The Missing Links – by Drs Phillip Meade & Laura Gallagher
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book looks at what goes wrong in projects, why it goes wrong, and how to fill in those “missing links” so that we don’t make the same mistakes that failed projects before us have made.
Using the Columbia crash (and NASA’s subsequent investigation and organizational overhaul) as an example, Drs Meade and Gallagher take us through the steps to apply NASA’s resultant model to our own projects.
The book is aimed squarely at business management, but the lessons within are applicable to any kind of project management, whether the project in question is a Fortune 500 merger or a new patio.
Bottom line is as per the blurb: “you don’t have to be a rocket scientist to apply this model to your organization to create a culture of accountability, inclusivity, and productivity.”
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dr. Greger’s Anti-Aging Eight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
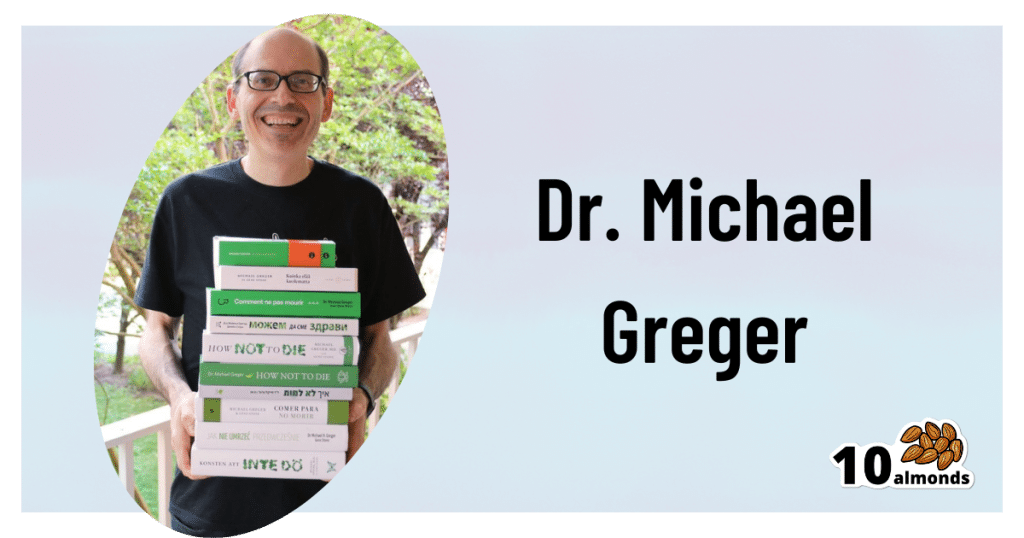
Dr. Greger’s Anti-Aging Eight
This is Dr. Michael Greger. We’ve featured him before: Brain Food? The Eyes Have It!
This time, we’re working from his latest book, the excellent “How Not To Age”, which we reviewed all so recently. It is very information-dense, but we’re going to be focussing on one part, his “anti-aging eight”, that is to say, eight interventions he rates the most highly to slow aging in general (other parts of the book pertained to slowing eleven specific pathways of aging, or preserving specific bodily functions against aging, for example).
Without further ado, his “anti-aging eight” are…
- Nuts
- Greens
- Berries
- Xenohormesis & microRNA manipulation
- Prebiotics & postbiotics
- Caloric restriction / IF
- Protein restriction
- NAD+
As you may have noticed, some of these are things might appear already on your grocery shopping list; others don’t seem so “household”. Let’s break them down:
Nuts, greens, berries
These are amongst the most nutrient-dense and phytochemical-useful parts of the diet that Dr. Greger advocates for in his already-famous “Dr. Greger’s Daily Dozen”.
For brevity, we’ll not go into the science of these here, but will advise you: eat a daily portion of nuts, a daily portion of berries, and a couple of daily portions of greens.
Xenohormesis & microRNA manipulation
You might, actually, have these on your grocery shopping list too!
Hormesis, you may recall from previous editions of 10almonds, is about engaging in a small amount of eustress to trigger the body’s self-strengthening response, for example:
Xenohormesis is about getting similar benefits, second-hand.
For example, plants that have been grown to “organic” standards (i.e. without artificial pesticides, herbicides, fertilizers) have had to adapt to their relatively harsher environment by upping their levels of protective polyphenols and other phytochemicals that, as it turns out, are as beneficial to us as they are to the plants:
Hormetic Effects of Phytochemicals on Health and Longevity
Additionally, the flip side of xenohormesis is that some plant compounds can themselves act as a source of hormetic stress that end up bolstering us. For example:
In essence, it’s not just that it has anti-oxidant effect; it also provides a tiny oxidative-stress immunization against serious sources of oxidative stress—and thus, aging.
MicroRNA manipulation is, alas, too complex to truly summarize an entire chapter in a line or two, but it has to do with genetic information from the food that we eat having a beneficial or deleterious effect to our own health:
Diet-derived microRNAs: unicorn or silver bullet?
A couple of quick takeaways (out of very many) from Dr. Greger’s chapter on this is to spring for the better quality olive oil, and skip the cow’s milk:
- Impact of Phenol-Enriched Virgin Olive Oils on the Postprandial Levels of Circulating microRNAs Related to Cardiovascular Disease
- MicroRNA exosomes of pasteurized milk: potential pathogens of Western diseases
Prebiotics & Postbiotics
We’re short on space, so we’ll link you to a previous article, and tell you that it’s important against aging too:
Making Friends With Your Gut (You Can Thank Us Later)
An example of how one of Dr. Greger’s most-recommended postbiotics helps against aging, by the way:
- The mitophagy activator urolithin A is safe and induces a molecular signature of improved mitochondrial and cellular health in humans
- Urolithin A improves muscle strength, exercise performance, and biomarkers of mitochondrial health in a randomized trial in middle-aged adults
(Urolithin can be found in many plants, and especially those containing tannins)
See also: How to Make Urolithin Postbiotics from Tannins
Caloric restriction / Intermittent fasting
This is about lowering metabolic load and promoting cellular apoptosis (programmed cell death; sounds bad; is good) and autophagy (self-consumption; again, sounds bad; is good).
For example, he cites the intermittent fasters’ 46% lower risk of dying in the subsequent years of follow-up in this longitudinal study:
For brevity we’ll link to our previous IF article, but we’ll revisit caloric restriction in a main feature on of these days:
Fasting Without Crashing? We sort the science from the hype!
Dr. Greger favours caloric restriction over intermittent fasting, arguing that it is easier to adhere to and harder to get wrong if one has some confounding factor (e.g. diabetes, or a medication that requires food at certain times, etc). If adhered to healthily, the benefits appear to be comparable for each, though.
Protein restriction
In contrast to our recent main feature Protein vs Sarcopenia, in which that week’s featured expert argued for high protein consumption levels, protein restriction can, on the other hand, have anti-aging effects. A reminder that our body is a complex organism, and sometimes what’s good for one thing is bad for another!
Dr. Greger offers protein restriction as a way to get many of the benefits of caloric restriction, without caloric restriction. He further notes that caloric restriction without protein restriction doesn’t decrease IGF-1 levels (a marker of aging).
However, for FGF21 levels (these are good and we want them higher to stay younger), what matters more than lowering proteins in general is lowering levels of the amino acid methionine—found mostly in animal products, not plants—so the source of the protein matters:
For example, legumes deliver only 5–10% of the methionine that meat does, for the same amount of protein, so that’s a factor to bear in mind.
NAD+
This is about nicotinamide adenine dinucleotide, or NAD+ to its friends.
NAD+ levels decline with age, and that decline is a causal factor in aging, and boosting the levels can slow aging:
Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
Can we get NAD+ from food? We can, but not in useful quantities or with sufficient bioavailability.
Supplements, then? Dr. Greger finds the evidence for their usefulness lacking, in interventional trials.
How to boost NAD+, then? Dr. Greger prescribes…
Exercise! It boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
Another study on resistance training found the same 127% boost:
Take care!
Share This Post
-
Healing Your Gut: Anastasia’s Journey and Tips
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anastasia Gurova shares her inspiring journey from chronic gut issues to vibrant health.
A Personal Journey to Gut Health
In the below video, Anastasia shares her long struggle with gut problems, including SIBO, IBS, and gastritis. She talks about ending up in the hospital with severe bloating, only to find that a range of medical approaches didn’t provide her with any lasting relief. This led her to explore the importance of the microbiome and its crucial role in gut health, which is what we’ll be focusing on in this overview.
Key Insights and Tips
The most valuable parts of Anastasia’s story for 10almonds readers are, in our opinion, the solutions she discovered to her gut issues. You’ll have to watch her video to discover all of them, but here are some of our favorites:
- Reintroduce Whole Grains and Legumes: Despite the popularity of grain-free diets, Anastasia found significant improvements in her gut health by adding whole grains like quinoa, oats, and buckwheat back into her diet. These foods provide essential fibers that feed beneficial gut bacteria.
- Soaking and Fermenting Foods: To make grains and legumes more digestible, Anastasia recommends soaking them overnight. This is similar to the common technique people use on oats. She also includes fermented foods like sauerkraut, kimchi, and yogurt in her diet, which introduce beneficial bacteria to the gut.
- Resistant Starches: Foods like cooked and cooled rice, potatoes, and green bananas contain resistant starches that promote healthy gut bacteria. Anastasia emphasizes incorporating these into meals to support gut health.
- Mindful Eating: Anastasia found that taking time to chew food thoroughly and savor each bite helped improve her digestion. She avoids distractions like TV while eating and pays attention to the textures and flavors of her meals.
- Avoid Overly Restrictive Diets: Anastasia warns against overly restrictive diets like keto and strict SIBO diets that cut out all carbs and fiber. These can worsen gut health by starving beneficial bacteria.
That’s Only The Beginning
Anastasia’s video goes far beyond what we’ve covered in this short introduction; she provides a detailed look at the steps she took, from dietary changes to lifestyle adjustments, and offers tips that anyone can apply. Plus, she explains the science behind these changes, which, of course, we love.
Enjoy the video! (It would be remiss for us to not bring up our general intro to gut health, or our more specific article on the gut-brain connection)
Good luck on your gut-health journey!
Share This Post
-
The Sprout Book – by Doug Evans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sprouting seeds are more nutritious than most people think, and “seeds” is also a much broader category than people think. Beyond even chia and sunflower and such, this book bids us remember that onions do not just appear on supermarket shelves fully formed (to give just one example of many); most plants come from seeds and of those, most can be usefully sprouted.
The author, most well-known for his tech companies, here is selling us a very low-tech health kick with very little profit to be found except for our health. By sprouting seeds of many kinds at home, we can enjoy powerful superfoods that are not only better than, but also cheaper than, most supplements.
Nor are the benefits of sprouting things marginal; we’re not talking about a 1–10% increase in bioavailable so much as what’s often a 100–1000% increase.
After explaining the science and giving a primer on sprouting things for oneself, there is a wide selection of recipes, but the biggest benefit of the book is in just getting the reader up-and-running with at-home sprouting.
Bottom line: if you like the idea of letting food be your medicine and even like the idea of essentially growing your own food with zero gardening skills, then this is an excellent book for you.
Share This Post
Related Posts
-
Avoiding/Managing Osteoarthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding/Managing Osteoarthritis
Arthritis is the umbrella term for a cluster of joint diseases involving inflammation of the joints, hence “arthr-” (joint) “-itis” (suffix used to denote inflammation).
Inflammatory vs Non-Inflammatory Arthritis
Arthritis is broadly divided into inflammatory arthritis and non-inflammatory arthritis.
Some forms, such as rheumatoid arthritis, are of the inflammatory kind. We wrote about that previously:
See: Avoiding/Managing Rheumatoid Arthritis
You may be wondering: how does one get non-inflammatory inflammation of the joints?
The answer is, in “non-inflammatory” arthritis, such as osteoarthritis, the damage comes first (by general wear-and-tear) and inflammation generally follows as part of the symptoms, rather than the cause.
So the name can be a little confusing. In the case of osteo- and other “non-inflammatory” forms of arthritis, you definitely still want to keep your inflammation at bay as best you can; it’s just not the prime focus.
So, what should we focus on?
First and foremost: avoiding wear-and-tear if possible. Naturally, we all must live our lives, and sometimes that means taking a few knocks, and definitely it means using our joints. An unused joint would suffer just as much as an abused one. But, we can take care of our joints!
We wrote on that previously, too:
See: How To Really Look After Your Joints
New osteoarthritis medication (hot off the press!)
At 10almonds, we try to keep on top of new developments, and here’s a shiny new one from this month:
- Methotrexate to treat hand osteoarthritis with synovitis (12th Oct, clinical trial)
- New research has found an existing drug could help many people with painful hand osteoarthritis (24th Oct, pop-science article about the above, but still written by one of the study authors!)
Note also that Dr. Flavia Cicuttini there talks about what we talked about above—that calling it non-inflammatory arthritis is a little misleading, as the inflammation still occurs.
And finally…
You might consider other lifestyle adjustments to manage your symptoms. These include:
- Exercise—gently, though!
- Rest—while keeping mobility going.
- Mobility aids—if it helps, it helps.
- Go easy on the use of braces, splints, etc—these can offer short-term relief, but at a long term cost of loss of mobility.
- Only you can decide where to draw the line when it comes to that trade-off.
You can also check out our previous article:
See: Managing Chronic Pain (Realistically!)
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Book Of Hormones – by Dr. Shweta Patel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle promising “through every stage of life” is a slight overstatement, as the book barely touches on puberty, but we know that the vast majority of our readers have left that one far behind in the past, so probably this is not such an issue.
Where the book gives more attention is in general adult life, through the years of potential fertility, into menopause and beyond. This means lots about the hormonal fluctuations inherent to the menstrual cycle (both the normal, and the still-quite-commonly abnormal, e.g. in cases of PCOS etc), the before-during-after of pregnancy, and many hormonal matters that are not related to sex hormones, such as stress-related hormones and food-related hormones. As such, the book certainly lives up to its title; it is indeed “the book of hormones”.
The style is light and conversational; we get a lot of lessons in chemistry here, but it never feels like it, and there’s certainly no hard science, just clear and easy explanations.
Bottom line: if you’d like to understand hormones quite comprehensively but in a light-hearted manner, this book is a very pleasant and educational read.
Click here to check out The Book Of Hormones, and understand them!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is HRT? HRT and Hormones Explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In this short video, Dr. Sophie Newton explains how menopausal HRT, sometimes called just MHT, is the use of exogenous (didn’t come from your body) to replace/supplement the endogenous hormones (made in your body) that aren’t being made in the quantities that would result in ideal health.
Bioidentical hormones are, as the name suggests, chemically identical to those made in the body; there is no difference, all the way down to the atomic structure.
People are understandably wary of “putting chemicals into the body”, but in fact, everything is a chemical and those chemicals are also found in your body, just not in the numbers that we might always like.
In the case of hormones, these chemical messengers are simply there to tell cells what to do, so having the correct amount of hormones ensures that all the cells that need to get a certain message, get it.
In the case of estrogen specifically, while it’s considered a sex hormone (and it is), it’s responsible for a lot more than just the reproductive system, which is why many people without correct estrogen levels (such as peri- or post-menopause, though incorrect levels can happen earlier in life for other reasons too) can severely feel their absence in a whole stack of ways.
What ways? More than we can list here, but some are discussed in the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might like our previous main features:
- What Does “Balance Your Hormones” Even Mean?
- What You Should Have Been Told About The Menopause Beforehand
- Menopausal HRT: Bioidentical vs Animal
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: