, but it can also affect pre-pubescent and post-menopausal people. In rare cases, it has been documented in cisgender men.
Scientists still don’t know what causes the endometrial-like tissue to grow, but research shows that people with a family history of endometriosis are at a higher risk of developing the condition. Other risk factors include early menstruation, short menstrual cycles, high estrogen, low body mass, and starting menopause at an older age.
There is no known way to prevent endometriosis.
How does endometriosis affect fertility?
Up to 50 percent of people with endometriosis may struggle to get pregnant. Adhesions and scarring on the fallopian tubes and ovaries as well as changes in hormones and egg quality can contribute to infertility.
Additionally, when patients with this condition are able to conceive, they may face an increased risk of pregnancy complications and adverse pregnancy outcomes.
Treating endometriosis, taking fertility medications, and using assistive reproductive technology like in vitro fertilization can improve fertility outcomes.
How is endometriosis diagnosed, and what challenges do patients face when seeking a diagnosis?
A doctor may perform a pelvic exam and request an ultrasound or MRI. These exams and tests help identify cysts or other unusual tissue that may indicate endometriosis.
Endometriosis can only be confirmed through a surgical laparoscopy (although less-invasive diagnostic tests are currently in development). During the procedure, a surgeon makes a small cut in the patient’s abdomen and inserts a thin scope to check for endometrial-like tissue outside of the uterus. The surgeon may take a biopsy, or a small sample, and send it to a lab.
It takes an average of 10 years for patients to be properly diagnosed with endometriosis. A 2023 U.K. study found that stigma around menstrual health, the normalization of menstrual pain, and a lack of medical training about the condition contribute to delayed diagnoses. Patients also report that health care providers dismiss their pain and attribute their symptoms to psychological factors.
Additionally, endometriosis has typically been studied among white, cisgender populations. Data on the prevalence of endometriosis among people of color and transgender people is limited, so patients in those communities face additional barriers to care.
What treatment options are available?
Treatment for endometriosis depends on its severity. Management options include:
- Over-the-counter pain medication to alleviate pelvic pain
- Hormonal birth control to facilitate lighter, less painful periods
- Hormonal medications such as gonadotropin-releasing hormone (GnRH) or danazol, which stop the production of hormones that cause menstruation
- Progestin therapy, which may stop the growth of endometriosis tissue
- Aromatase inhibitors, which reduce estrogen
In some cases, a doctor may perform a laparoscopic surgery to remove endometrial-like tissue.
Depending on the severity of the patient’s symptoms and scar tissue, some doctors may also recommend a hysterectomy, or the removal of the uterus, to alleviate symptoms. Doctors may also recommend removing the patient’s ovaries, inducing early menopause to potentially improve pain.
Where can people living with endometriosis find support?
Given the documented mental health impacts of endometriosis, patients with this condition may benefit from therapy, as well as support from others living with the same symptoms. Some peer support organizations include:
- Endometriosis Coalition Patient Support Group (virtual)
- MyEndometriosisTeam (virtual)
- Endo Black, Inc. (Washington, D.C.)
- endoQueer (virtual)
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 7 Approaches To Pain Management
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More Than One Way To Kill Pain
This is Dr. Deepak Ravindran (MD, FRCA. FFPMRCA, EDRA. FIPP, DMSMed). He has decades of experience and is a specialist in acute and chronic pain management, anesthesia, musculoskeletal medicine, and lifestyle medicine.
A quick catch-up, first:
We’ve written about chronic pain management before:
Managing Chronic Pain (Realistically!)
As well as:
Science-Based Alternative Pain Relief
Dr. Ravindran’s approach
Dr. Ravindran takes a “trauma-informed care” approach to his professional practice, and recommends the same for others.
In a nutshell, this means starting from a position of not “what’s wrong with you?”, but rather “what happened to you?”.
This seemingly subtle shift is important, because it means actually dealing with a person’s issues, instead of “take one of these and call my secretary next month”. Read more:
Pain itself can be something of a many-headed hydra. Dr. Ravindran’s approach is equally many-headed; specifically, he has a 7-point plan:
Medications
Dr. Ravindran sees painkillers (and a collection of other drugs, like antidepressants and muscle relaxants) as a potential means to an end worth exploring, but he doesn’t expect them to be the best choice for everyone, and nor does he expect them to be a cure-all. Neither should we. He also advises being mindful of the drawbacks and potential complications of these drugs, too.
Interventions
Sometimes, surgery is the right choice. Sometimes it isn’t. Often, it will change a life—one way or the other. Similar to with medications, Dr. Ravindran is very averse to a “one size fits all” approach here. See also:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Neuroscience and stress management
Often a lot of the distress of pain is not just the pain itself, but the fear associated with it. Will it get worse if I move wrong or eat the wrong thing? How long will it last? Will it ever get better? Will it get worse if I do nothing?. Dr. Ravindran advises tackling this, with the same level of importance as the pain itself. Here’s a good start:
Stress, And Building Psychological Resilience
Diet and the microbiome
Many chronic illnesses are heavily influenced by this, and Dr. Ravindran’s respect for lifestyle medicine comes into play here. While diet might not fix all our ills, it certainly can stop things from being a lot worse. Beyond the obvious “eat healthily” (Mediterranean diet being a good starting point for most people), he also advises doing elimination tests where appropriate, to screen out potential flare-up triggers. You also might consider:
Four Ways To Upgrade The Mediterranean Diet
Sleep
“Get good sleep” is easy advice for those who are not in agonizing pain that sometimes gets worse from staying in the same position for too long. Nevertheless, it is important, and foundational to good health. So it’s important to explore—whatever limitations one might realistically have—what can be done to improve it.
If you can only sleep for a short while at a time, you may get benefit from this previous main feature of ours:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Exercise and movement
The trick here is to move little and often; without overdoing it, but without permitting loss of mobility either. See also:
The Doctor Who Wants Us To Exercise Less, And Move More
Therapies of the mind and body
This is about taking a holistic approach to one’s wellness. In Dr. Ravindran’s words:
❝Mind-body therapies are often an extremely sensitive topic about which people hold very strong opinions and sometimes irrational beliefs.
Some, like reiki and spiritual therapy and homeopathy, have hardly any scientific evidence to back them up, while others like yoga, hypnosis, and meditation/mindfulness are mainstream techniques with many studies showing the benefits, but they all work for certain patients.❞
In other words: evidence-based is surely the best starting point, but if you feel inclined to try something else and it works for you, then it works for you. And that’s a win.
Want to know more?
You might like his book…
The Pain-Free Mindset: 7 Steps to Taking Control and Overcoming Chronic Pain
He also has a blog and a podcast.
Take care!
Share This Post
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Share This Post
-
How Tight Are Your Hips? Test (And Fix!) With This
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Upon surveying over half a million people; hips were the most common area for stiffness and lack of mobility. So, what to do about it?
This test don’t lie
With 17 muscles contributing to hip function (“hip flexors” being the name for this group of 17 muscles, not specific muscle), it’s important to figure out which ones are tight, and if indeed it really is the hip flexors at all, or if it could be, as it often is, actually the tensor fasciae latae (TFL) muscle of the thigh. If it turns out to be both, well, that’s unfortunate but the good news is, now you’ll know and can start fixing from all the necessary angles.
Diagnostic test for tight hip flexors (Thomas Test):
- Use a sturdy, elevated surface (e.g. table or counter—not a bed or couch, unless there is perchance room to swing your legs without them touching the floor).
- Sit at the edge, lie back, and pull both knees to your chest.
- Return one leg back down until the thigh is perpendicular to the table.
- Let the other leg dangle off the edge to assess flexibility.
Observations from the test:
- Thigh contact: is the back of your thigh touching the table?
- Knee angle: is your knee bent at roughly 80° or straighter?
- Thigh rotation: does the thigh roll outward?
Interpreting results:
- If your thigh contacts the surface and the knee is bent at around 80°, hip mobility is good.
- If your thigh doesn’t touch or knee is too straight, hip flexor tightness is present.
- If your thigh rolls outwards from your midline, that indicates tightness in the TFL muscle of the thigh.
Three best hip flexor stretches:
- Kneeling lunge stretch:
- Hips above the knee, tuck tailbone, engage glutes, press hips forward, reach arm up with a slight side bend.
- Seated hip lift stretch:
- Sit with feet hip-width apart, hands behind shoulders, lift hips, step one foot back, tuck tailbone, point knee away.
- Sofa stretch:
- Kneel with one shin against a couch/wall, other foot forward in lunge, tuck tailbone, press hips forward, lift torso.
It’s recommended to how each stretch for 30 seconds on each side.
For more on all of the above, and visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
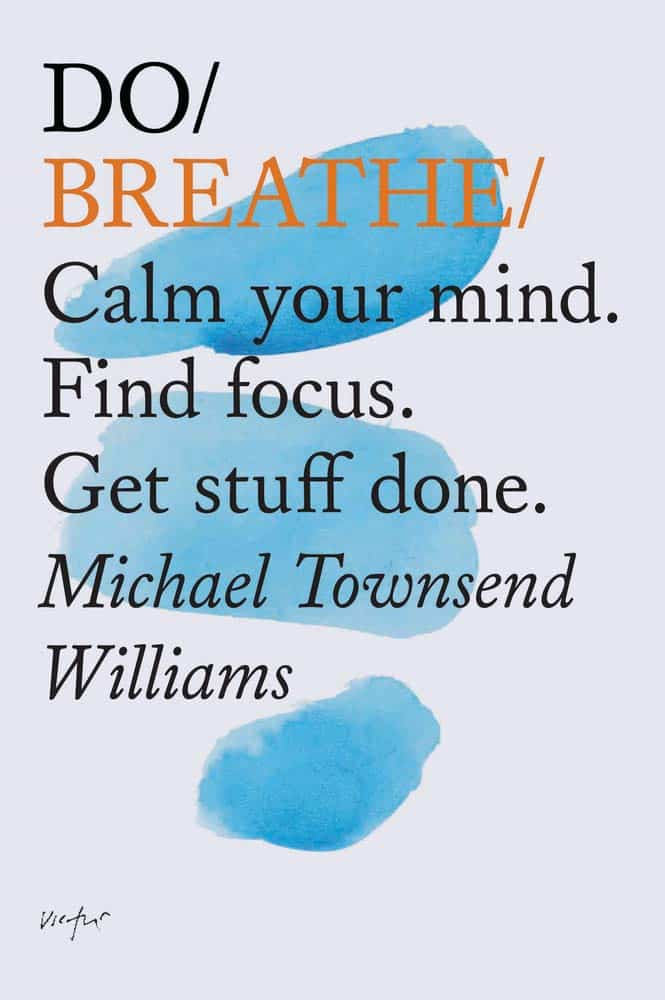
Do Breathe – by Michael Williams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever felt you could get everything in your life in order, if you could just get a little breathing room first?
Notwithstanding the title, this is mostly not a book about breathing exercises. It does cover that too, but there’s a lot more.
The author’s advices draw from a variety of high quality sources. Well-read readers will certainly recognise sections that are straight from David Allen’s “Getting Things Done”, and Mihaly Czikszentmihalyi’s “Flow”, for example, as well as Francesco Cirillo’s “Pomodoro Technique”, and James Clear’s “Atomic Habits”.
We also learn about how even simple yoga can help us, and good sleep, and a healthy diet.
In short, if you’ve been reading 10almonds for a while, you might not actually learn much new! But it’s very nice to have all these things in one book, for sure, and it’s a pleasant, easy read too.
Bottom line: if you’d like to streamline your life and not have to buy a whole stack of different books to do it, this book is a great composite that will enable you to get the job done efficiently.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tasty Tofu Scramble
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re trying to eat more plant-based, this is a great way to enjoy a culinary experience that hits the same notes as scrambled egg, with many similar nutritional benefits too, and some of its own!
You will need
- 1 cup (10oz) silken tofu
- ¼ bulb garlic, crushed
- 1 tbsp nutritional yeast
- 2 tsp chia seeds
- 2 tsp dried thyme, or 1 tsp fresh thyme, stripped (i.e. pulled off the stalks)
- 2 tsp turmeric
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- ½ tsp MSG, or 1 tsp low-sodium salt
- Extra virgin olive oil, for frying
Method
(we suggest you read everything at least once before doing anything)
1) Heat a skillet with olive oil in it; if you want a low-calorie option, you can use quite little oil here; the tofu is a lot more forgiving than egg in this regard and is almost impossible to burn unless you actively try. If you don’t want a low-calorie option, feel free to be generous with the oil if you prefer; it’ll go into the tofu and make it fattier, much like egg.
2) Add the tofu. You can just drop it (carefully) straight in; you don’t need to press it or anything.
3) Scramble it with a spatula, just the same as you would if it were egg.
4) Add the rest of the ingredients, mixing them in as you continue to scramble it, until it reaches the desired consistency.
5) Serve! Serving it on wholegrain toast is a great option—but this dish can also be enjoyed any other way you might use scrambled eggs (including for making
egg-friedtofu-fried rice; just stir it into our Tasty Versatile Rice recipe!)Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Plant vs Animal Protein: Head to Head
- Black Pepper’s Impressive Anti-Cancer Arsenal
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Why Curcumin (Turmeric) Is Worth Its Weight In Gold
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why rating your pain out of 10 is tricky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“It’s really sore,” my (Josh’s) five-year-old daughter said, cradling her broken arm in the emergency department.
“But on a scale of zero to ten, how do you rate your pain?” asked the nurse.
My daughter’s tear-streaked face creased with confusion.
“What does ten mean?”
“Ten is the worst pain you can imagine.” She looked even more puzzled.
As both a parent and a pain scientist, I witnessed firsthand how our seemingly simple, well-intentioned pain rating systems can fall flat.
altanaka/Shutterstock What are pain scales for?
The most common scale has been around for 50 years. It asks people to rate their pain from zero (no pain) to ten (typically “the worst pain imaginable”).
This focuses on just one aspect of pain – its intensity – to try and rapidly understand the patient’s whole experience.
How much does it hurt? Is it getting worse? Is treatment making it better?
Rating scales can be useful for tracking pain intensity over time. If pain goes from eight to four, that probably means you’re feeling better – even if someone else’s four is different to yours.
Research suggests a two-point (or 30%) reduction in chronic pain severity usually reflects a change that makes a difference in day-to-day life.
But that common upper anchor in rating scales – “worst pain imaginable” – is a problem.
People usually refer to their previous experiences when rating pain. sasirin pamai/Shutterstock A narrow tool for a complex experience
Consider my daughter’s dilemma. How can anyone imagine the worst possible pain? Does everyone imagine the same thing? Research suggests they don’t. Even kids think very individually about that word “pain”.
People typically – and understandably – anchor their pain ratings to their own life experiences.
This creates dramatic variation. For example, a patient who has never had a serious injury may be more willing to give high ratings than one who has previously had severe burns.
“No pain” can also be problematic. A patient whose pain has receded but who remains uncomfortable may feel stuck: there’s no number on the zero-to-ten scale that can capture their physical experience.
Increasingly, pain scientists recognise a simple number cannot capture the complex, highly individual and multifaceted experience that is pain.
Who we are affects our pain
In reality, pain ratings are influenced by how much pain interferes with a person’s daily activities, how upsetting they find it, their mood, fatigue and how it compares to their usual pain.
Other factors also play a role, including a patient’s age, sex, cultural and language background, literacy and numeracy skills and neurodivergence.
For example, if a clinician and patient speak different languages, there may be extra challenges communicating about pain and care.
Some neurodivergent people may interpret language more literally or process sensory information differently to others. Interpreting what people communicate about pain requires a more individualised approach.
Impossible ratings
Still, we work with the tools available. There is evidence people do use the zero-to-ten pain scale to try and communicate much more than only pain’s “intensity”.
So when a patient says “it’s eleven out of ten”, this “impossible” rating is likely communicating more than severity.
They may be wondering, “Does she believe me? What number will get me help?” A lot of information is crammed into that single number. This patient is most likely saying, “This is serious – please help me.”
In everyday life, we use a range of other communication strategies. We might grimace, groan, move less or differently, use richly descriptive words or metaphors.
Collecting and evaluating this kind of complex and subjective information about pain may not always be feasible, as it is hard to standardise.
As a result, many pain scientists continue to rely heavily on rating scales because they are simple, efficient and have been shown to be reliable and valid in relatively controlled situations.
But clinicians can also use this other, more subjective information to build a fuller picture of the person’s pain.
How can we communicate better about pain?
There are strategies to address language or cultural differences in how people express pain.
Visual scales are one tool. For example, the “Faces Pain Scale-Revised” asks patients to choose a facial expression to communicate their pain. This can be particularly useful for children or people who aren’t comfortable with numeracy and literacy, either at all, or in the language used in the health-care setting.
A vertical “visual analogue scale” asks the person to mark their pain on a vertical line, a bit like imagining “filling up” with pain.
Modified visual scales are sometimes used to try to overcome communication challenges. Nenadmil/Shutterstock What can we do?
Health professionals
Take time to explain the pain scale consistently, remembering that the way you phrase the anchors matters.
Listen for the story behind the number, because the same number means different things to different people.
Use the rating as a launchpad for a more personalised conversation. Consider cultural and individual differences. Ask for descriptive words. Confirm your interpretation with the patient, to make sure you’re both on the same page.
Patients
To better describe pain, use the number scale, but add context.
Try describing the quality of your pain (burning? throbbing? stabbing?) and compare it to previous experiences.
Explain the impact the pain is having on you – both emotionally and how it affects your daily activities.
Parents
Ask the clinician to use a child-suitable pain scale. There are special tools developed for different ages such as the “Faces Pain Scale-Revised”.
Paediatric health professionals are trained to use age-appropriate vocabulary, because children develop their understanding of numbers and pain differently as they grow.
A starting point
In reality, scales will never be perfect measures of pain. Let’s see them as conversation starters to help people communicate about a deeply personal experience.
That’s what my daughter did — she found her own way to describe her pain: “It feels like when I fell off the monkey bars, but in my arm instead of my knee, and it doesn’t get better when I stay still.”
From there, we moved towards effective pain treatment. Sometimes words work better than numbers.
Joshua Pate, Senior Lecturer in Physiotherapy, University of Technology Sydney; Dale J. Langford, Associate Professor of Pain Management Research in Anesthesiology, Weill Cornell Medical College, Cornell University, and Tory Madden, Associate Professor and Pain Researcher, University of Cape Town
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: