What does it mean to be immunocompromised?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our immune systems help us fight off disease, but certain health conditions and medications can weaken our immune systems. People whose immune systems don’t work as well as they should are considered immunocompromised.
Read on to learn more about how the immune system works, what causes people to be immunocompromised, and how we can protect ourselves and the immunocompromised people around us from illness.
What is the immune system?
The immune system is a network of cells, organs, and chemicals that helps our bodies fight off infections caused by invaders, such as bacteria, viruses, fungi, and parasites.
Some important parts of the immune system include:
- White blood cells, which attack and kill germs that don’t belong inside our bodies.
- Lymph nodes, which help our bodies filter out germs.
- Antibodies, which help our bodies recognize invaders.
- Cytokines, which tell our immune cells what to do.
What causes people to be immunocompromised?
Some health conditions and medications can prevent our immune systems from functioning optimally, which makes us more vulnerable to infection. Health conditions that compromise the immune system fall into two categories: primary immunodeficiency and secondary immunodeficiency.
Primary immunodeficiency
People with primary immunodeficiency are born with genetic mutations that prevent their immune systems from functioning as they should. There are hundreds of types of primary immunodeficiencies. Since these mutations affect the immune system to varying degrees, some people may experience symptoms and get diagnosed early in life, while others may not know they’re immunocompromised until adulthood.
Secondary immunodeficiency
Secondary immunodeficiency happens later in life due to an infection like HIV, which weakens the immune system over time, or certain types of cancer, which prevent the body from producing enough white blood cells to adequately fight off infection. Studies have also shown that getting infected with COVID-19 may cause immunodeficiency by reducing our production of “killer T-cells,” which help fight off infections.
Sometimes necessary treatments for certain medical conditions can also cause secondary immunodeficiency. For example, people with autoimmune disorders—which cause the immune system to become overactive and attack healthy cells—may need to take immunosuppressant drugs to manage their symptoms. However, the drugs can make them more vulnerable to infection.
People who receive organ transplants may also need to take immunosuppressant medications for life to prevent their body from rejecting the new organ. (Given the risk of infection, scientists continue to research alternative ways for the immune system to tolerate transplantation.)
Chemotherapy for cancer patients can also cause secondary immunodeficiency because it kills the immune system’s white blood cells as it’s trying to kill cancer cells.
What are the symptoms of a compromised immune system?
People who are immunocompromised may become sick more frequently than others or may experience more severe or longer-term symptoms than others who contract the same disease.
Other symptoms of a compromised immune system may include fatigue; digestive problems like cramping, nausea, and diarrhea; and slow wound healing.
How can I find out if I’m immunocompromised?
If you think you may be immunocompromised, talk to your health care provider about your medical history, your symptoms, and any medications you take. Blood tests can determine whether your immune system is producing adequate proteins and cells to fight off infection.
I’m immunocompromised—how can I protect myself from infection?
If you’re immunocompromised, take precautions to protect yourself from illness.
Wash your hands regularly, wear a well-fitting mask around others to protect against respiratory viruses, and ensure that you’re up to date on recommended vaccines.
Immunocompromised people may need more doses of vaccines than people who are not immunocompromised—including COVID-19 vaccines. Talk to your health care provider about which vaccines you need.
How can I protect the immunocompromised people around me?
You never know who may be immunocompromised. The best way to protect immunocompromised people around you is to avoid spreading illnesses.
If you know you’re sick, isolate whenever possible. Wear a well-fitting mask around others—especially if you know that you’re sick or that you’ve been exposed to germs. Make sure you’re up to date on recommended vaccines, and practice regular hand-washing.
If you’re planning to spend time with someone who is immunocompromised, ask them what steps you can take to keep them safe.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mung Beans vs Black Gram – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to black gram, we picked the black gram.
Why?
Both are great, and it was close!
In terms of macros, the main difference is that mung beans have slightly more fiber, while black gram has slightly more protein. So, it comes down to which we prioritize out of those two, and we’re going to call it fiber and thus hand the win in this category to mung beans—but it’s very close in either case.
In the category of vitamins, mung beans have more of vitamins B1, B6, and B9, while black gram has more of vitamins A, B2, B3, and B5. They’re equal on vitamins C, E, K, and choline. So, a marginal victory by the numbers for black gram here.
When it comes to minerals, mung beans have more copper and potassium, while black gram has more calcium, iron, magnesium, manganese, and phosphorus. They’re equal on selenium and zinc. Another win for black gram.
Adding up the sections makes for an overall win for black gram, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
-
Debate over tongue tie procedures in babies continues. Here’s why it can be beneficial for some infants
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There is increasing media interest about surgical procedures on new babies for tongue tie. Some hail it as a miracle cure, others view it as barbaric treatment, though adverse outcomes are rare.
Tongue tie occurs when the tissue under the tongue is attached to the lower gum or floor of the mouth in a way that can restrict the movement or range of the tongue. This can impact early breastfeeding in babies. It affects an estimated 8% of children under one year of age.
While there has been an increase in tongue tie releases (also called division or frenotomy), it’s important to keep this in perspective relative to the increase in breastfeeding rates.
The World Health Organization recommends exclusive breastfeeding for the first six months of life, with breastfeeding recommended into the second year of life and beyond for the health of mother and baby as well as optimal growth. Global rates of breastfeeding infants for the first six months have increased from 38% to 48% over the past decade. So, it is not surprising there is also an increase in the number of babies being referred globally with breastfeeding challenges and potential tongue tie.
An Australian study published in 2023 showed that despite a 25% increase in referrals for tongue tie division between 2014 and 2018, there was no increase in the number of tongue tie divisions performed. Tongue tie surgery rates increased in Australia in the decade from 2006 to 2016 (from 1.22 per 1,000 population to 6.35) for 0 to 4 year olds. There is no data on surgery rates in Australia over the last eight years.
Tongue tie division isn’t always appropriate but it can make a big difference to the babies who need it. More referrals doesn’t necessarily mean more procedures are performed.
chomplearn/Shutterstock How tongue tie can affect babies
When tongue tie (ankyloglossia) restricts the movement of the tongue, it can make it more difficult for a baby to latch onto the mother’s breast and painlessly breastfeed.
Earlier this month, the International Consortium of oral Ankylofrenula Professionals released a tongue tie position statement and practice guideline. Written by a range of health professionals, the guidelines define tongue tie as a functional diagnosis that can impact breastfeeding, eating, drinking and speech. The guidelines provide health professionals and families with information on the assessment and management of tongue tie.
Tongue tie release has been shown to improve latch during breastfeeding, reduce nipple pain and improve breast and bottle feeding. Early assessment and treatment are important to help mothers breastfeed for longer and address any potential functional problems.
The frenulum is a band of tissue under the tongue that is attached to the gumline base of the mouth. Akkalak Aiempradit/Shutterstock Where to get advice
If feeding isn’t going well, it may cause pain for the mother or there may be signs the baby isn’t attaching properly to the breast or not getting enough milk. Parents can seek skilled help and assessment from a certified lactation consultant or International Board-Certified Lactation Consultant who can be found via online registry.
Alternatively, a health professional with training and skills in tongue tie assessment and division can assist families. This may include a doctor, midwife, speech pathologist or dentist with extended skills, training and experience in treating babies with tongue tie.
When access to advice or treatment is delayed, it can lead to unnecessary supplementation with bottle feeds, early weaning from breastfeeding and increased parental anxiety.
Getting a tongue tie assessment
During assessment, a qualified health professional will collect a thorough case history, including pregnancy and birth details, do a structural and functional assessment, and conduct a comprehensive breastfeeding or feeding assessment.
They will view and thoroughly examine the mouth, including the tongue’s movement and lift. The appearance of where the tissue attaches to the underside of the tongue, the ability of the tongue to move and how the baby can suck also needs to be properly assessed.
Treatment decisions should focus on the concerns of the mother and baby and the impact of current feeding issues. Tongue tie division as a baby is not recommended for the sole purpose of avoiding speech problems in later life if there are no feeding concerns for the baby.
A properly qualified lactation consultant can help with positioning and attachment. HarryKiiM Stock/Shutterstock Treatment options
The Australian Dental Association’s 2020 guidelines provide a management pathway for babies diagnosed with tongue tie.
Once feeding issues are identified and if a tongue tie is diagnosed, non-surgical management to optimise positioning, latch and education for parents should be the first-line approach.
If feeding issues persist during follow-up assessment after non-surgical management, a tongue tie division may be considered. Tongue tie release may be one option to address functional challenges associated with breastfeeding problems in babies.
There are risks associated with any procedure, including tongue tie release, such as bleeding. These risks should be discussed with the treating practitioner before conducting any laser, scissor or scalpel tongue tie procedure.
Post-release support by a certified lactation consultant or feeding specialist is necessary after a tongue tie division. A post-release treatment plan should be developed by a team of health professionals including advice and support for breastfeeding to address both the mother and baby’s individual needs.
We would like to acknowledge the contribution of Raymond J. Tseng, DDS, PhD, (Paediatric Dentist) to the writing of this article.
Sharon Smart, Lecturer and Researcher (Speech Pathology) – School of Allied Health, Curtin University; David Todd, Associate Professor, Neonatology, ANU Medical School, Australian National University, and Monica J. Hogan, PhD student, ANU School of Medicine and Psychology, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Keep Inflammation At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to Prevent (or Reduce) Inflammation
You asked us to do a main feature on inflammation, so here we go!
Before we start, it’s worth noting an important difference between acute and chronic inflammation:
- Acute inflammation is generally when the body detects some invader, and goes to war against it. This (except in cases such as allergic responses) is usually helpful.
- Chronic inflammation is generally when the body does a civil war. This is almost never helpful.
We’ll be tackling the latter, which frees up your body’s resources to do better at the former.
First, the obvious…
These five things are as important for this as they are for most things:
- Get a good diet—the Mediterranean diet is once again a top-scorer
- Exercise—move and stretch your body; don’t overdo it, but do what you reasonably can, or the inflammation will get worse.
- Reduce (or ideally eliminate) alcohol consumption. When in pain, it’s easy to turn to the bottle, and say “isn’t this one of red wine’s benefits?” (it isn’t, functionally*). Alcohol will cause your inflammation to flare up like little else.
- Don’t smoke—it’s bad for everything, and that goes for inflammation too.
- Get good sleep. Obviously this can be difficult with chronic pain, but do take your sleep seriously. For example, invest in a good mattress, nice bedding, a good bedtime routine, etc.
*Resveratrol (which is a polyphenol, by the way), famously found in red wine, does have anti-inflammatory properties. However, to get enough resveratrol to be of benefit would require drinking far more wine than will be good for your inflammation or, indeed, the rest of you. So if you’d like resveratrol benefits, consider taking it as a supplement. Superficially it doesn’t seem as much fun as drinking red wine, but we assure you that the results will be much more fun than the inflammation flare-up after drinking.
About the Mediterranean Diet for this…
There are many causes of chronic inflammation, but here are some studies done with some of the most common ones:
- Beneficial effect of Mediterranean diet in systemic lupus erythematosus patients
- How the Mediterranean diet and some of its components modulate inflammatory pathways in arthritis
- The effects of the Mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease
- Adherence to Mediterranean diet and 10-year incidence of diabetes: correlations with inflammatory and oxidative stress biomarkers*
*Type 1 diabetes is a congenital autoimmune disorder, as the pancreas goes to war with itself. Type 2 diabetes is different, being a) acquired and b) primarily about insulin resistance, and/but this is related to chronic inflammation regardless. It is also possible to have T1D and go on to develop insulin resistance, and that’s very bad, and/but beyond the scope of today’s newsletter, in which we are focusing on the inflammation aspects.
Some specific foods to eat or avoid…
Eat these:
- Leafy greens
- Cruciferous vegetables
- Tomatoes
- Fruits in general (berries in particular)
- Healthy fats, e.g. olives and olive oil
- Almonds and other nuts
- Dark chocolate (choose high cocoa, low sugar)
Avoid these:
- Processed meats (absolute worst offenders are hot dogs, followed by sausages in general)
- Red meats
- Sugar (includes most fruit juices, but not most actual fruits—the difference with actual fruits is they still contain plenty of fiber, and in many cases, antioxidants/polyphenols that reduce inflammation)
- Dairy products (unless fermented, in which case it seems to be at worst neutral, sometimes even a benefit, in moderation)
- White flour (and white flour products, e.g. white bread, white pasta, etc)
- Processed vegetable oils
See also: 9 Best Drinks To Reduce Inflammation, Says Science
Supplements?
Some supplements that have been found to reduce inflammation include:
(links are to studies showing their efficacy)
Consider Intermittent Fasting
Remember when we talked about the difference between acute and chronic inflammation? It’s fair to wonder “if I reduce my inflammatory response, will I be weakening my immune system?”, and the answer is: generally, no.
Often, as with the above supplements and dietary considerations, reducing inflammation actually results in a better immune response when it’s actually needed! This is because your immune system works better when it hasn’t been working in overdrive constantly.
Here’s another good example: intermittent fasting reduces the number of circulating monocytes (a way of measuring inflammation) in healthy humans—but doesn‘t compromise antimicrobial (e.g. against bacteria and viruses) immune response.
See for yourself: Dietary Intake Regulates the Circulating Inflammatory Monocyte Pool ← the study is about the anti-inflammatory effects of fasting
Share This Post
Related Posts
-
Why Some People Get Sick More (And How To Not Be One Of Them)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some people have never yet had COVID (so far so good, this writer included); others are on their third bout already; others have not been so lucky and are no longer with us to share their stories.
Obviously, even the healthiest and/or most careful person can get sick, and it would be folly to be complacent and think “I’m not a person who gets sick; that happens to other people”.
Nor is COVID the only thing out there to worry about; there’s always the latest outbreak-du-jour of something, and there are always the perennials such as cold and flu—which are also not to be underestimated, because both weaken us to other things, and flu has killed very many, from the 50,000,000+ in the 1918 pandemic, to the 700,000ish that it kills each year nowadays.
And then there are the combination viruses:
Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
So, why are some people more susceptible?
Firstly, some people are simply immunocompromised. This means for example that:
- perhaps they have an inflammatory/autoimmune disease of some kind (e.g. lupus, rheumatoid arthritis, type 1 diabetes), or…
- perhaps they are taking immunosuppressants for some reason (e.g. because they had an organ transplant), or…
- perhaps they have a primary infection that leaves them vulnerable to secondary infections. Most infections will do this to some degree or another, but some are worse for it than others; untreated HIV is a clear example. The HIV itself may not kill people, but (if untreated) the resultant AIDS will leave a person open to being killed by almost any passing opportunistic pathogen. Pneumonia of various kinds being high on the list, but it could even be something as simple as the common cold, without a working immune system to fight it.
See also: How To Prevent (Or Reduce) Inflammation
And for that matter, since pneumonia is a very common last-nail-in-the-coffin secondary infection (especially: older people going into hospital with one thing, getting a secondary infection and ultimately dying as a result), it’s particularly important to avoid that, so…
See also: Pneumonia: What We Can & Can’t Do About It
Secondly, some people are not immunocompromised per the usual definition of the word, but their immune system is, arguably, compromised.
Cortisol, the stress hormone, is an immunosuppressant. We need cortisol to live, but we only need it in small bursts here and there (such as when we are waking up the morning). When high cortisol levels become chronic, so too does cortisol’s immunosuppressant effect.
Top things that cause elevated cortisol levels include:
- Stress
- Alcohol
- Smoking
Thus, the keys here are to 1) not smoke 2) not drink, ideally, or at least keep consumption low, but honestly even one drink will elevate cortisol levels, so it’s better not to, and 3) manage stress.
See also: Lower Your Cortisol! (Here’s Why & How)
Other modifiable factors
Being aware of infection risk and taking steps to reduce it (e.g. avoiding being with many people in confined indoor places, masking as appropriate, handwashing frequently) is a good preventative strategy, along with of course getting any recommended vaccines as they come available.
What if they fail? How can we boost the immune system?
We talked about not sabotaging the immune system, but what about actively boosting it? The answer is yes, we certainly can (barring serious medical reasons why not), as there are some very important lifestyle factors too:
Beyond Supplements: The Real Immune-Boosters!
One final last-line thing…
Since if we do get an infection, it’s better to know sooner rather than later… A recent study shows that wearable activity trackers can (if we pay attention to the right things) help predict disease, including highlighting COVID status (positive or negative) about as accurately (88% accuracy) as rapid screening tests. Here’s a pop-science article about it:
Wearable activity trackers show promise in detecting early signals of disease
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Creatine’s Brain Benefits Increase With Age
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Creatine is generally thought of as a body-building supplement, and for most young people, that’s all it is. But with extra years come extra advantages, and creatine starts to confer cognitive benefits. Dr. Brad Stanfield shares the science:
What the science says
Although 95% of creatine is stored in muscles, 5% is found in the brain, where it helps produce energy needed for brain processes (and that’s a lot of energy—about 20% of our body’s metabolic base rate is accounted for by our brain).
In this video, Dr. Stanfield shares studies showing creatine improving memory, especially in older adults—and also in vegetarians/vegans, since creatine is found in meat (just like in our own bodies, which are also made of meat) and not in plants. On the meta-analysis level, a systematic review concluded that creatine supplementation indeed improves memory, with stronger effects observed in older adults.
Dr. Stanfield also addresses the safety concerns about creatine, which, on balance, are not actually supported by the science (of course, always consult your own doctor to be sure, as your case could vary).
As for dosage, 5g/day is recommended. For more on all of this plus links to the studies cited, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Creatine: Very Different For Young & Old People
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
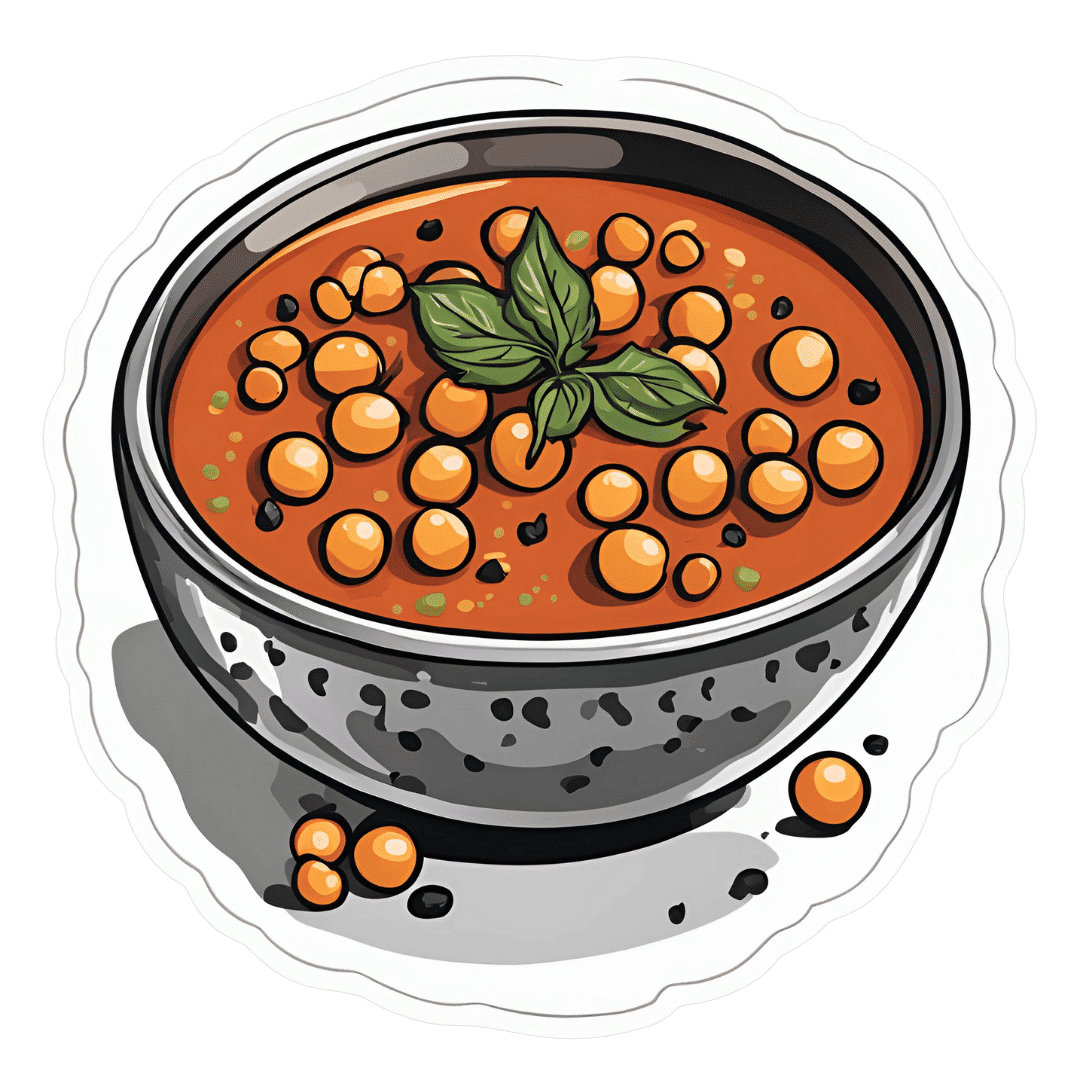
Gut-Healthy Sunset Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So-called for its gut-healthy ingredients, and its flavor profile being from the Maghreb (“Sunset”) region, the western half of the N. African coast.
You will need
- 1 can chickpeas (do not drain)
- 1 cup low-sodium vegetable stock
- 1 small onion, finely chopped
- 1 carrot, finely chopped
- 2 tbsp sauerkraut, drained and chopped (yes, it is already chopped, but we want it chopped smaller so it can disperse evenly in the soup)
- 2 tbsp tomato paste
- 1 tbsp harissa paste (adjust per your heat preference)
- 1 tbsp ras el-hanout
- ¼ bulb garlic, crushed
- Juice of ½ lemon
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
- Optional: herb garnish; we recommend cilantro or flat-leaf parsley
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a sauté pan or similar (something suitable for combination cooking, as we’ll be frying first and then adding liquids), and fry the onion and carrot until the onion is soft and translucent; about 5 minutes.
2) Stir in the garlic, tomato paste, harissa paste, and ras el-hanout, and fry for a further 1 minute.
3) Add the remaining ingredients* except the lemon juice. Bring to the boil and then simmer for 5 minutes.
*So yes, this includes adding the “chickpea water” also called “aquafaba”; it adds flavor and also gut-healthy fiber in the form of oligosaccharides and resistant starches, which your gut microbiota can use to make short-chain fatty acids, which improve immune function and benefit the health in more ways than we can reasonably mention as a by-the-way in a recipe.
4) Stir in the lemon juice, and serve, adding a herb garnish if you wish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← today’s recipe scored 5/5 of these, plus quite a few more! Remember that ras el-hanout is a spice blend, so if you’re thinking “wait, where’s the…?” then it’s in the ras el-hanout 😉
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← not to be underestimated!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: