The Insider’s Guide To Making Hospital As Comfortable As Possible
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
This is Dr. Chris Bonney. He’s an anesthesiologist. If you have a surgery, he wants you to go in feeling calm, and make a quick recovery afterwards, with minimal suffering in between.
Being a patient in a hospital is a bit like being a passenger in an airplane:
- Almost nobody enjoys the thing itself, but we very much want to get to the other side of the experience.
- We have limited freedoms and comforts, and small things can make a big difference between misery and tolerability.
- There are professionals present to look after us, but they are busy and have a lot of other people to tend to too.
So why is it that there are so many resources available full of “tips for travelers” and so few “tips for hospital patients”?
Especially given the relative risks of each, and likelihood, or even near-certainty of coming to at least some harm… One would think “tips for patients” would be more in demand!
Tips for surgery patients, from an insider expert
First, he advises us: empower yourself.
Empowering yourself in this context means:
- Relax—doctors really want you to feel better, quickly. They’re on your side.
- Research—knowledge is power, so research the procedure (and its risks!). Dr. Bonney, himself an anesthesiologist, particularly recommends you learn what specific anesthetic will be used (there are many, and they’re all a bit different!), and what effects (and/or after-effects) that may have.
- Reframe—you’re not just a patient; you’re a customer/client. Many people suffer from MDeity syndrome, and view doctors as authority figures, rather than what they are: service providers.
- Request—if something would make you feel better, ask for it. If it’s information, they will be not only obliged, but also enthusiastic, to give it. If it’s something else, they’ll oblige if they can, and the worst case scenario is something won’t be possible, but you won’t know if you don’t ask.
Next up, help them to help you
There are various ways you can be a useful member of your own care team:
- Go into surgery as healthy as you can. If there’s ever a time to get a little fitter, eat a little healthier, prioritize good quality sleep more, the time approaching your surgery is the time to do this.
- This will help to minimize complications and maximize recovery.
- Take with you any meds you’re taking, or at least have an up-to-date list of what you’re taking. Dr. Bonney has very many times had patients tell him such things as “Well, let me see. I have two little pink ones and a little white one…” and when asked what they’re for they tell him “I have no idea, you’d need to ask my doctor”.
- Help them to help you; have your meds with you, or at least a comprehensive list (including: medication name, dosage, frequency, any special instructions)
- Don’t stop taking your meds unless told to do so. Many people have heard that one should stop taking meds before a surgery, and sometimes that’s true, but often it isn’t. Keep taking them, unless told otherwise.
- If unsure, ask your surgical team in advance (not your own doctor, who will not be as familiar with what will or won’t interfere with a surgery).
Do any preparatory organization well in advance
Consider the following:
- What do you need to take with you? Medications, clothes, toiletries, phone charger, entertainment, headphones, paperwork, cash for the vending machine?
- Will the surgeons need to shave anywhere, and if so, might you prefer doing some other form of depilation (e.g. waxing etc) yourself in advance?
- Is your list of medications ready?
- Who will take you to the hospital and who will bring you back?
- Who will stay with you for the first 24 hours after you’re sent home?
- Is someone available to look after your kids/pets/plants etc?
Be aware of how you do (and don’t) need to fast before surgery
The American Society of Anesthesiologists gives the following fasting guidelines:
- Non-food liquids: fast for at least 2 hours before surgery
- Food liquids or light snacks: fast for at least 6 hours before surgery
- Fried foods, fatty foods, meat: fast for at least 8 hours before surgery
(see the above link for more details)
Dr. Bonney notes that many times he’s had patients who’ve had the worst thirst, or caffeine headache, because of abstaining unnecessarily for the day of the surgery.
Unless told otherwise by your surgical team, you can have black coffee/tea up until two hours before your surgery, and you can and should have water up until two hours before surgery.
Hydration is good for you and you will feel the difference!
Want to know more?
Dr. Bonney has his own website and blog, where he offers lots of advice, including for specific conditions and specific surgeries, with advice for before/during/after your hospital stay.
He also has a book with many more tips like those we shared today:
Calm For Surgery: Supertips For A Smooth Recovery
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healing Your Gut: Anastasia’s Journey and Tips
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anastasia Gurova shares her inspiring journey from chronic gut issues to vibrant health.
A Personal Journey to Gut Health
In the below video, Anastasia shares her long struggle with gut problems, including SIBO, IBS, and gastritis. She talks about ending up in the hospital with severe bloating, only to find that a range of medical approaches didn’t provide her with any lasting relief. This led her to explore the importance of the microbiome and its crucial role in gut health, which is what we’ll be focusing on in this overview.
Key Insights and Tips
The most valuable parts of Anastasia’s story for 10almonds readers are, in our opinion, the solutions she discovered to her gut issues. You’ll have to watch her video to discover all of them, but here are some of our favorites:
- Reintroduce Whole Grains and Legumes: Despite the popularity of grain-free diets, Anastasia found significant improvements in her gut health by adding whole grains like quinoa, oats, and buckwheat back into her diet. These foods provide essential fibers that feed beneficial gut bacteria.
- Soaking and Fermenting Foods: To make grains and legumes more digestible, Anastasia recommends soaking them overnight. This is similar to the common technique people use on oats. She also includes fermented foods like sauerkraut, kimchi, and yogurt in her diet, which introduce beneficial bacteria to the gut.
- Resistant Starches: Foods like cooked and cooled rice, potatoes, and green bananas contain resistant starches that promote healthy gut bacteria. Anastasia emphasizes incorporating these into meals to support gut health.
- Mindful Eating: Anastasia found that taking time to chew food thoroughly and savor each bite helped improve her digestion. She avoids distractions like TV while eating and pays attention to the textures and flavors of her meals.
- Avoid Overly Restrictive Diets: Anastasia warns against overly restrictive diets like keto and strict SIBO diets that cut out all carbs and fiber. These can worsen gut health by starving beneficial bacteria.
That’s Only The Beginning
Anastasia’s video goes far beyond what we’ve covered in this short introduction; she provides a detailed look at the steps she took, from dietary changes to lifestyle adjustments, and offers tips that anyone can apply. Plus, she explains the science behind these changes, which, of course, we love.
Enjoy the video! (It would be remiss for us to not bring up our general intro to gut health, or our more specific article on the gut-brain connection)
Good luck on your gut-health journey!
Share This Post
-
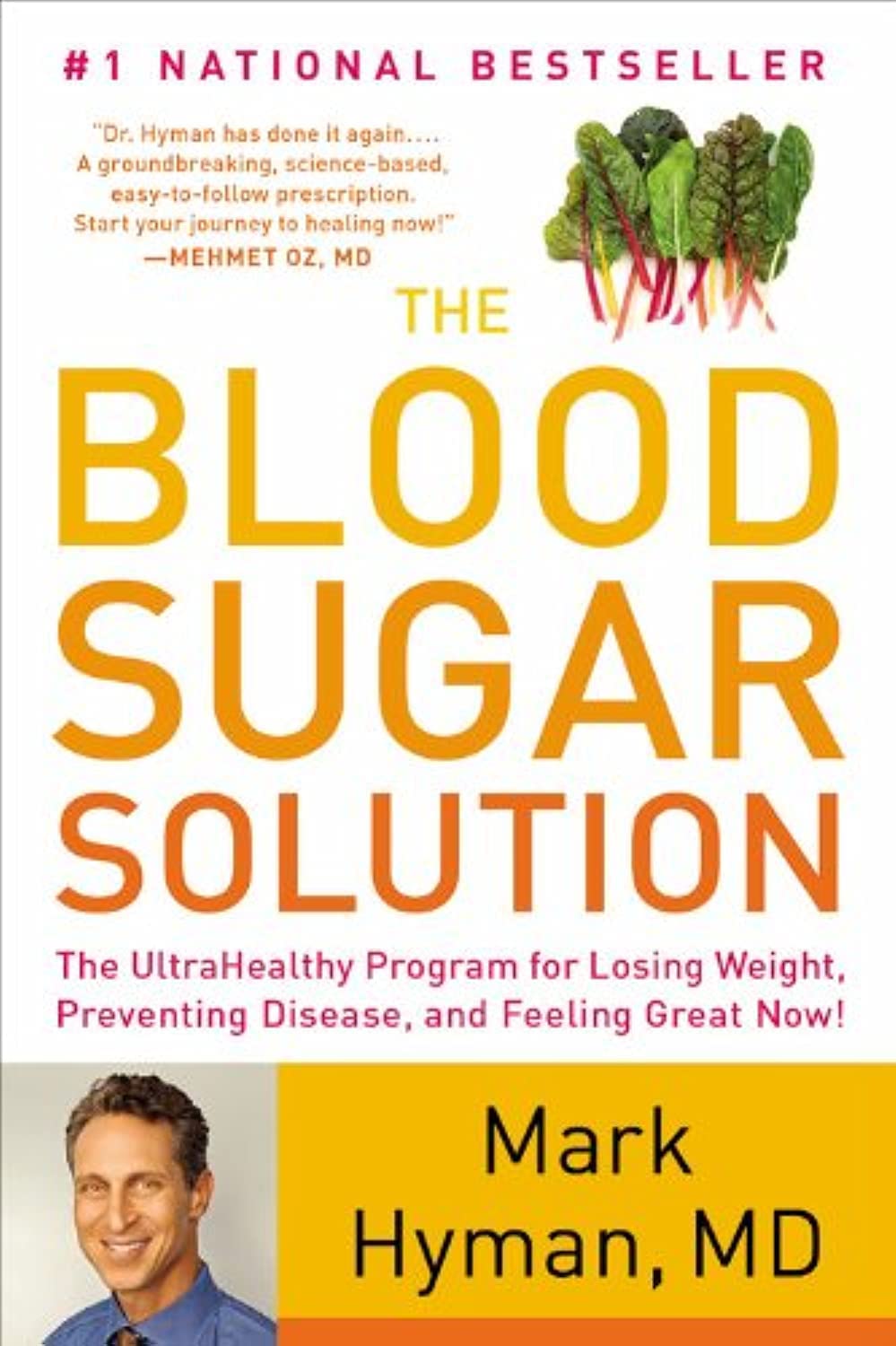
The Blood Sugar Solution – by Dr. Mark Hyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The main purpose of this book is combating metabolic disease, the amalgam of what’s often prediabetes (sometimes fully-fledged diabetes) and cardiovascular disease (sometimes fully-fledged heart disease).
To achieve this (after an introductory section explaining what the sociomedical problems are and why the sociomedical problems are happening), he offers a seven-step program; we’ll not keep those steps a mystery; they are:
- Boost your nutrition
- Regulate your hormones
- Reduce inflammation
- Improve your digestion
- Maximize detoxification
- Enhance energy metabolism
- Soothe your mind
Thereafter, it’s all about leading the reader by the hand through the steps; he also offers a six-week action plan, and a six-week meal plan with recipes.
The style is very sensationalist (too sensationalist for this reviewer’s personal taste) but nevertheless backed up with hard science when it comes to hard claims. So, if you don’t mind wading through (or skipping) some early chapters that are a bit “used car salesman” in feel, there’s actually a lot of good information, especially in the middle of the book, and useful practical guides in the middle and end.
Bottom line: if you want a good comprehensive science-based practical guide to addressing the risk of metabolic disease, this is that.
Click here to check out The Blood Sugar Solution, and look after yours!
Share This Post
-
Semaglutide’s Surprisingly Unexamined Effects
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide’s Surprisingly Big Research Gap
GLP-1 receptor agonists like Ozempic, Wegovy, and other semaglutide drugs. are fast becoming a health industry standard go-to tool in the weight loss toolbox. When it comes to recommending that patients lose weight, “Have you considered Ozempic?” is the common refrain.
Sometimes, this may be a mere case of kicking the can down the road with regard to some other treatment that it can be argued (sometimes even truthfully) would go better after some weight loss:
How weight bias in health care can harm patients with obesity: Research
…which we also covered in fewer words in the second-to-last item here:
But GLP-1 agonists work, right?
Yes, albeit there’s a litany of caveats, top of which are usually:
- there are often adverse gastrointestinal side effects
- if you stop taking them, weight regain generally ensues promptly
For more details on these and more, see:
…but now there’s another thing that’s come to light:
The dark side of semaglutide’s weight loss
In academia, “dark” is often used to describe “stuff we don’t have much (or in some cases, any) direct empirical evidence of, but for reasons of surrounding things, we know it’s there”.
Well-known examples include “dark matter” in physics and the Dark Ages in (European) history.
In the case of semaglutide and weight loss, a review by a team of researchers (Drs. Sandra Christenen, Katie Robinson, Sara Thomas, and Dominique Williams) has discovered how little research has been done into a certain aspect of GLP-1 agonist’s weight loss effects, namely…
Dietary changes!
There’s been a lot of popular talk about “people taking semaglutide eat less”, but it’s mostly anecdotal and/or presumed based on parts of the mechanism of action (increasing insulin production, reducing glucagon secretions, modulating dietary cravings).
Where studies have looked at dietary changes, it’s almost exclusively been a matter of looking at caloric intake (which has been found to be a 16–39% reduction), and observations-in-passing that patients reported reduction in cravings for fatty and sweet foods.
This reduction in caloric intake, by the way, is not significantly different to the reduction brought about by counselling alone (head-to-head studies have been done; these are also discussed in the research review).
However! It gets worse. Very few studies of good quality have been done, even fewer (two studies) actually had a registered dietitian nutritionist on the team, and only one of them used the “gold standard” of nutritional research, the 24-hour dietary recall test. Which, in case you’re curious, you can read about what that is here:
Dietary Assessment Methods: What Is A 24-Hour Recall?
Of the four studies that actually looked at the macros (unlike most studies), they found that on average, protein intake decreased by 17.1%. Which is a big deal!
It’s an especially big deal, because while protein’s obviously important for everyone, it’s especially important for anyone trying to lose weight, because muscle mass is a major factor in metabolic base rate—which in turn is much important for fat loss/maintenance than exercise, when it comes to how many calories we burn by simply existing.
A reasonable hypothesis, therefore, is that one of the numerous reasons people who quit GLP-1 agonists immediately put fat back on, is because they probably lost muscle mass in amongst their weight loss, meaning that their metabolic base rate will have decreased, meaning that they end up more disposed to put on fat than before.
And, that’s just a hypothesis and it’s a hypothesis based on very few studies, so it’s not something to necessarily take as any kind of definitive proof of anything, but it is to say—as the researchers of this review do loudly say—more research needs to be done into this, because this has been a major gap in research so far!
Any other bad news?
While we’re talking research gaps, guess how many studies looked into micronutrient intake changes in people taking GLP-1 agonists?
If you guessed zero, you guessed correctly.
You can find the paper itself here:
What’s the main take-away here?
On a broad, scoping level: we need more research!
On a “what this means for individuals who want to lose weight” level: maybe we should be more wary of this still relatively new (less than 10 years old) “wonder drug”. And for most of those 10 years it’s only been for diabetics, with weight loss use really being in just the past few years (2021 onwards).
In other words: not necessarily any need to panic, but caution is probably not a bad idea, and natural weight loss methods remain very reasonable options for most people.
See also: How To Lose Weight (Healthily!)
Take care!
Share This Post
Related Posts
-
Eating For Energy (In Ways That Actually Work)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Snacks & Hacks: The Real Energy Boosters
Declining energy levels are a common complaint of people getting older, and this specific kind of “getting older” is starting earlier and earlier (even Gen-Z are already getting in line for this one). For people of all ages, however, diet is often a large part of the issue.
The problem:
It can sometimes seem, when it comes to food and energy levels, that we have a choice:
- Don’t eat (energy levels decline)
- Eat quick-release energy snacks (energy spikes and crashes)
- Eat slow-release energy meals (oh hi, post-dinner slump)
But, this minefield can be avoided! Advice follows…
Skip the quasi-injectables
Anything the supermarket recommends for rapid energy can be immediately thrown out (e.g. sugary energy drinks, glucose tablets, and the like).
Same goes for candy of most sorts (if the first ingredient is sugar, it’s not good for your energy levels).
Unless you are diabetic and need an emergency option to keep with you in case of a hypo, the above things have no place on a healthy shopping list.
Aside from that, if you have been leaning on these heavily, you might want to check out yesterday’s main feature:
The Not-So-Sweet Science Of Sugar Addiction
…and if your knee-jerk response is “I’m not addicted; I just enjoy…” then ok, test that! Skip it for this month.
- If you succeed, you’ll be in better health.
- If you don’t, you’ll be aware of something that might benefit from more attention.
Fruit and nuts are your best friends
Unless you are allergic, in which case, obviously skip your allergen(s).
But for most of us, we were born to eat fruit and nuts. Literally, those two things are amongst the oldest and most well-established parts of human diet, which means that our bodies have had a very long time to evolve the perfect fruit-and-nut-enjoying abilities, and reap the nutritional benefits.
Nuts are high in fat (healthy fats) and that fat is a great source of energy’s easy for the body to get from the food, and/but doesn’t result in blood sugar spikes (and thus crashes) because, well, it’s not a sugar.
See also: Why You Should Diversify Your Nuts
Fruit is high in sugars, and/but high in fiber that slows the absorption into a nice gentle curve, and also contains highly bioavailable vitamins to perk you up and polyphenols to take care of your long-term health too.
Be warned though: fruit juice does not work the same as actual fruit; because the fiber has been stripped and it’s a liquid, those sugars are zipping straight in exactly the same as a sugary energy drink.
See also: Which Sugars Are Healthier, And Which Are Just The Same?
Slow release carbs yes, but…
Eating a bowl of wholegrain pasta is great if you don’t have to do anything much immediately afterwards, but it won’t brighten your immediately available energy much—on the contrary, energy will be being used for digestion for a while.
So if you want to eat slow-release carbs, make it a smaller portion of something more-nutrient dense, like oats or lentils. This way, the metabolic load will be smaller (because the portion was smaller) but the higher protein content will prompt satiety sooner (so you addressed your hunger with a smaller portion) and the iron and B vitamins will be good for your energy too.
See also: Should You Go Light Or Heavy On Carbs?
Animal, vegetable, or mineral?
At the mention of iron and B vitamins, you might be thinking about various animal products that might work too.
If you are vegetarian or vegan: stick to that; it’s what your gut microbiome is used to now, and putting an animal product in will likely make you feel ill.
If you have them in your diet already, here’s a quick rundown of how broad categories of animal product work (or not) for energy:
- Meat: nope. Well, the fat, if applicable, will give you some energy, but less than you need just to digest the meat. This, by the way, is a likely part of why the paleo diet is good for short term weight loss. But it’s not very healthy.
- Fish: healthier than the above, but for energy purposes, just the same.
- Dairy: high-fat dairy, such as cream and butter, are good sources of quick energy. Be aware if they contain lactose though, that this is a sugar and can be back to spiking blood sugars.
- As an aside for diabetics: this is why milk can be quite good for correcting a hypo: the lactose provides immediate sugar, and the fat keeps it more balanced afterwards
- Eggs: again the fat is a good source of quick energy, and the protein is easier to digest than that of meat (after all, egg protein is literally made to be consumed by an embryo, while meat protein is made to be a functional muscle of an animal), so the metabolic load isn’t too strenuous. Assuming you’re doing a moderate consumption (under 3 eggs per day) and not Sylvester Stallone-style 12-egg smoothies, you’re good to go.
See also: Do We Need Animal Products To Be Healthy?
…and while you’re at it, check out:
Eggs: Nutritional Powerhouse
or Heart-Health Timebomb?(spoiler: it’s the former; the title was because it was a mythbusting edition)
Hydration considerations
Lastly, food that is hydrating will be more energizing than food that is not, so how does your snack/meal rank on a scale of watermelon to saltines?
You may be thinking: “But you said to eat nuts! They’re not hydrating at all!”, in which case, indeed, drink water with them, or better yet, enjoy them alongside fruit (hydration from food is better than hydration from drinking water).
And as for those saltines? Salt is not your friend (unless you are low on sodium, because then that can sap your energy)
How to tell if you are low on sodium: put a little bit (e.g. ¼ tsp) of salt into a teaspoon and taste it; does it taste unpleasantly salty? If not, you were low on sodium. Have a little more at five minute intervals, until it tastes unpleasantly salty. Alternatively have a healthy snack that nonetheless contains a little salt.
If you otherwise eat salty food as an energy-giving snack, you risk becoming dehydrated and bloated, neither of which are energizing conditions.
Dehydrated and bloated at once? Yes, the two often come together, even though it usually doesn’t feel like it. Basically, if we consume too much salty food, our homeostatic system goes into overdrive to try to fix it, borrows a portion of our body’s water reserves to save us from the salt, and leaves us dehydrated, bloated, and sluggish.
For more on salt in general, check out:
How Too Much Salt Can Lead To Organ Failure: Lesser-Known Salt Health Risks
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Stress-Proof Brain – by Dr. Melanie Greenberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The premise of the book is as stated in the subtitle: using mindfulness and neuroplasticity to manage our stress response.
As such, it’s divided into three parts:
- Understanding your stress (and different types of stressors)
- Calming your amygdalae (thus, dealing with your stress response while the stressor is stressing you)
- Moving forward with your prefrontal cortex (and thus, gradually improving automatic stress responses over time, as we learn new, better responses to do automatically)
The content ranges from the neurophysiological to “therapist’s couch” stuff; Dr. Greenberg having her PhD in psychology has prepared her to write both of those different-but-touching fields with equal competence. In-line citations are given throughout, for those who want to look up studies.
The style is direct and informative, with little to no attention given to making it an entertaining read. As a result, it’s information dense (which is good), and/but not necessarily a “couldn’t put it down” page-turner.
Bottom line: if you’d like to improve your ability to deal with stress, this book is as good as any.
Click here to check out The Stress-Proof Brain, and stress-proof yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Psychology Sunday: Family Estrangement & How To Fix It
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Estrangement, And How To Heal It
We’ve written before about how deleterious to the health loneliness and isolation can be, and what things can be done about it. Today, we’re tackling a related but different topic.
We recently had a request to write about…
❝Reconciliation of relationships in particular estrangement mother adult daughter❞
And, this is not only an interesting topic, but a very specific one that affects more people than is commonly realized!
In fact, a recent 800-person study found that more than 43% of people experienced family estrangement of one sort or another, and a more specific study of more than 2,000 mother-child pairs found that more than 11% of mothers were estranged from at least one adult child.
So, if you think of the ten or so houses nearest to you, probably at least one of them contains a parent estranged from at least one adult child. Maybe it’s yours. Either way, we hope this article will give you some pause for thought.
Which way around?
It makes a difference to the usefulness of this article whether any given reader experiencing estrangement is the parent or the adult child. We’re going to assume the reader is the parent. It also makes a difference who did the estranging. That’s usually the adult child.
So, we’re broadly going to write with that expectation.
Why does it happen?
When our kids are small, we as parents hold all the cards. It may not always feel that way, but we do. We control our kids’ environment, we influence their learning, we buy the food they eat and the clothes they wear. If they want to go somewhere, we probably have to take them. We can even set and enforce rules on a whim.
As they grow, so too does their independence, and it can be difficult for us as parents to relinquish control, but we’re going to have to at some point. Assuming we are good parents, we just hope we’ve prepared them well enough for the world.
Once they’ve flown the nest and are living their own adult lives, there’s an element of inversion. They used to be dependent on us; now, not only do they not need us (this is a feature not a bug! If we have been good parents, they will be strong without us, and in all likelihood one day, they’re going to have to be), but also…
We’re more likely to need them, now. Not just in the “oh if we have kids they can look after us when we’re old” sense, but in that their social lives are growing as ours are often shrinking, their family growing, while ours, well, it’s the same family but they’re the gatekeepers to that now.
If we have a good relationship, this goes fine. However, it might only take one big argument, one big transgression, or one “final straw”, when the adult child decides the parent is more trouble than they’re worth.
And, obviously, that’s going to hurt. But it’s pretty much how it pans out, according to studies:
Here be science: Tensions in the Parent and Adult Child Relationship: Links to Solidarity and Ambivalence
How to fix it, step one
First, figure out what went wrong.
Resist any urge to protect your own feelings with a defensive knee-jerk “I don’t know; I was a good, loving parent”. That’s a very natural and reasonable urge and you’re quite possibly correct, but it won’t help you here.
Something pushed them away. And, it will almost certainly have been a push factor from you, not a pull factor from whoever is in their life now. It’s easy to put the blame externally, but that won’t fix anything.
And, be honest with yourself; this isn’t a job interview where we have to present a strength dressed up as a “greatest weakness” for show.
You can start there, though! If you think “I was too loving”, then ok, how did you show that love? Could it have felt stifling to them? Controlling? Were you critical of their decisions?
It doesn’t matter who was right or wrong, or even whether or not their response was reasonable. It matters that you know what pushed them away.
How to fix it, step two
Take responsibility, and apologize. We’re going to assume that your estrangement is such that you can, at least, still get a letter to them, for example. Resist the urge to argue your case.
Here’s a very good format for an apology; please consider using this template:
The 10-step (!) apology that’s so good, you’ll want to make a note of it
You may have to do some soul-searching to find how you will avoid making the same mistake in the future, that you did in the past.
If you feel it’s something you “can’t change”, then you must decide what is more important to you. Only you can make that choice, but you cannot expect them to meet you halfway. They already made their choice. In the category of negotiation, they hold all the cards now.
How to fix it, step three
Now, just wait.
Maybe they will reply, forgiving you. If they do, celebrate!
Just be aware that once you reconnect is not the time to now get around to arguing your case from before. It will never be the time to get around to arguing your case from before. Let it go.
Nor should you try to exact any sort of apology from them for estranging you, or they will at best feel resentful, wonder if they made a mistake in reconnecting, and withdraw.
Instead, just enjoy what you have. Many people don’t get that.
If they reply with anger, maybe it will be a chance to reopen a dialogue. If so, family therapy could be an approach useful for all concerned, if they are willing. Chances are, you all have things that you’d all benefit from talking about in a calm, professional, moderated, neutral environment.
You might also benefit from a book we reviewed previously, “Parent Effectiveness Training”. This may seem like “shutting the stable door after the horse has bolted”, but in fact it’s a very good guide to relationship dynamics in general, and extensively covers relations between parents and adult children.
If they don’t reply, then, you did your part. Take solace in knowing that much.
Some final thoughts:
At the end of the day, as parents, our kids living well is (hopefully) testament to that we prepared them well for life, and sometimes, being a parent is a thankless task.
But, we (hopefully) didn’t become parents for the plaudits, after all.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: