Protein vs Sarcopenia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein vs Sarcopenia
This is Dr. Gabrielle Lyon. A medical doctor, she’s board-certified in family medicine, and has also engaged in research and clinical practice in the fields of geriatrics and nutritional sciences.
A quick note…
We’re going to be talking a bit about protein metabolism today, and it’s worth noting that Dr. Lyon personally is vehemently against vegetarianism/veganism, and considers red meat to be healthy.
Scientific consensus on the other hand, holds that vegetarianism and veganism are fine for most people if pursued in an informed and mindful fashion, that white meat and fish are also fine for most people, and red meat is simply not.
If you’d like a recap on the science of any of that:
- Protein: How Much Do We Need, Really?
- Plant vs Animal Protein: Diversity is Key
- Do We Need Animal Products to be Healthy?
Nevertheless, if we look at the science that she provides, the advice is sound when applied to protein in general and without an undue focus on red meat.
How much protein is enough?
In our article linked above, we gave 1–2g/kg/day
Dr. Lyons gives the more specific 1.6g/kg/day for adults older than 40 (this is where sarcopenia often begins!) and laments that many sources offer 0.8g/kg.
To be clear, that “per kilogram” means per kilogram of your bodyweight. For Americans, this means dividing lbs by 2.2 to get the kg figure.
Why so much protein?
Protein is needed to rebuild not just our muscles, but also our bones, joint tissues, and various other parts of us:
We Are Such Stuff As Fish Are Made Of
Additionally, our muscles themselves are important for far more than just moving us (and other things) around.
As Dr. Lyon explains: sarcopenia, the (usually age-related) loss of muscle mass, does more than just make us frail; it also messes up our metabolism, which in turn messes up… Everything else, really. Because everything depends on that.
This is because our muscles themselves use a lot of our energy, and/but also store energy as glycogen, so having less of them means:
- getting a slower metabolism
- the energy that can’t be stored in muscle tissue gets stored somewhere else (like the liver, and/or visceral fat)
So, while for example the correlation between maintaining strong muscles and avoiding non-alcoholic fatty liver disease may not be immediately obvious, it is clear when one follows the metabolic trail to its inevitable conclusion.
Same goes for avoiding diabetes, heart disease, and suchlike, though those things are a little more intuitive.
How can we get so much protein?
It can seem daunting at first to get so much protein if you’re not used to it, especially as protein is an appetite suppressant, so you’ll feel full sooner.
It can especially seem daunting to get so much protein if you’re trying to avoid too many carbs, and here’s where Dr. Lyon’s anti-vegetarianism does have a point: it’s harder to get lean protein without meat/fish.
That said, “harder” does not mean “impossible” and even she acknowledges that lentils are great for this.
If you’re not vegetarian or vegan, collagen supplementation is a good way to make up any shortfall, by the way.
And for everyone, there are protein supplements available if we want them (usually based on whey protein or soy protein)
Anything else we need to do?
Yes! Eating protein means nothing if you don’t do any resistance work to build and maintain muscle. This can take various forms, and Dr. Lyon recommends lifting weights and/or doing bodyweight resistance training (calisthenics, Pilates, etc).
Here are some previous articles of ours, consistent with the above:
- Resistance Is Useful! (Especially As We Get Older)
- Overdone It? How To Speed Up Recovery After Exercise
- How To Do HIIT (Without Wrecking Your Body)
- Exercises To Do (And Ones To Avoid) If You Have Osteoporosis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
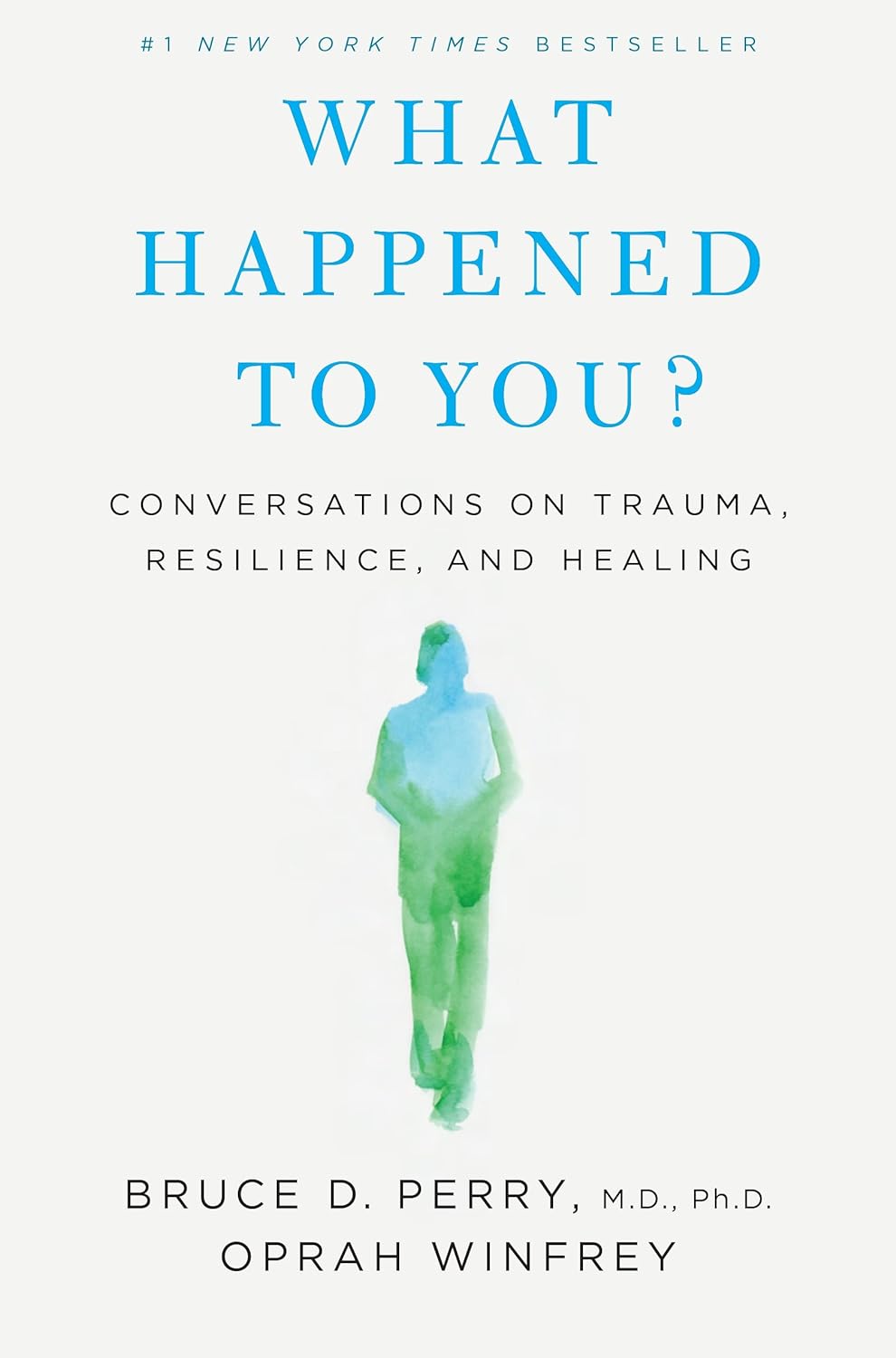
What Happened to You? – by Dr. Bruce Perry and Oprah Winfrey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The very title “What Happened To You?” starts with an assumption that the reader has suffered trauma. This is not just a sample bias of “a person who picks up a book about healing from trauma has probably suffered trauma”, but is also a statistically safe assumption. Around 60% of adults report having suffered some kind of serious trauma.
The authors examine, as the subtitle suggests, these matters in three parts:
- Trauma
- Resilience
- Healing
Trauma can take many forms; sometimes it is a very obvious dramatic traumatic event; sometimes less so. Sometimes it can be a mountain of small things that eroded our strength leaving us broken. But what then, of resilience?
Resilience (in psychology, anyway) is not imperviousness; it is the ability to suffer and recover from things.
Healing is the tail-end part of that. When we have undergone trauma, displayed whatever amount of resilience we could at the time, and now have outgrown our coping strategies and looking to genuinely heal.
The authors present many personal stories and case studies to illustrate different kinds of trauma and resilience, and then go on to outline what we can do to grow from there.
Bottom line: if you or a loved one has suffered trauma, this book may help a lot in understanding and processing that, and finding a way forwards from it.
Click here to check out “What Happened To You?” and give yourself what you deserve.
Share This Post
-
How an Idaho vaccine advocacy org plans its annual goals
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The start of a new year means many nonprofits and community health workers are busy setting goals and reflecting on what’s worked and what hasn’t. For those engaged in vaccine outreach, it also means reflecting on the tools and tactics that help them communicate better with their communities about why vaccines matter.
Across the country, childhood vaccination rates have declined since the COVID-19 pandemic, resulting in a resurgence of preventable diseases like pertussis.
Also known as whooping cough, pertussis has surged in states like Idaho, said Karen Jachimowski Sharpnack, executive director of the Idaho Immunization Coalition, in a conversation with PGN about the organization’s 2025 priorities.
Sharpnack shared how spikes in infectious respiratory illnesses can create opportunities to listen better and understand the nuances of the communities they serve.
Here’s more of what Sharpnack said.
[Editor’s note: The contents of this interview have been edited for length and clarity.]
PGN: Whooping cough cases are up in your state. Can you share an example of how your organization is responding?
Karen Jachimowski Sharpnack: If you look at Treasure Valley and Northern Idaho, the majority of those cases have been reported, and it’s like five times as much as we had the previous year.
So, two things that the Coalition is doing in response: First, we put out radio public service announcements throughout those particular areas about what whooping cough is, how contagious it is, and what you should do if you think your child or anyone you know has it.
Second, we are contacting every school superintendent, principal, school nurse, with a letter from us at the Coalition [to warn about] the whooping cough outbreaks in schools right now. Here’s what the symptoms are, here’s what you can do, and then here’s how you can protect yourself and your families.
It doesn’t mean the health district wouldn’t do it, or the Department of Health and Welfare can’t do it. But from our standpoint, at least we are bringing an awareness to the schools that this is happening.
PGN: How does your organization decide when outreach is needed? How do you take a pulse of your communities’ vaccine attitudes?
K.J.S.: We consistently hold listening sessions. We do them in English and Spanish if we need to, and we go around—and I’m talking about the southern part of the state—and bring people together.
We’ve done adults, we’ve done teenagers, we’ve done college students, we’ve done seniors, we’ve done all age groups.
So, we’ll bring eight or 10 people together, and we’ll spend a couple of hours with them. We feed them and we also pay them to be there. We say, ‘We want to hear from you about what you’re hearing about vaccines, what your views are if you’re vaccinated.’ Anytime, by the way, they can get up and leave and still get paid.
We want to hear what they’re hearing on the ground. And these sessions are extremely informational. For one, we learn about the misinformation that goes out there, like immediately. And two, we’re able to then focus [on how to respond]. If we’re hearing this, what kind of media campaign do we need to get together?
PGN: How do these listening sessions inform your work?
K.J.S.: So, a couple times a year we also pay a professional poller to do a poll. And when we get those results we check them against our listening sessions. We want to see: Are we on target? Are we ahead?
We just finished putting a one-pager together for legislators, so we’re ready to go with the new [legislative] session. We do this poll every year in August-September to know how Idahoans are feeling about vaccines. We get the results in October, because we’re getting ready for the next year.
We actually poll 19-to-64-year-olds, really honing in on questions like, ‘Do you believe vaccines are safe and effective?’ ‘Do you believe that school vaccination rules should still be in place?’
And what’s pretty cool is that two-thirds of Idahoans still believe vaccines are safe and effective, want to keep school rules in place, and believe that the infrastructure systems that we have in place for our vaccine registry should remain the same. Those are important to hear, so this is really good information that we can pull out and do something with.
PGN: Like what?
K.J.S.: Here’s the bottom line. It takes money to do this work, so you have to be able to say what you are going to do with the results.
Doing a poll costs anywhere from $15,000 to $35,000. This is an expensive investment, but we know that the polling is so important to us, along with the time that I have my staff go out and do the listening sessions and get feedback.
We take those results to educate, to talk to our legislators, and advocate for vaccines. We actually do these high-level media campaigns around the state. So, we are actually doing something with the polling. We’re not just sharing the results out.
And then we actually ask, what can we do to make a change? What are we hearing that we need to focus on?
That’s why it’s really important, because we are actually pushing this out for 2025. We know where we’re going in 2025 programmatically with marketing, and we know where we’re going with advocacy work.
We’re not guessing. We’re actually listening to people. And then we’re making really concrete decisions on how we’re going to move the organization forward to be able to help our communities.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Seven Things To Do For Good Lung Health!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
YouTube Channel Wellness Check is challenging us all to do the following things. They’re framing it as a 30-day challenge, but honestly, there’s nothing here that isn’t worth doing for life
Here’s the list:
- Stop smoking (of course, smoking is bad for everything, but the lungs are one of its main areas of destruction)
- Good posture (a scrunched up chest is not the lungs’ best operating conditions!)
- Regular exercise (exercising your body in different ways exercises your lungs in different ways!)
- Monitor air quality (some environments are much better/worse than others, but don’t underestimate household air quality threats either)
- Avoid respiratory infections (shockingly, COVID is not great for your lungs, nor are the various other respiratory infections available)
- Check your O2 saturation levels (pulse oximeters like this one are very cheap to buy and easy to use)
- Prevent mucus and phlegm from accumulating (these things are there for reasons; the top reason is trapping pathogens, allergens, and general pollutants/dust etc; once those things are trapped, we don’t want that mucus there any more!)
Check out the video itself for more detail on each of these items:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might like our article about COPD:
Why Chronic Obstructive Pulmonary Disease (COPD) Is More Likely Than You Think
Take care!
Share This Post
Related Posts
-
Early Detection May Help Kentucky Tamp Down Its Lung Cancer Crisis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anthony Stumbo’s heart sank after the doctor shared his mother’s chest X-ray.
“I remember that drive home, bringing her back home, and we basically cried,” said the internal medicine physician, who had started practicing in eastern Kentucky near his childhood home shortly before his mother began feeling ill. “Nobody wants to get told they’ve got inoperable lung cancer. I cried because I knew what this meant for her.”
Now Stumbo, whose mother died the following year, in 1997, is among a group of Kentucky clinicians and researchers determined to rewrite the script for other families by promoting training and boosting awareness about early detection in the state with the highest lung cancer death rate. For the past decade, Kentucky researchers have promoted lung cancer screening, first recommended by the U.S. Preventive Services Task Force in 2013. These days the Bluegrass State screens more residents who are at high risk of developing lung cancer than any state except Massachusetts — 10.6% of eligible residents in 2022, more than double the national rate of 4.5% — according to the most recent American Lung Association analysis.
The effort has been driven by a research initiative called the Kentucky LEADS (Lung Cancer Education, Awareness, Detection, and Survivorship) Collaborative, which in 2014 launched to improve screening and prevention, to identify more tumors earlier, when survival odds are far better. The group has worked with clinicians and hospital administrators statewide to boost screening rates both in urban areas and regions far removed from academic medical centers, such as rural Appalachia. But, a decade into the program, the researchers face an ongoing challenge as they encourage more people to get tested, namely the fear and stigma that swirl around smoking and lung cancer.
Lung cancer kills more Americans than any other malignancy, and the death rates are worst in a swath of states including Kentucky and its neighbors Tennessee and West Virginia, and stretching south to Mississippi and Louisiana, according to data from the Centers for Disease Control and Prevention.
It’s a bit early to see the impact on lung cancer deaths because people may still live for years with a malignancy, LEADS researchers said. Plus, treatment improvements and other factors may also help reduce death rates along with increased screening. Still, data already shows that more cancers in Kentucky are being detected before they become advanced, and thus more difficult to treat, they said. Of total lung cancer cases statewide, the percentage of advanced cases — defined as cancers that had spread to the lymph nodes or beyond — hovered near 81% between 2000 and 2014, according to Kentucky Cancer Registry data. By 2020, that number had declined to 72%, according to the most recent data available.
“We are changing the story of families. And there is hope where there has not been hope before,” said Jennifer Knight, a LEADS principal investigator.
Older adults in their 60s and 70s can hold a particularly bleak view of their mortality odds, given what their loved ones experienced before screening became available, said Ashley Shemwell, a nurse navigator for the lung cancer screening program at Owensboro Health, a nonprofit health system that serves Kentucky and Indiana.
“A lot of them will say, ‘It doesn’t matter if I get lung cancer or not because it’s going to kill me. So I don’t want to know,’” said Shemwell. “With that generation, they saw a lot of lung cancers and a lot of deaths. And it was terrible deaths because they were stage 4 lung cancers.” But she reminds them that lung cancer is much more treatable if caught before it spreads.
The collaborative works with several partners, including the University of Kentucky, the University of Louisville, and GO2 for Lung Cancer, and has received grant funding from the Bristol Myers Squibb Foundation. Leaders have provided training and other support to 10 hospital-based screening programs, including a stipend to pay for resources such as educational materials or a nurse navigator, Knight said. In 2022, state lawmakers established a statewide lung cancer screening program based in part on the group’s work.
Jacob Sands, a lung cancer physician at Boston’s Dana-Farber Cancer Institute, credits the LEADS collaborative with encouraging patients to return for annual screening and follow-up testing for any suspicious nodules. “What the Kentucky LEADS program is doing is fantastic, and that is how you really move the needle in implementing lung screening on a larger scale,” said Sands, who isn’t affiliated with the Kentucky program and serves as a volunteer spokesperson for the American Lung Association.
In 2014, Kentucky expanded Medicaid, increasing the number of lower-income people who qualified for lung cancer screening and any related treatment. Adults 50 to 80 years old are advised to get a CT scan every year if they have accumulated at least 20 pack years and still smoke or have quit within the past 15 years, according to the latest task force recommendation, which widened the pool of eligible adults. (To calculate pack years, multiply the packs of cigarettes smoked daily by years of smoking.) The lung association offers an online quiz, called “Saved By The Scan,” to figure out likely eligibility for insurance coverage.
Half of U.S. patients aren’t diagnosed until their cancer has spread beyond the lungs and lymph nodes to elsewhere in the body. By then, the five-year survival rate is 8.2%.
But regular screening boosts those odds. When a CT scan detects lung cancer early, patients have an 81% chance of living at least 20 years, according to data published in November in the journal Radiology.
Some adults, like Lisa Ayers, didn’t realize lung cancer screening was an option. Her family doctor recommended a CT scan last year after she reported breathing difficulties. Ayers, who lives in Ohio near the Kentucky border, got screened at UK King’s Daughters, a hospital in far eastern Kentucky. The scan didn’t take much time, and she didn’t have to undress, the 57-year-old said. “It took me longer to park,” she quipped.
She was diagnosed with a lung carcinoid tumor, a type of neuroendocrine cancer that can grow in various parts of the body. Her cancer was considered too risky for surgery, Ayers said. A biopsy showed the cancer was slow-growing, and her doctors said they would monitor it closely.
Ayers, a lifelong smoker, recalled her doctor said that her type of cancer isn’t typically linked to smoking. But she quit anyway, feeling like she’d been given a second chance to avoid developing a smoking-related cancer. “It was a big wake-up call for me.”
Adults with a smoking history often report being treated poorly by medical professionals, said Jamie Studts, a health psychologist and a LEADS principal investigator, who has been involved with the research from the start. The goal is to avoid stigmatizing people and instead to build rapport, meeting them where they are that day, he said.
“If someone tells us that they’re not ready to quit smoking but they want to have lung cancer screening, awesome; we’d love to help,” Studts said. “You know what? You actually develop a relationship with an individual by accepting, ‘No.’”
Nationally, screening rates vary widely. Massachusetts reaches 11.9% of eligible residents, while California ranks last, screening just 0.7%, according to the lung association analysis.
That data likely doesn’t capture all California screenings, as it may not include CT scans done through large managed care organizations, said Raquel Arias, a Los Angeles-based associate director of state partnerships at the American Cancer Society. She cited other 2022 data for California, looking at lung cancer screening for eligible Medicare fee-for-service patients, which found a screening rate of 1%-2% in that population.
But, Arias said, the state’s effort is “nowhere near what it needs to be.”
The low smoking rate in California, along with its image as a healthy state, “seems to have come with the unintended consequence of further stigmatizing people who smoke,” said Arias, citing one of the findings from a 2022 report looking at lung cancer screening barriers. For instance, eligible patients may be reluctant to share prior smoking habits with their health provider, she said.
Meanwhile, Kentucky screening efforts progress, scan by scan.
At Appalachian Regional Healthcare, 3,071 patients were screened in 2023, compared with 372 in 2017. “We’re just scratching the surface of the potential lives that we can have an effect on,” said Stumbo, a lung cancer screening champion at the health system, which includes 14 hospitals, most located in eastern Kentucky.
The doctor hasn’t shed his own grief about what his family missed after his mother died at age 51, long before annual screening was recommended. “Knowing that my children were born, and never knowing their grandmother,” he said, “just how sad is that?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The voice in your head may help you recall and process words. But what if you don’t have one?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you imagine hearing yourself speak? A voice inside your head – perhaps reciting a shopping list or a phone number? What would life be like if you couldn’t?
Some people, including me, cannot have imagined visual experiences. We cannot close our eyes and conjure an experience of seeing a loved one’s face, or imagine our lounge room layout – to consider if a new piece of furniture might fit in it. This is called “aphantasia”, from a Greek phrase where the “a” means without, and “phantasia” refers to an image. Colloquially, people like myself are often referred to as having a “blind mind”.
While most attention has been given to the inability to have imagined visual sensations, aphantasics can lack other imagined experiences. We might be unable to experience imagined tastes or smells. Some people cannot imagine hearing themselves speak.
A recent study has advanced our understanding of people who cannot imagine hearing their own internal monologue. Importantly, the authors have identified some tasks that such people are more likely to find challenging.
fizkes/Shutterstock What the study found
Researchers at the University of Copenhagen in Denmark and at the University of Wisconsin-Madison in the United States recruited 93 volunteers. They included 46 adults who reported low levels of inner speech and 47 who reported high levels.
Both groups were given challenging tasks: judging if the names of objects they had seen would rhyme and recalling words. The group without an inner monologue performed worse. But differences disappeared when everyone could say words aloud.
Importantly, people who reported less inner speech were not worse at all tasks. They could recall similar numbers of words when the words had a different appearance to one another. This negates any suggestion that aphants (people with aphantasia) simply weren’t trying or were less capable.
Hearing our own imagined voice may play an important role in word processing. sutadimages/Shutterstock A welcome validation
The study provides some welcome evidence for the lived experiences of some aphants, who are still often told their experiences are not different, but rather that they cannot describe their imagined experiences. Some people feel anxiety when they realise other people can have imagined experiences that they cannot. These feelings may be deepened when others assert they are merely confused or inarticulate.
In my own aphantasia research I have often quizzed crowds of people on their capacity to have imagined experiences.
Questions about the capacity to have imagined visual or audio sensations tend to be excitedly endorsed by a vast majority, but questions about imagined experiences of taste or smell seem to cause more confusion. Some people are adamant they can do this, including a colleague who says he can imagine what combinations of ingredients will taste like when cooked together. But other responses suggest subtypes of aphantasia may prove to be more common than we realise.
The authors of the recent study suggest the inability to imagine hearing yourself speak should be referred to as “anendophasia”, meaning without inner speech. Other authors had suggested anauralia (meaning without auditory imagery). Still other researchers have referred to all types of imagined sensation as being different types of “imagery”.
Having consistent names is important. It can help scientists “talk” to one another to compare findings. If different authors use different names, important evidence can be missed.
We’re starting to broaden our understanding of the senses and how we imagine them. Napat Chaichanasiri/Shutterstock We have more than 5 senses
Debate continues about how many senses humans have, but some scientists reasonably argue for a number greater than 20.
In addition to the five senses of sight, smell, taste, touch and hearing, lesser known senses include thermoception (our sense of heat) and proprioception (awareness of the positions of our body parts). Thanks to proprioception, most of us can close our eyes and touch the tip of our index finger to our nose. Thanks to our vestibular sense, we typically have a good idea of which way is up and can maintain balance.
It may be tempting to give a new name to each inability to have a given type of imagined sensation. But this could lead to confusion. Another approach would be to adapt phrases that are already widely used. People who are unable to have imagined sensations commonly refer to ourselves as “aphants”. This could be adapted with a prefix, such as “audio aphant”. Time will tell which approach is adopted by most researchers.
Why we should keep investigating
Regardless of the names we use, the study of multiple types of inability to have an imagined sensation is important. These investigations could reveal the essential processes in human brains that bring about a conscious experience of an imagined sensation.
In time, this will not only lead to a better understanding of the diversity of humans, but may help uncover how human brains can create any conscious sensation. This question – how and where our conscious feelings are generated – remains one of the great mysteries of science.
Derek Arnold, Professor, School of Psychology, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Metabolic Health Roadmap – by Brenda Wollenberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The term “roadmap” is often used in informative books, but in this case, Wollenberg (a nutritionist with decades of experience) really does deliver what can very reasonably be described as a roadmap:
She provides chapters in the form of legs of a journey [to better metabolic health], and those legs are broadly divided into an “information center” to deliver new information, a “rest stop” for reflection, “roadwork” to guide the reader through implementing the information we just learned, in a practical fashion, and finally “traveller assistance” to give additional support / resources, as well as any potential troubleshooting, etc.
The information and guidance within are all based on very good science; a lot is what you will have read already about blood sugar management (generally the lynchpin of metabolic health in general), but there’s also a lot about leveraging epigenetics for our benefit, rather than being sabotaged by such.
There’s a little guidance that falls outside of nutrition (sleep, exercise, etc), but for the most part, Wollenberg stays within her own field of expertise, nutrition.
The style is idiosyncratic; it’s very clear that her goal is providing the promised roadmap, and not living up to any editor’s wish or publisher’s hope of living up to industry standard norms of book formatting. However, this pays off, because her delivery is clear and helpful while remaining personable and yet still bringing just as much actual science, and this makes for a very pleasant and informative read.
Bottom line: if you’d like to improve your metabolic health, as well as get held-by-the-hand through your health-improvement journey by a charming guide, this is very much the book for you!
Click here to check out the Metabolic Health Roadmap, and start taking steps!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: