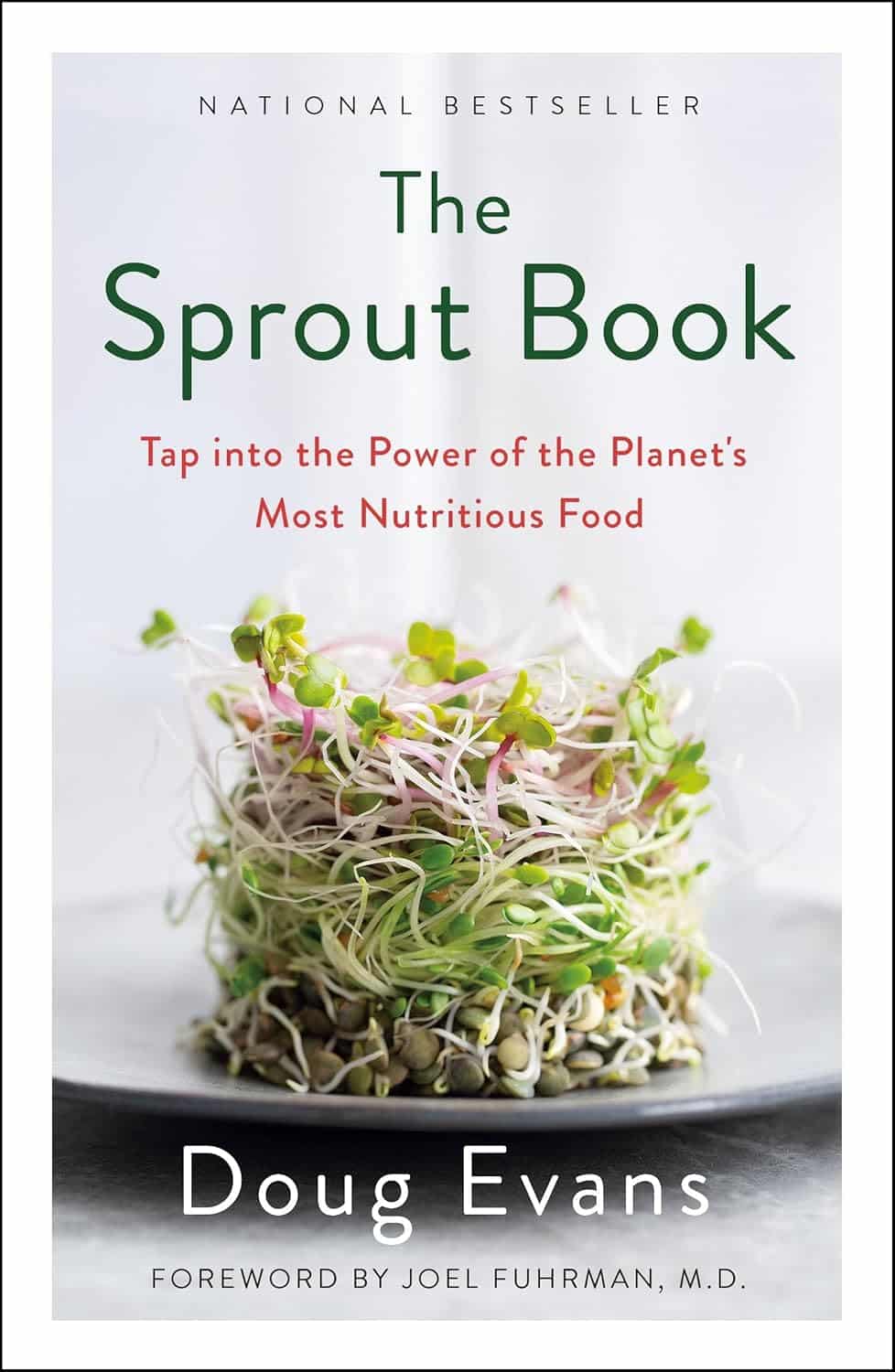
The Sprout Book – by Doug Evans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sprouting seeds are more nutritious than most people think, and “seeds” is also a much broader category than people think. Beyond even chia and sunflower and such, this book bids us remember that onions do not just appear on supermarket shelves fully formed (to give just one example of many); most plants come from seeds and of those, most can be usefully sprouted.
The author, most well-known for his tech companies, here is selling us a very low-tech health kick with very little profit to be found except for our health. By sprouting seeds of many kinds at home, we can enjoy powerful superfoods that are not only better than, but also cheaper than, most supplements.
Nor are the benefits of sprouting things marginal; we’re not talking about a 1–10% increase in bioavailable so much as what’s often a 100–1000% increase.
After explaining the science and giving a primer on sprouting things for oneself, there is a wide selection of recipes, but the biggest benefit of the book is in just getting the reader up-and-running with at-home sprouting.
Bottom line: if you like the idea of letting food be your medicine and even like the idea of essentially growing your own food with zero gardening skills, then this is an excellent book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Omega-3 Fatty Acids Really Do For Us
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Omega-3 Fatty Acids Really Do For Us
Shockingly, we’ve not previously covered this in a main feature here at 10almonds… Mostly we tend to focus on less well-known supplements. However, in this case, the supplement may be well known, while some of its benefits, we suspect, may come as a surprise.
So…
What is it?
In this case, it’s more of a “what are they?”, because omega-3 fatty acids come in multiple forms, most notably:
- Alpha-linoleic acid (ALA)
- Eicosapentaenoic acid (EPA)
- Docosahexanoic acid (DHA)
ALA is most readily found in certain seeds and nuts (chia seeds and walnuts are top contenders), while EPA and DHA are most readily found in certain fish (hence “cod liver oil” being a commonly available supplement, though actually cod aren’t even the best source—salmon and mackerel are better; cod is just cheaper to overfish, making it the cheaper supplement to manufacture).
Which of the three is best, or do we need them all?
There are two ways of looking at this:
- ALA is sufficient alone, because it is a precursor to EPA and DHA, meaning that the body will take ALA and convert it into EPA and DHA as required
- EPA and DHA are superior because they’re already in the forms the body will use, which makes them more efficient
As with most things in health, diversity is good, so you really can’t go wrong by getting some from each source.
Unless you have an allergy to fish or nuts, in which case, definitely avoid those!
What do omega-3 fatty acids do for us, according to actual research?
Against inflammation
Most people know it’s good for joints, as this is perhaps what it’s most marketed for. Indeed, it’s good against inflammation of the joints (and elsewhere), and autoimmune diseases in general. So this means it is indeed good against common forms of arthritis, amongst others:
Read: Omega-3 fatty acids in inflammation and autoimmune disease
Against menstrual pain
Linked to the above-referenced anti-inflammatory effects, omega-3s were also found to be better than ibuprofen for the treatment of severe menstrual pain:
Don’t take our word for it: Comparison of the effect of fish oil and ibuprofen on treatment of severe pain in primary dysmenorrhea
Against cognitive decline
This one’s a heavy-hitter. It’s perhaps to be expected of something so good against inflammation (bearing in mind that, for example, a large part of Alzheimer’s is effectively a form of inflammation of the brain); as this one’s so important and such a clear benefit, here are three particularly illustrative studies:
- Inadequate supply of vitamins and DHA in the elderly: implications for brain aging and Alzheimer-type dementia
- Fish consumption and cognitive decline with age in a large community study
- Fish consumption, long-chain omega-3 fatty acids and risk of cognitive decline or Alzheimer disease
Against heart disease
The title says it all in this one:
But what about in patients who do have heart disease?
Mozaffarian and Wu did a huge meta-review of available evidence, and found that in fact, of all the studied heart-related effects, reducing mortality rate in cases of cardiovascular disease was the single most well-evidenced benefit:
How much should we take?
There’s quite a bit of science on this, and—which is unusual for something so well-studied—not a lot of consensus.
However, to summarize the position of the academy of nutrition and dietetics on dietary fatty acids for healthy adults, they recommend a minimum of 250–500 mg combined EPA and DHA each day for healthy adults. This can be obtained from about 8 ounces (230g) of fatty fish per week, for example.
If going for ALA, on the other hand, the recommendation becomes 1.1g/day for women or 1.6g/day for men.
Want to know how to get more from your diet?
Here’s a well-sourced article about different high-density dietary sources:
Share This Post
-
How Primary Care Is Being Disrupted: A Video Primer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How patients are seeing their doctor is changing, and that could shape access to and quality of care for decades to come.
More than 100 million Americans don’t have regular access to primary care, a number that has nearly doubled since 2014. Yet demand for primary care is up, spurred partly by record enrollment in Affordable Care Act plans. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades.
KFF Health News senior correspondent Julie Appleby breaks down what is happening — and what it means for patients.
More From This Investigation
Primary Care Disrupted
Known as the “front door” to the health system, primary care is changing. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades. KFF Health News looks at what this means for patients.
Credits
Hannah Norman Video producer and animator Oona Tempest Illustrator and creative director KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
The Orchid That Renovates Your Gut (Gently)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Orchid That Renovates Your Gut (Gently)
Dendrobium officinale is an orchid that’s made its way from Traditional Chinese Medicine into modern science.
Read: Traditional Uses, Phytochemistry, Pharmacology, and Quality Control of Dendrobium officinale
To summarize its benefits, we’ll quote from Dr. Paharia’s article featured in our “what’s happening in the health world” section all so recently:
❝Gut microbes process Dendriobium officinale polysaccharides (DOPs) in the colon, producing short-chain fatty acids (SCFAs) and oligosaccharides that alter gut microbial composition and improve human health.
DOPs have been shown to decrease harmful bacteria like E. coli and Staphylococcus while promoting beneficial ones like Bifidobacterium.❞
We don’t stop at secondary sources, though, so we took a look at the science.
Dr. Wu et al. found (we’ll quote directly for these bullet points):
- DOPs have been shown to influence the gut microbiota, such as the abundance of Lactobacillus, Bifidobacterium, Akkermansia, Bacteroides, and Prevotella, and provide different benefits to the host due to structural differences.
- The dietary intake of DOPs has been shown to improve the composition of the gut microbiome and offers new intervention strategies for metabolic diseases such as obesity and type 2 diabetes as well as inflammatory diseases such as chronic obstructive pulmonary disease and colitis.
- Compared to drug therapy, intervention with DOPs is not specific and has a longer intervention duration
This is consistent with previous research on Dendrobium officinale, such as last year’s:
❝DOP significantly increased benign intestinal microbe proportion (Lactobacillus, etc.), but reduced harmful bacteria (Escherichia shigella) (P < 0.05), and significantly increased butyric acid production (P < 0.05)❞
In summary…
Research so far indicates that this does a lot of good for the gut, in a way that can “kickstart” healthier, self-regulating gut microbiota.
As to its further prospects, check out:
Very promising!
Where can I get it?
We don’t sell it, but for your convenience here’s an example product on Amazon
Be warned, it is expensive though!
Share This Post
Related Posts
-
Carrots vs Parsnips – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrots to parsnips, we picked the parsnips.
Why?
There are arguments for both! But we say parsnips win on overall nutritional density.
In terms of macros, parsnips vary quite a lot from region to another, but broadly speaking, parsnips have more carbs and fiber, and/but the ratios are such that carrots have the lower glycemic index. We’ll call this one a win for carrots.
When it comes to vitamins, carrots have more of vitamins A, B2, B3, B6, and choline, while parsnips have more of vitamins B1, B5, B9, C, E, and K. A small win for parsnips here.
In the category of minerals, carrots are not higher in any minerals, while parsnips are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for parsnips.
While the overall vitamin and mineral content puts parsnips ahead, it’s still worth noting that carrots have highly bioavailable megadoses of vitamin A.
Another thing to note is that the glycemic index recorded for both is when peeled and boiled, whereas both of these root vegetables can be enjoyed raw if you wish, which has a much lower GI.
In short, enjoy either or both, but parsnips are the more nutritionally dense overall.
Want to learn more?
You might like to read:
Glycemic Index vs Glycemic Load vs Insulin Index
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
To Err Is Human; To Forgive, Healthy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Forgive (And Why)
There’s an old saying that holding onto a grudge is like drinking poison and expecting the other person to die. If only it were so simple and easy as just choosing to let go!
But it’s not, is it?
When people have wronged us and/or wronged our loved ones, it’s hard to forgive, especially if they have not changed. For that matter, it can be hard to forgive ourselves for mistakes that we made, too.
Either way, “drinking that poison” can be close to literal, in terms of what harboring such anger and resentment can do for our cortisol levels.
So, what to do about it?
If you have a dialogue with the person, our previous article on communication may help a lot.
If you don’t, there are various other angles that can be taken:
The Unsent Letter
You can even send it, if you like, but it’s not the point here. The idea is to write to the person, expressing your grievances. But, (as per the above-linked article on communication) try to focus at least as much on your feelings as their actions. “When you did/said x, I felt y”, etc.
This is important for helping you process your feelings. If you send the letter, it’s also important for the other person to be able to understand your feelings.
Sometimes, we feel the things we do so strongly because we don’t have an outlet for them. Pouring out our emotions in such a fashion, on the other hand, means (to labor the metaphor) they’re no longer bottled up. Even just in and of itself, that can provide us a lot of relief.
And when we the negative emotions are no longer such high pressure, it can be easier to let go of them.
Mindfulness
Following on from the above idea, a good strategy can be simply sitting and feeling everything you need to feel, noticing it without judgement, like a curious observer.
Sometimes what we need is just to be heard, and that starts with hearing ourselves.
Compassion
There’s a Buddhist exercise that involves actively feeling compassion for three people: a loved one, a stranger, and an enemy. Many people report that it’s actually harder to feel compassion for a random stranger, than an enemy. Why? Because we don’t know them; we don’t know what’s good and bad about them in our estimation.
If you’re reading this because you want to be able to gain the peace of being able to forgive someone (even if that someone is yourself), then in at least some respect right now, that person is in the “enemy” category. So how do we unpack that?
To err is human. Everybody screws up sometimes. And also, everyone has a reason (or a complex of reasons) for acting the way they do. This does not mean that those reasons excuse the behavior, but it can explain it.
You don’t get angry at a storm for soaking you through. Even if you might not understand the physics of it in the way a meteorologist might, you understand that there were things that led to that, and you were just in the wrong place at the wrong time.
So why do we get angry at someone else for wronging us? Even if we might not understand the personal background of it in the way their psychologist or therapist might, we (hopefully) understand that there were things that caused them to be the way they were, and we were just in the wrong place at the wrong time.
And ourselves? We probably know, when we made a mistake, why we made it. Maybe we were afraid, insecure, reactive, forgetful, or too focused on some other thing. Whatever it was, we did our best at the time and, apparently, our best wasn’t as good as we’d like.
If we didn’t deserve forgiveness, we wouldn’t be critical of our past selves in the first place.
And, the science is very clear that it’s important for our health for other reasons besides cortisol management, too.
And as for others? They did the best they knew how. Maybe they were afraid, insecure, reactive, forgetful, or too focused on some other thing. Same story, different character.
Remembering that can be key to “accepting the apology we never received”.
Forgiving without forgetting
Developing the ability to forgive is a useful tool for our own mental health. It doesn’t mean we must or even should make ourselves a doormat.
“I forgive you” does not have to mean a clean slate; it means remembering that the thing happened, and just not holding on to the anger/resentment associated with it.
It may be water under the bridge now, but it might have been a devastatingly destructive wave at the time, and continuing to acknowledge truth that is sensible. Just, from a position of peace now, hopefully.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Diet Tips for Crohn’s Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: