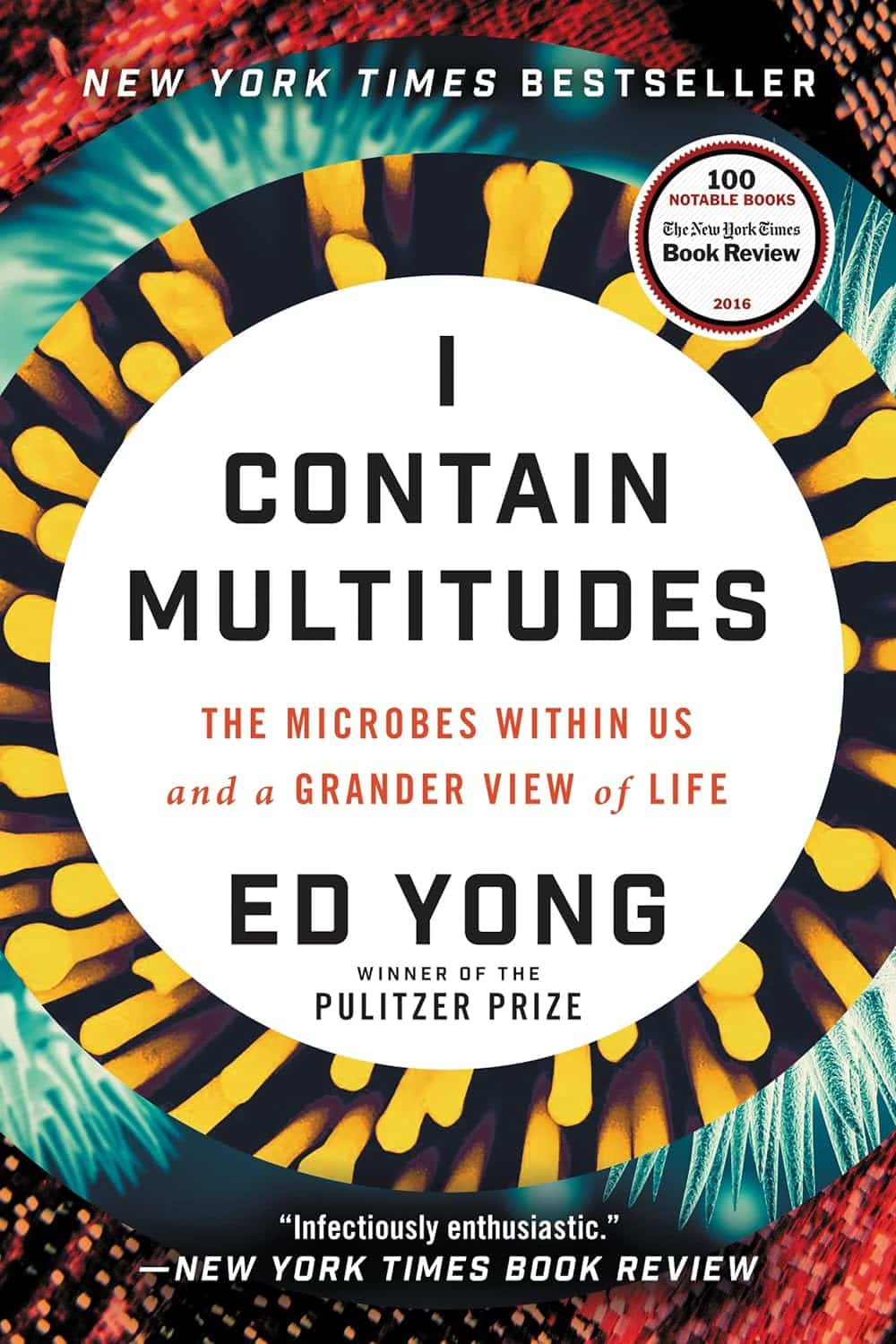
I Contain Multitudes – by Ed Yong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A little while back we reviewed a book (Planet of Viruses) about the role of viruses in our lives, beyond the obvious. Today’s book gives the same treatment to microbes in general—mostly bacteria.
We all know about pathogens, and we all know about gut microbiota and that some (hopefully the majority) there are good for our health. This book covers those things too, but also much more.
Pulitzer Prize-winning science writer Ed Yong takes a big picture view (albeit, of some very small things) and looks at the many ways microbes keep us alive, directly or indirectly. From the microbes that convert certain proteins in breast milk into a form that babies can digest (yes, this means we produce nutrients in breast milk that have been evolved solely to feed that bacterium), to those without which agriculture would simply not work, we’re brought to realize how much our continued existence is contingent on our trillions of tiny friends.
The style throughout is easy-reading pop-science, very accessible. There’s also plenty in terms of practical take-away value, when it comes to adjusting our modern lives to better optimize the benefits we get from microbes—inside and out.
Bottom line: if you’d like to learn about the role of microbes in our life beyond “these ones are pathogens” and “these ones help our digestion”, this is the book for you.
Click here to check out I Contain Multitudes, and learn more about yours and those around you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
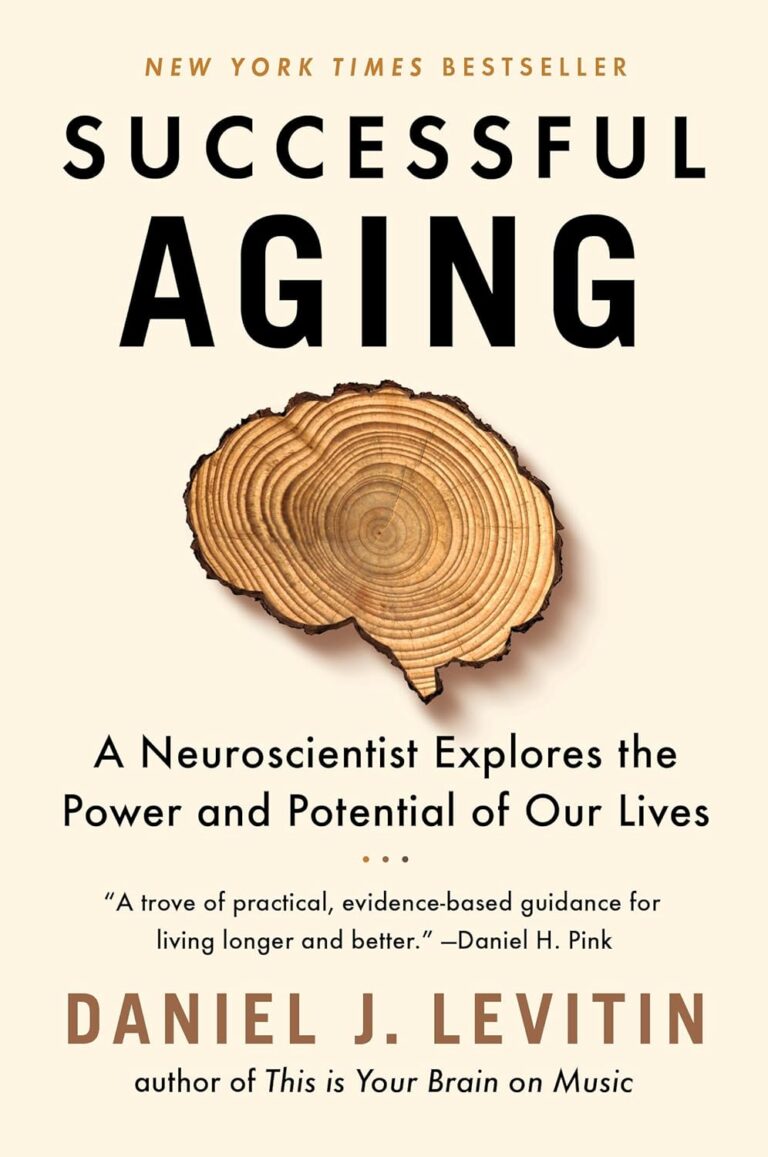
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Eyes for Alzheimer’s Diagnosis: New?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Share This Post

Lycopene’s Benefits For The Gut, Heart, Brain, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Doesn’t Lycopene Do?
Lycopene is an antioxidant carotenoid famously found in tomatoes; it actually appears in even higher levels in watermelon, though. If you are going to get it from tomato, know that cooking improves the lycopene content rather than removing it (watermelon, on the other hand, can be enjoyed as-is and already has the higher lycopene content).
Antioxidant properties
Let’s reiterate the obvious first, for the sake of being methodical and adding a source. Lycopene is a potent antioxidant with multiple health benefits:
Lycopene: A Potent Antioxidant with Multiple Health Benefits
…and as such, it does all the things you might reasonably expect and antioxidant to do. For example…
Anti-inflammatory properties
In particular, it regulates macrophage activity, reducing inflammation while improving immune response:
Lycopene Regulates Macrophage Immune Response through the Autophagy Pathway Mediated by RIPK1
As can be expected of most antioxidants and anti-inflammatory agents, it also has…
Anticancer properties
Scientific papers tend to be “per cancer type”, so we’re just going to give one example, but there’s pretty much evidence for its utility against most if not all types of cancer. We’re picking prostate cancer though, as it’s one that’s been studied the most in the context of lycopene intake—in this study, for example, it was found that men who enjoyed at least two servings of lycopene-rich tomato sauce per week were 30% less likely to develop prostate cancer than those who didn’t:
Dietary lycopene intake and risk of prostate cancer defined by ERG protein expression
If you’d like to see something more general, however, then check out:
Potential Use of Tomato Peel, a Rich Source of Lycopene, for Cancer Treatment
It also fights Candida albicans
Ok, this is not (usually) so life-and-death as cancer, but reducing our C. albicans content (specifically: in our gut) has a lot of knock-on effects for other aspects of our health, so this isn’t one to overlook:
The title does not make this clear, but yes: this does mean it has an antifungal effect. We mention this because often cellular apoptosis is good for an overall organism, but in this case, it simply kills the Candida.
It’s good for the heart
A lot of studies focus just on triglyceride markers (which lycopene improves), but more tellingly, here’s a 10-year observational study in which diets rich in lycopene were associated to a 17–26% lower risk of heart disease:
Relationship of lycopene intake and consumption of tomato products to incident CVD
…and a 39% overall reduced mortality in, well, we’ll let the study title tell it:
…which means also:
It’s good for the brain
As a general rule of thumb, what’s good for the heart is good for the brain (because the brain needs healthy blood flow to stay healthy, and is especially vulnerable when it doesn’t get that), and in this case that rule of thumb is also borne out by the post hoc evidence, specifically yielding a 31% decreased incidence of stroke:
Dietary and circulating lycopene and stroke risk: a meta-analysis of prospective studies
Is it safe?
As a common food product, it is considered very safe.
If you drink nothing but tomato juice all day for a long time, your skin will take on a reddish hue, which will go away if you stop getting all your daily water intake in tomato juice.
In all likelihood, even if you went to extremes, you would get sick from the excess of vitamin A (generally present in the same foods) sooner than you’d get sick from the excess of lycopene.
Want to try some?
We don’t sell it, and also we recommend simply enjoying tomatoes, watermelons, etc, but if you do want a supplement, here’s an example product on Amazon
Enjoy!
Share This Post

How community health screenings get more people of color vaccinated
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
U.S. preventive health screening rates dropped drastically at the height of the COVID-19 pandemic. They have yet to go back to pre-pandemic levels, especially for Black and Latine communities.
Screenings, or routine medical checkups, are important ways to avoid and treat disease. They’re key to finding problems early on and can even help save people’s lives.
Community health workers say screenings are also a key to getting more people vaccinated. Screening fairs provide health workers the chance to build rapport and trust with the communities they serve, while giving their clients the chance to ask questions and get personalized recommendations according to their age, gender, and family history.
But systemic barriers to health care can often keep people from marginalized communities from accessing recommended screenings, exacerbating racial health disparities.
Public Good News spoke with Dr. Marie-Jose Francois, president and chief executive officer, and April Johnson, outreach coordinator, at the Center for Multicultural Wellness and Prevention (CMWP), in Central Florida, to learn how they promote the benefits of screening and leverage screenings for vaccination outreach among their diverse communities.
Here’s what they said.
[Editor’s note: This content has been edited for clarity and length.]
PGN: What is CMWP’s mission? How does vaccine outreach fit into the work you do in the communities you serve?
Dr. Marie-Jose Francois: Since 1995, our mission has been to enhance the health, wellness, and quality of life for diverse populations in Central Florida. At the beginning, our main focus was education, wellness, and screening for HIV/AIDS, and we continue to do case management for HIV screening and testing.
When the issue of COVID-19 came into the picture, we included COVID-19 information and education and stressed the importance of screening and receiving vaccinations during all of our outreach activities.
We try to meet the community where they are. Because there is so much misconception—and taboo—in regard to immunization.
April Johnson: So our job is to disperse accurate information. And how we do that is we go into rural communities. We build partnerships with local apartment complexes, hair salons, nail salons, laundromats, and provide a little community engagement, where people just hang out in different areas.
We build gatekeepers in those communities because you first have to get in there. You have to know that they trust you. Being in this field for about 30 years, I’ve [learned that] flexibility is key. Because sometimes you can’t get them from 9 to 5, or [from] Monday through Friday. So, you have to be very flexible in doing the outreach portion in order to get what you need.
I’ve built collaborations with senior citizen centers, community centers, schools, clinics, churches in Orlando and [in] different areas in Orange, Osceola, Seminole, and Lake counties. And we also partner with other community-based organizations to try to make it like a one-stop shop. So, partnership is a big thing.
PGN: How do you promote the importance of preventive screenings in the communities you serve?
M.F.: We try to make them view their health in a more comprehensive way, for them to understand the importance of screening. [That] self care is key, and for them to not be afraid.
We empower them to know what to ask when they go to the doctor. We ask them, ‘Do you know your status? Do you know your numbers?’
For example, if you go to the doctor, do you know your blood pressure? If you’re diabetic? Do you know your hemoglobin (A1C)? Do you know your cholesterol levels?
And now, [we also ask them]: ‘Have you received your flu shot for the year? Have you received all of your vaccine doses for COVID-19?’ We are even adding the mpox vaccine now, based on risk factors.
[We recommend they] ask their provider. For women, [we ask], ‘When do you need to have your mammogram?’ For the men, ‘You need to ask about your PSA and also about when and when to have your colonoscopy based on your age.’
We also try to explain to the community that the more they know their family history, the more they can engage in their own health. Because sometimes you have mom and dad who have a history of cancer. They have a history of diabetes or blood pressure—and they don’t talk to their children. So, we try to [recommend they] talk to their children. Your own family needs to know what’s going on so they can be proactive in their screenings.
PGN: What strategies or methods have you found most effective in getting people screened?
M.F.: Not everybody wants to be screened, not everybody wants to receive vaccines.
But with patience, just give them the facts. It goes right back to education, people have to be assured.
When you talk to them about COVID, or even HIV, you may hear them say, ‘Oh, I don’t see myself at risk for HIV.’ But we have to repeat to them that the more they get screened to make sure they’re OK, the better it is for them. ‘The more you use condoms, [the] safer it is for you.’
In Haitian culture, they listen to the radio. So we use the radio as a tool to educate and deliver information [to] get vaccinated, wash your hands. ‘If you’re coughing, cover your mouth. If you have a fever, wear your masks. Call your doctor.’
In our target population, we have people who have chronic conditions. We have people with HIV. So, we have to motivate them to receive the flu vaccine, to receive the COVID vaccine, to receive that RSV [vaccine], or to get the mpox vaccine. We have people with diabetes, high blood pressure, high cholesterol, depressed immune systems. We have people with lupus, we have people with sickle cell disease.
So, this is a way to [ensure that] whomever you’re talking to one-on-one understands the value of being safe.
This article first appeared on Public Good News and is republished here under a Creative Commons license.

Share This Post
Related Posts

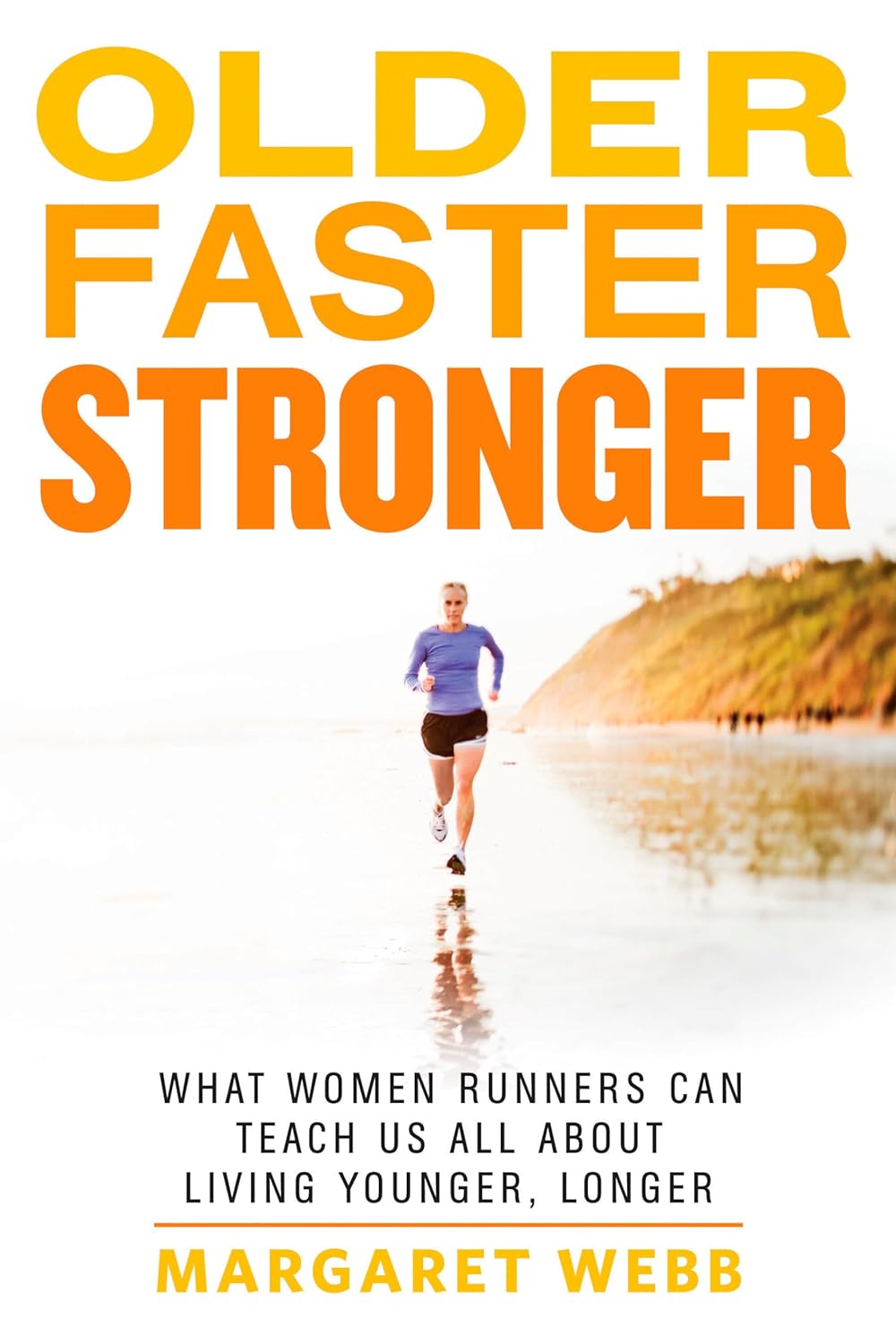
Older, Faster, Stronger – by Margaret Webb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, now in her 60s, made it her mission in her 50s to become the best runner she could. Before that, she’d been a keen runner previously, but let things slip rather in her 40s. But the book’s not about her 40s, it’s about her 50s and onwards, and other female runners in their 50s, 60s, 70s, 80s, and even 90s.
There’s a lot of this book that’s about people’s individual stories, and those should certainly be enough to prompt almost any reader that “if they can do it, I can”.
A lot, meanwhile, is about health and exercise science, training methods, and what has worked for various later-life athletes, including the author. So, it’s also partway instruction manual, with plenty of reference to science and medical considerations too.
Bottom line: sometimes, life throws us challenges. Sometimes, the best response is “Yeah? Bet” and surprise everyone.
Click here to check out Older, Faster, Stronger, and become all those cool things!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

The Mental Health First-Aid That You’ll Hopefully Never Need
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Take Your Mental Health As Seriously As General Health!
Sometimes, health and productivity means excelling—sometimes, it means avoiding illness and unproductivity. Both are essential, and today we’re going to tackle some ground-up stuff. If you don’t need it right now, great; we suggest to read it for when and if you do. But how likely is it that you will?
- One in four of us are affected by serious mental health issues in any given year.
- One in five of us have suicidal thoughts at some point in our lifetime.
- One in six of us are affected to at least some extent by the most commonly-reported mental health issues, anxiety and depression, in any given week.
…and that’s just what’s reported, of course. These stats are from a UK-based source but can be considered indicative generally. Jokes aside, the UK is not a special case and is not measurably worse for people’s mental health than, say, the US or Canada.
While this is not an inherently cheery topic, we think it’s an important one.
Depression, which we’re going to focus on today, is very very much a killer to both health and productivity, after all.
One of the most commonly-used measures of depression is known by the snappy name of “PHQ9”. It stands for “Patient Health Questionnaire Nine”, and you can take it anonymously online for free (without signing up for anything; it’s right there on the page already):
Take The PHQ9 Test Here! (under 2 minutes, immediate results)
There’s a chance you took that test and your score was, well, depressing. There’s also a chance you’re doing just peachy, or maybe somewhere in between. PHQ9 scores can fluctuate over time (because they focus on the past two weeks, and also rely on self-reports in the moment), so you might want to bookmark it to test again periodically. It can be interesting to track over time.
In the event that you’re struggling (or: in case one day you find yourself struggling, or want to be able to support a loved one who is struggling), some top tips that are useful:
Accept that it’s a medical condition like any other
Which means some important things:
- You/they are not lazy or otherwise being a bad person by being depressed
- You/they will probably get better at some point, especially if help is available
- You/they cannot, however, “just snap out of it”; illness doesn’t work that way
- Medication might help (it also might not)
Do what you can, how you can, when you can
Everyone knows the advice to exercise as a remedy for depression, and indeed, exercise helps many. Unfortunately, it’s not always that easy.
Did you ever see the 80s kids’ movie “The Neverending Story”? There’s a scene in which the young hero Atreyu must traverse the “Swamp of Sadness”, and while he has a magical talisman that protects him, his beloved horse Artax is not so lucky; he slows down, and eventually stops still, sinking slowly into the swamp. Atreyu pulls at him and begs him to keep going, but—despite being many times bigger and stronger than Atreyu, the horse just sinks into the swamp, literally drowning in despair.
See the scene: The Neverending Story movie clip – Artax and the Swamp of Sadness (1984)
Wow, they really don’t make kids’ movies like they used to, do they?
But, depression is very much like that, and advice “exercise to feel less depressed!” falls short of actually being helpful, when one is too depressed to do it.
If you’re in the position of supporting someone who’s depressed, the best tool in your toolbox will be not “here’s why you should do this” (they don’t care; not because they’re an uncaring person by nature, but because they are physiologically impeded from caring about themself at this time), but rather:
“please do this with me”
The reason this has a better chance of working is because the depressed person will in all likelihood be unable to care enough to raise and/or maintain an objection, and while they can’t remember why they should care about themself, they’re more likely to remember that they should care about you, and so will go with your want/need more easily than with their own. It’s not a magic bullet, but it’s worth a shot.
What if I’m the depressed person, though?
Honestly, the same, if there’s someone around you that you do care about; do what you can to look after you, for them, if that means you can find some extra motivation.
But I’m all alone… what now?
Firstly, you don’t have to be alone. There are free services that you can access, for example:
- US: https://nami.org/help
- Canada: https://www.wellnesstogether.ca/en-CA
- UK: https://www.samaritans.org/
…which varyingly offer advice, free phone services, webchats, and the like.
But also, there are ways you can look after yourself a little bit; do the things you’d advise someone else to do, even if you’re sure they won’t work:
- Take a little walk around the block
- Put the lights on when you’re not sleeping
- For that matter, get out of bed when you’re not sleeping. Literally lie on the floor if necessary, but change your location.
- Change your bedding, or at least your clothes
- If changing the bedding is too much, change just the pillowcase
- If changing your clothes is too much, change just one item of clothing
- Drink some water; it won’t magically cure you, but you’ll be in slightly better order
- On the topic of water, splash some on your face, if showering/bathing is too much right now
- Do something creative (that’s not self-harm). You may scoff at the notion of “art therapy” helping, but this is a way to get at least some of the lights on in areas of your brain that are a little dark right now. Worst case scenario is it’ll be a distraction from your problems, so give it a try.
- Find a connection to community—whatever that means to you—even if you don’t feel you can join it right now. Discover that there are people out there who would welcome you if you were able to go join them. Maybe one day you will!
- Hiding from the world? That’s probably not healthy, but while you’re hiding, take the time to read those books (write those books, if you’re so inclined), learn that new language, take up chess, take up baking, whatever. If you can find something that means anything to you, go with that for now, ride that wave. Motivation’s hard to come by during depression and you might let many things slide; you might as well get something out of this period if you can.
If you’re not depressed right now but you know you’re predisposed to such / can slip that way?
Write yourself instructions now. Copy the above list if you like.
Most of all: have a “things to do when I don’t feel like doing anything” list.
If you only take one piece of advice from today’s newsletter, let that one be it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Severe Complications for Pregnant Veterans Nearly Doubled in the Last Decade, a GAO Report Finds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Post-Roe America:Abortion Access Divides the Nation
After the Supreme Court overturned Roe v. Wade, ending nearly 50 years of federal protection for abortion, some states began enforcing strict abortion bans while others became new havens for the procedure. ProPublica is investigating how sweeping changes to reproductive health care access in America are affecting people, institutions and governments.
Over the past decade, the rate of veterans suffering severe pregnancy complications has risen dramatically, a new federal report found.
Veterans have raced to the hospital with dangerous infections, kidney failure, aneurysms or blood loss. They’ve required hysterectomies, breathing machines and blood transfusions to save their lives. Between 2011 and 2020, 13 veterans died after such complications.
The report found that among people getting health care benefits through the Department of Veterans Affairs, the rate of severe complications nearly doubled during that time, from about 93 per 10,000 hospitalizations in 2011 to just over 184 per 10,000 hospitalizations in 2020. Black veterans had the highest rates.
The report, which was put together by the Government Accountability Office, also made recommendations for reducing the problem, which focus on conducting more routine screenings throughout pregnancy and in the postpartum period.
“It is imperative that the VA help ensure veterans have the healthiest pregnancy outcomes possible,” the report said, highlighting the increasing number of veterans using the agency’s maternity benefits as well as the troublesome complication rates faced by Black women.
The report’s findings are an unfortunate trend, said Alyssa Hundrup, director of health care at the GAO. The office analyzed data on 40,000 hospitalizations related to deliveries paid for by the VA. It captures a time period before 21 states banned or greatly restricted abortion and the military was thrust into a political battle over whether it would pay for active service members to travel for abortion care if a pregnancy was a risk to their health.
Hundrup, who led the review, said the analysis included hospital records from days after delivery to a year postpartum. The report was mandated after Congress passed a law in 2021 that aimed to address the maternal health crisis among veterans. The law led to a $15 million investment in maternity care coordination programs for veterans.
The report recommended that the VA analyze and collect more data on severe complications as well as data on the mental health, race and ethnicity of veterans who experience complications to understand the causes behind the increase and the reasons for the disparity. The report also states that oversight is needed to ensure screenings are being completed.
Studies show there’s a connection between mental health conditions and pregnancy-related complications, VA officials said.
The report recommended expanding the screening questions that providers ask patients at appointments to glean more information about their mental health, including anxiety and PTSD symptoms. It urged the VA to review the data more regularly.
“You don’t know what you don’t measure,” Hundrup said in an interview with ProPublica.
The VA health system, which historically served a male population, does not provide maternity care at its facilities. Instead, the agency has outsourced maternity care. But when patients were treated by those providers, the VA failed to track whether they were getting screened for other health issues and mental health problems.
Officials hope the improved data collection will help the VA study underlying issues that may lead to complications. For example, do higher rates of anxiety have a connection to rates of high blood pressure in pregnant people?
VA officials are working with a maternal health review committee to monitor the data as it is gathered. The agency recently conducted its first review of data going back five years about pregnancy-related complications, said Dr. Amanda Johnson, acting head of the VA’s Office of Women’s Health, who is overseeing the implementation of the report’s recommendations.
The VA has created a dashboard to monitor pregnant veterans’ health outcomes. The VA’s data analysis team will also examine the impact of veterans’ ages on complications and whether they differ for people who live in urban and rural areas.
VA officials will begin to review mental health screenings conducted by maternal care coordinators in March. The coordinators advocate for veterans, helping them between health care visits, whether their providers are inside or outside the VA.
Johnson said that reducing racial and ethnic disparities is a priority for the agency. In 2018, ProPublica published “Lost Mothers,” a series that shed light on the country’s maternal health crisis. Studies have shown that in the general population, Black women are three times more likely than white women to die from pregnancy-related complications. While deaths made up only a small portion of the bad outcomes for Black veterans cited in the report, VA care could not spare them from elevated rates of severe complications. Johnson said the maternal health crisis also persists within the VA.
“There is a disparity,” Johnson said. “We are not immune to that.”
Research shows pregnant people who have used the VA’s coverage have higher rates of trauma and mental conditions that can increase their risks of complications and bad outcomes.
This may be because many people who join the military enter it having already faced trauma, said Dr. Laura Miller, a psychiatrist and the medical director of reproductive mental health at the VA.
She said veterans with PTSD have higher rates of complications such as preeclampsia, a potentially fatal condition related to high blood pressure, gestational diabetes and postpartum depression. If untreated during pregnancy, depression also increases the likelihood of preterm birth and lingering problems for babies.
Hundrup said she hopes this proactive work will improve maternal health.
“We want these numbers trending in the other direction,” Hundrup said.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: