The Dangers Of Fires, Floods, & Having Your Hair Washed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a dangerous business, going out of your door… And this week’s news round-up looks at 5 reasons why that might be:
Superspreading like wildfire
Environmental health risks are a big topic these days, with our changing climate. As for wildfires? Some of the risks are obvious: burning to death or choking to death in the smoke—but even upon surviving the seemingly worst, more threats remain that themselves can still kill.
Those threats include that both burns and smoke inhalation can cause acute and chronic changes in the immune system. Specifically: changes for the worse. The mechanisms by which this happens depend on the nature of any burns received, and in the case of smoke, what exactly was in the smoke. Now, there is no kind of smoke that is healthy to inhale, but definitely some kinds are a lot worse than others, and let’s just say, people’s homes contain a lot of plastic.
Additionally, if you think someone coughing near you spreads germs, imagine how far germs can be spread by miles-high, miles-wide billowing hot air.
In short, there’s a lot going on and none of it is good, and we’ve barely had room to summarise here, so…
Read in full: Wildfires ignite infection risks by weakening the body’s immune defenses and spreading bugs in smoke
Related: What’s Lurking In Your Household Air?
A flood of diseases
*record scratch*
Environmental health risks are a big topic these days, with our changing climate. As for floods? Some of the risks are obvious: drowning to death or having your house washed away—but even upon surviving the seemingly worst, more threats remain that themselves can still kill.
Those threats include increases in deaths from infectious and parasitic diseases, and respiratory diseases in general. Simply, a place that has been waterlogged, even if it seems “safe” now, is not a healthy place to be, due to bacteria, viruses, fungi, and more. In fact, it even increases all-cause mortality, because being healthy in such a place is simply harder:
Read in full: Linked to higher mortality rates, large floods emerge as an urgent public health concern
Related: Dodging Dengue In The US
Don’t lose your head
Visiting the hairdresser is not something that most people consider a potential brush with death—your hairdresser is probably not Sweeney Todd, after all. However…
There is an issue specifically with getting your hair washed there. Backwash basins—the sink things into which one rests one’s head at a backwards tilt—create an awkward angle for the cervical vertebrae and a sudden reduction in blood flow to the brain can cause a stroke, with the risk being sufficiently notable as to have its own name in scientific literature: beauty parlor stroke syndrome (BPSS).
❝While research suggests BPSS is most likely to occur in women over 50—and previous history of narrowing or thinning of blood vessels and arthritis of the spinal column in the neck are particular risk factors—it could happen to anyone regardless of age or medical history.❞
Read in full: The hidden health risk of having your hair washed
Related: Your Stroke Survival Plan
The smartwatch wristbands that give you cancer
It’s about the PFAS content. The article doesn’t discuss cancer in detail, just mentioning the increased risk, but you can read about the link between the two in our article below.
Basically, if your smartwatch wristband is a) not silicone and b) waterproof anyway, especially if it’s stain-resistant (as most are designed to be, what with wearing it next to one’s skin all the time while exercising, and not being the sort of thing one throws in the wash), then chances are it has PFAS levels much higher than normally found in consumer goods or clothing.
You can read more about how to identify the risks, here:
Read in full: Smartwatch bands can contain high levels of toxic PFAS, study finds
Related: PFAS Exposure & Cancer: The Numbers Are High
The cows giving milk with a little extra
Bird flu (HPAI) is now not the only flu epidemic amongst cattle in the US, and not only that, but rather than “merely” colonizing the lungs and upper respiratory tracts, in this case the virus (IAV) is thriving in the mammary glands, meaning that yes, it gets dispensed into the milk, and so far scientists are simply scrambling to find better ways to vaccinate the cattle, in the hopes that the milk will not be so risky because yes, it is currently a “reservoir and transmission vector” for the virus.
There are, however, barriers to creating those vaccines:
Read in full: Unexpected viral reservoir: influenza A thrives in cattle mammary glands
Related: Cows’ Milk, Bird Flu, & You
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bird Flu Is Bad for Poultry and Dairy Cows. It’s Not a Dire Threat for Most of Us — Yet.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Headlines are flying after the Department of Agriculture confirmed that the H5N1 bird flu virus has infected dairy cows around the country. Tests have detected the virus among cattle in nine states, mainly in Texas and New Mexico, and most recently in Colorado, said Nirav Shah, principal deputy director at the Centers for Disease Control and Prevention, at a May 1 event held by the Council on Foreign Relations.
A menagerie of other animals have been infected by H5N1, and at least one person in Texas. But what scientists fear most is if the virus were to spread efficiently from person to person. That hasn’t happened and might not. Shah said the CDC considers the H5N1 outbreak “a low risk to the general public at this time.”
Viruses evolve and outbreaks can shift quickly. “As with any major outbreak, this is moving at the speed of a bullet train,” Shah said. “What we’ll be talking about is a snapshot of that fast-moving train.” What he means is that what’s known about the H5N1 bird flu today will undoubtedly change.
With that in mind, KFF Health News explains what you need to know now.
Q: Who gets the bird flu?
Mainly birds. Over the past few years, however, the H5N1 bird flu virus has increasingly jumped from birds into mammals around the world. The growing list of more than 50 species includes seals, goats, skunks, cats, and wild bush dogs at a zoo in the United Kingdom. At least 24,000 sea lions died in outbreaks of H5N1 bird flu in South America last year.
What makes the current outbreak in cattle unusual is that it’s spreading rapidly from cow to cow, whereas the other cases — except for the sea lion infections — appear limited. Researchers know this because genetic sequences of the H5N1 viruses drawn from cattle this year were nearly identical to one another.
The cattle outbreak is also concerning because the country has been caught off guard. Researchers examining the virus’s genomes suggest it originally spilled over from birds into cows late last year in Texas, and has since spread among many more cows than have been tested. “Our analyses show this has been circulating in cows for four months or so, under our noses,” said Michael Worobey, an evolutionary biologist at the University of Arizona in Tucson.
Q: Is this the start of the next pandemic?
Not yet. But it’s a thought worth considering because a bird flu pandemic would be a nightmare. More than half of people infected by older strains of H5N1 bird flu viruses from 2003 to 2016 died. Even if death rates turn out to be less severe for the H5N1 strain currently circulating in cattle, repercussions could involve loads of sick people and hospitals too overwhelmed to handle other medical emergencies.
Although at least one person has been infected with H5N1 this year, the virus can’t lead to a pandemic in its current state. To achieve that horrible status, a pathogen needs to sicken many people on multiple continents. And to do that, the H5N1 virus would need to infect a ton of people. That won’t happen through occasional spillovers of the virus from farm animals into people. Rather, the virus must acquire mutations for it to spread from person to person, like the seasonal flu, as a respiratory infection transmitted largely through the air as people cough, sneeze, and breathe. As we learned in the depths of covid-19, airborne viruses are hard to stop.
That hasn’t happened yet. However, H5N1 viruses now have plenty of chances to evolve as they replicate within thousands of cows. Like all viruses, they mutate as they replicate, and mutations that improve the virus’s survival are passed to the next generation. And because cows are mammals, the viruses could be getting better at thriving within cells that are closer to ours than birds’.
The evolution of a pandemic-ready bird flu virus could be aided by a sort of superpower possessed by many viruses. Namely, they sometimes swap their genes with other strains in a process called reassortment. In a study published in 2009, Worobey and other researchers traced the origin of the H1N1 “swine flu” pandemic to events in which different viruses causing the swine flu, bird flu, and human flu mixed and matched their genes within pigs that they were simultaneously infecting. Pigs need not be involved this time around, Worobey warned.
Q: Will a pandemic start if a person drinks virus-contaminated milk?
Not yet. Cow’s milk, as well as powdered milk and infant formula, sold in stores is considered safe because the law requires all milk sold commercially to be pasteurized. That process of heating milk at high temperatures kills bacteria, viruses, and other teeny organisms. Tests have identified fragments of H5N1 viruses in milk from grocery stores but confirm that the virus bits are dead and, therefore, harmless.
Unpasteurized “raw” milk, however, has been shown to contain living H5N1 viruses, which is why the FDA and other health authorities strongly advise people not to drink it. Doing so could cause a person to become seriously ill or worse. But even then, a pandemic is unlikely to be sparked because the virus — in its current form — does not spread efficiently from person to person, as the seasonal flu does.
Q: What should be done?
A lot! Because of a lack of surveillance, the U.S. Department of Agriculture and other agencies have allowed the H5N1 bird flu to spread under the radar in cattle. To get a handle on the situation, the USDA recently ordered all lactating dairy cattle to be tested before farmers move them to other states, and the outcomes of the tests to be reported.
But just as restricting covid tests to international travelers in early 2020 allowed the coronavirus to spread undetected, testing only cows that move across state lines would miss plenty of cases.
Such limited testing won’t reveal how the virus is spreading among cattle — information desperately needed so farmers can stop it. A leading hypothesis is that viruses are being transferred from one cow to the next through the machines used to milk them.
To boost testing, Fred Gingrich, executive director of a nonprofit organization for farm veterinarians, the American Association of Bovine Practitioners, said the government should offer funds to cattle farmers who report cases so that they have an incentive to test. Barring that, he said, reporting just adds reputational damage atop financial loss.
“These outbreaks have a significant economic impact,” Gingrich said. “Farmers lose about 20% of their milk production in an outbreak because animals quit eating, produce less milk, and some of that milk is abnormal and then can’t be sold.”
The government has made the H5N1 tests free for farmers, Gingrich added, but they haven’t budgeted money for veterinarians who must sample the cows, transport samples, and file paperwork. “Tests are the least expensive part,” he said.
If testing on farms remains elusive, evolutionary virologists can still learn a lot by analyzing genomic sequences from H5N1 viruses sampled from cattle. The differences between sequences tell a story about where and when the current outbreak began, the path it travels, and whether the viruses are acquiring mutations that pose a threat to people. Yet this vital research has been hampered by the USDA’s slow and incomplete posting of genetic data, Worobey said.
The government should also help poultry farmers prevent H5N1 outbreaks since those kill many birds and pose a constant threat of spillover, said Maurice Pitesky, an avian disease specialist at the University of California-Davis.
Waterfowl like ducks and geese are the usual sources of outbreaks on poultry farms, and researchers can detect their proximity using remote sensing and other technologies. By zeroing in on zones of potential spillover, farmers can target their attention. That can mean routine surveillance to detect early signs of infections in poultry, using water cannons to shoo away migrating flocks, relocating farm animals, or temporarily ushering them into barns. “We should be spending on prevention,” Pitesky said.
Q: OK it’s not a pandemic, but what could happen to people who get this year’s H5N1 bird flu?
No one really knows. Only one person in Texas has been diagnosed with the disease this year, in April. This person worked closely with dairy cows, and had a mild case with an eye infection. The CDC found out about them because of its surveillance process. Clinics are supposed to alert state health departments when they diagnose farmworkers with the flu, using tests that detect influenza viruses, broadly. State health departments then confirm the test, and if it’s positive, they send a person’s sample to a CDC laboratory, where it is checked for the H5N1 virus, specifically. “Thus far we have received 23,” Shah said. “All but one of those was negative.”
State health department officials are also monitoring around 150 people, he said, who have spent time around cattle. They’re checking in with these farmworkers via phone calls, text messages, or in-person visits to see if they develop symptoms. And if that happens, they’ll be tested.
Another way to assess farmworkers would be to check their blood for antibodies against the H5N1 bird flu virus; a positive result would indicate they might have been unknowingly infected. But Shah said health officials are not yet doing this work.
“The fact that we’re four months in and haven’t done this isn’t a good sign,” Worobey said. “I’m not super worried about a pandemic at the moment, but we should start acting like we don’t want it to happen.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
For Seniors With Hoarding Disorder, a Support Group Helps Confront Stigma and Isolation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A dozen people seated around folding tables clap heartily for a beaming woman: She’s donated two 13-gallon garbage bags full of clothes, including several Christmas sweaters and a couple of pantsuits, to a Presbyterian church.
A closet cleanout might not seem a significant accomplishment. But as the people in this Sunday-night class can attest, getting rid of stuff is agonizing for those with hoarding disorder.
People with the diagnosis accumulate an excessive volume of things such as household goods, craft supplies, even pets. In extreme cases, their homes become so crammed that moving between rooms is possible only via narrow pathways.
These unsafe conditions can also lead to strained relationships.
“I’ve had a few relatives and friends that have condemned me, and it doesn’t help,” said Bernadette, a Pennsylvania woman in her early 70s who has struggled with hoarding since retiring and no longer allows guests in her home.
People who hoard are often stigmatized as lazy or dirty. NPR, Spotlight PA, and KFF Health News agreed to use only the first names of people with hoarding disorder interviewed for this article because they fear personal and professional repercussions if their condition is made public.
As baby boomers age into the group most affected by hoarding disorder, the psychiatric condition is a growing public health concern. Effective treatments are scarce. And because hoarding can require expensive interventions that drain municipal resources, more funding and expertise is needed to support those with the diagnosis before the issue grows into a crisis.
For Bernadette, the 16-week course is helping her turn over a new leaf.
The program doubles as a support group and is provided through Fight the Blight. The Westmoreland County, Pennsylvania, organization started offering the course at a local Masonic temple after founder Matt Williams realized the area lacked hoarding-specific mental health services.
Fight the Blight uses a curriculum based on cognitive behavioral therapy to help participants build awareness of what fuels their hoarding. People learn to be more thoughtful about what they purchase and save, and they create strategies so that decluttering doesn’t become overwhelming.
Perhaps more importantly, attendees say they’ve formed a community knitted together through the shared experience of a psychiatric illness that comes with high rates of social isolation and depression.
“You get friendship,” said Sanford, a classmate of Bernadette’s.
After a lifetime of judgment, these friendships have become an integral part of the changes that might help participants eventually clear out the clutter.
Clutter Catches Up to Baby Boomers
Studies have estimated that hoarding disorder affects around 2.5% of the general population — a higher rate than schizophrenia.
The mental illness was previously considered a subtype of obsessive-compulsive disorder, but in 2013 it was given its own diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, the DSM-5.
The biological and environmental factors that may drive hoarding are not well understood. Symptoms usually appear during the teenage years and tend to be more severe among older adults with the disorder. That’s partly because they have had more time to acquire things, said Kiara Timpano, a University of Miami psychology professor.
“All of a sudden you have to downsize this huge home with all the stuff and so it puts pressures on individuals,” she said. In Bernadette’s case, her clutter includes a collection of VHS tapes, and spices in her kitchen that she said date back to the Clinton administration.
But it’s more than just having decades to stockpile possessions; the urge to accumulate strengthens with age, according to Catherine Ayers, a psychiatry professor at the University of California-San Diego.
Researchers are working to discern why. Ayers and Timpano theorize that age-related cognitive changes — particularly in the frontal lobe, which regulates impulsivity and problem-solving — might exacerbate the disorder.
“It is the only mental health disorder, besides dementia, that increases in prevalence and severity with age,” Ayers said.
As the U.S. population ages, hoarding presents a growing public health concern: Some 1 in 5 U.S. residents are baby boomers, all of whom will be 65 or older by 2030.
This population shift will require the federal government to address hoarding disorder, among other age-related issues that it has not previously prioritized, according to a July report by the Democratic staff of the U.S. Senate Special Committee on Aging, chaired then by former Sen. Bob Casey (D-Pa.).
Health Hazards of Hoarding
Clutter creates physical risks. A cramped and disorderly home is especially dangerous for older adults because the risk of falling and breaking a bone increases with age. And having too many things in one space can be a fire hazard.
Last year, the National Fallen Firefighters Foundation wrote to the Senate committee’s leadership that “hoarding conditions are among the most dangerous conditions the fire service can encounter.” The group also said that cluttered homes delay emergency care and increase the likelihood of a first responder being injured on a call.
The Bucks County Board of Commissioners in Pennsylvania told Casey that hoarding-related mold and insects can spread to adjacent households, endangering the health of neighbors.
Due to these safety concerns, it might be tempting for a family member or public health agency to quickly empty someone’s home in one fell swoop.
That can backfire, Timpano said, as it fails to address people’s underlying issues and can be traumatic.
“It can really disrupt the trust and make it even less likely that the individual is willing to seek help in the future,” she said.
It’s more effective, Timpano said, to help people build internal motivation to change and help them identify goals to manage their hoarding.
For example, at the Fight the Blight class, a woman named Diane told the group she wanted a cleaner home so she could invite people over and not feel embarrassed.
Sanford said he is learning to keep his documents and record collection more organized.
Bernadette wants to declutter her bedroom so she can start sleeping in it again. Also, she’s glad she cleared enough space on the first floor for her cat to play.
“Because now he’s got all this room,” she said, “he goes after his tail like a crazy person.”
Ultimately, the home of someone with hoarding disorder might always be a bit cluttered, and that’s OK. The goal of treatment is to make the space healthy and safe, Timpano said, not to earn Marie Kondo’s approval.
Lack of Treatment Leaves Few Options
A 2020 study found that hoarding correlates with homelessness, and those with the disorder are more likely to be evicted.
Housing advocates argue that under the Fair Housing Act, tenants with the diagnosis are entitled to reasonable accommodation. This might include allowing someone time to declutter a home and seek therapy before forcing them to leave their home.
But as outlined in the Senate aging committee’s report, a lack of resources limits efforts to carry out these accommodations.
Hoarding is difficult to treat. In a 2018 study led by Ayers, the UCSD psychiatrist, researchers found that people coping with hoarding need to be highly motivated and often require substantial support to remain engaged with their therapy.
The challenge of sticking with a treatment plan is exacerbated by a shortage of clinicians with necessary expertise, said Janet Spinelli, the co-chair of Rhode Island’s hoarding task force.
Could Changes to Federal Policy Help?
Casey, the former Pennsylvania senator, advocated for more education and technical assistance for hoarding disorder.
In September, he called for the Substance Abuse and Mental Health Services Administration to develop training, assistance, and guidance for communities and clinicians. He also said the Centers for Medicare & Medicaid Services should explore ways to cover evidence-based treatments and services for hoarding.
This might include increased Medicare funding for mobile crisis services to go to people’s homes, which is one way to connect someone to therapy, Spinelli said.
Another strategy would involve allowing Medicaid and Medicare to reimburse community health workers who assist patients with light cleaning and organizing; research has found that many who hoard struggle with categorization tasks.
Williams, of Fight the Blight, agrees that in addition to more mental health support, taxpayer-funded services are needed to help people address their clutter.
When someone in the group reaches a point of wanting to declutter their home, Fight the Blight helps them start the process of cleaning, removing, and organizing.
The service is free to those earning less than 150% of the federal poverty level. People making above that threshold can pay for assistance on a sliding scale; the cost varies also depending on the size of a property and severity of the hoarding.
Also, Spinelli thinks Medicaid and Medicare should fund more peer-support specialists for hoarding disorder. These mental health workers draw on their own life experiences to help people with similar diagnoses. For example, peer counselors could lead classes like Fight the Blight’s.
Bernadette and Sanford say courses like the one they enrolled in should be available all over the U.S.
To those just starting to address their own hoarding, Sanford advises patience and persistence.
“Even if it’s a little job here, a little job there,” he said, “that all adds up.”
This article is from a partnership that includes Spotlight PA, NPR, and KFF Health News.
Spotlight PA is an independent, nonpartisan, and nonprofit newsroom producing investigative and public-service journalism that holds power to account and drives positive change in Pennsylvania. Sign up for its free newsletters.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
What Does Kaempferol Do, Anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝In the this or that article, you said kampeferol was a famously good flavonol on a par with quercetin, does it do the same thing or does it do something different, and is it worth supplementing?❞
So, this will be in reference to a This-or-That from last week:
Cantaloupe vs Cucumber – Which is Healthier?
Let’s break down your question into parts:
- Is it comparable to quercetin?
- Does it have special properties of its own?
- Is it worth supplementing?
Is it comparable to quercetin?
They are both flavonols, and potent ones at that. Similarities include that they’re found in many of the same plants, and that (like most if not all polyphenols) they have antioxidant and anti-inflammatory benefits, which in turn usually translate to anti-aging and anticancer benefits too.
You can read more about quercetin here: Fight Inflammation & Protect Your Brain, With Quercetin
You can read more about polyphenols in general here: 21 Most Beneficial Polyphenols & What Foods Have Them ← quercetin and kaempferol are #1 and #2 on this list, respectively
Does it have special properties of its own?
Yes it does!
❝Epidemiological studies have shown an inverse relationship between kaempferol intake and cancer.
Kaempferol may help by augmenting the body’s antioxidant defense against free radicals, which promote the development of cancer.
At the molecular level, kaempferol has been reported to modulate a number of key elements in cellular signal transduction pathways linked to apoptosis, angiogenesis, inflammation, and metastasis.
Significantly, kaempferol inhibits cancer cell growth and angiognesis and induces cancer cell apoptosis, but on the other hand, kaempferol appears to preserve normal cell viability, in some cases exerting a protective effect.❞
Read in full: A review of the dietary flavonoid, kaempferol on human health and cancer chemoprevention
It is also particularly good for the gut:
❝Most recently, an increasing number of studies have demonstrated the significance of kaempferol in the regulation of intestinal function and the mitigation of intestinal inflammation❞
Read in full: A Critical Review of Kaempferol in Intestinal Health and Diseases
This also means it is particularly efficacious against food allergies:
❝we screened food ingredients with the expectation of finding dietary compounds that exert beneficial effects on intestinal immune tolerance and identified kaempferol, a flavonoid, as the compound that most effectively increased Aldh1a2 mRNA levels❞
(that’s good)
That one’s a bit scientifically denser than we usually try to find when citing sources here, so here’s a pop-science article about the same thing, which explains in more words than we have room to here:
Flavonoid kaempferol could offer natural relief for food allergies ← much lighter reading, but still very informative
Kaempferol (like quercetin, granted) is also a potent neuroprotective agent, not least of all because its anti-inflammatory powers extend to reducing neuroinflammation (not everything does, because not everything we ingest can pass the blood-brain barrier to affect what goes on in the brain):
…and more:
❝it may be used to treat numerous acute and chronic inflammation-induced diseases, including intervertebral disc degeneration and colitis, as well as post-menopausal bone loss and acute lung injury. In addition, it has beneficial effects against cancer, liver injury, obesity and diabetes, inhibits vascular endothelial inflammation, protects the cranial nerve and heart function, and may be used for treating fibroproliferative disorders, including hypertrophic scar.❞
Read in full: Recent progress regarding kaempferol for the treatment of various diseases
Is it worth supplementing?
If you eat a lot of leafy greens, cruciferous vegetables, and/or citrus fruits, and/or drink tea (true teas from tea plants, not miscellaneous herbal infusions), then you probably get a good dose of kaempferol already.
However, if you want to supplement, hawthorn berry is not a bad one to go with, like this example product on Amazon 😎
We wrote about this before, here: Hawthorn For The Heart (& More)
As for teas, if you’re wondering about the merits of black, white, green or red, check out:
Black, White, Green, Red: Which Kind Of Tea Is Best For The Health, According To Science? ← this covers many factors
Enjoy!
Share This Post
Related Posts
-
Nori vs Wakame – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing nori to wakame, we picked the nori.
Why?
It was close, and both of these seaweed options are great!
In terms of macros, nori has more protein while wakame has more carbs; they’re about equal on fiber. While the difference in protein and carbs isn’t big, out of the two we’ll prioritize protein, and thus say nori gets a notional win here—but as it’s so close, one could just as easily call it a tie.
In the category of vitamins both are very rich in many minerals, but nori has more of vitamins A, B1, B2, B6, B12*, and C, while wakame has more of vitamins B5, B9, K, and choline. Thus, a 6:4 victory for nori.
*Yes, nori is one of those rare vegan foods that naturally contain vitamin B12; it’s because of the composition of the algae that this seaweed is made of, which includes some beneficial B12-making bacteria. Meanwhile, wakame is “just” a kelp, so it doesn’t have B12.
When it comes to minerals, nori has more potassium and zinc, while wakame has more calcium and magnesium. They’re equal on other minerals, except: it’s worth noting that wakame is moderately high in sodium, while nori has very little sodium. So, either a tie-breaking win for nori, or just a tie.
Adding up the sections gives nori the overall win; it’s only the margin of the win that’s reasonably debatable. Still, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
- A Deeper Dive Into Seaweed
- Spirulina vs Nori – Which is Healthier? ← guess which won!
- 21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nori and wakame both feature (very favorably) in this case study
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Breathe; Don’t Vent (At Least In The Moment)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Zen And The Art Of Breaking Things
We’ve talked before about identifying emotions and the importance of being able to express them:
Answering The Most Difficult Question: How Are You?
However, there can be a difference between “expressing how we feel” and “being possessed by how we feel and bulldozing everything in our path”
…which is, of course, primarily a problem in the case of anger—and by extension, emotions that are often contemporaneous with anger, such as jealousy, shame, fear, etc.
How much feeling is too much?
While this is in large part a subjective matter, clinically speaking the key question is generally: is it adversely affecting daily life to the point of being a problem?
For example, if you have to spend half an hour every day actively managing a certain emotion, that’s probably indicative of something unusual, but “unusual” is not inherently bad. If you’re managing it safely and in a way that doesn’t negatively affect the rest of your life, then that is generally considered fine, unless you feel otherwise about it.
A good example of this is complicated grief and/or prolonged grief.
But what about when it comes to anger? How much is ok?
When it comes to those around you, any amount of anger can seem like too much. Anger often makes us short-tempered even with people who are not the object of our anger, and it rarely brings out the best in us.
We can express our feelings in non-aggressive ways, for example:
and
Seriously Useful Communication Skills!
Sometimes, there’s another way though…
Breathe; don’t vent
That’s a great headline, but we can’t take the credit for it, because it came from:
Breathe, don’t vent: turning down the heat is key to managing anger
…in which it was found that, by all available metrics, the popular wisdom of “getting it off your chest” doesn’t necessarily stand up to scrutiny, at least in the short term:
❝The work was inspired in part by the rising popularity of rage rooms that promote smashing things (such as glass, plates and electronics) to work through angry feelings.
I wanted to debunk the whole theory of expressing anger as a way of coping with it,” she said. “We wanted to show that reducing arousal, and actually the physiological aspect of it, is really important.❞
And indeed, he and his team did find that various arousal-increasing activities (such as hitting a punchbag, breaking things, doing vigorous exercise) did not help as much as arousal-decreasing activities, such as mindfulness-based relaxation techniques.
If you’d like to read the full paper, then so would we, but we couldn’t get full access to this one yet. However, the abstract includes representative statistics, so that’s worth a once-over:
Caveat!
Did you notice the small gap between their results and their conclusion?
In a lab or similar short-term observational setting, their recommendation is clearly correct.
However, if the source of your anger is something chronic and persistent, it could well be that calming down without addressing the actual cause is just “kicking the can down the road”, and will still have to actually be dealt with eventually.
So, while “here be science”, it’s not a mandate for necessarily suffering in silence. It’s more about being mindful about how we go about tackling our anger.
As for a primer on mindfulness, feel free to check out:
No-Frills, Evidence-Based Mindfulness
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
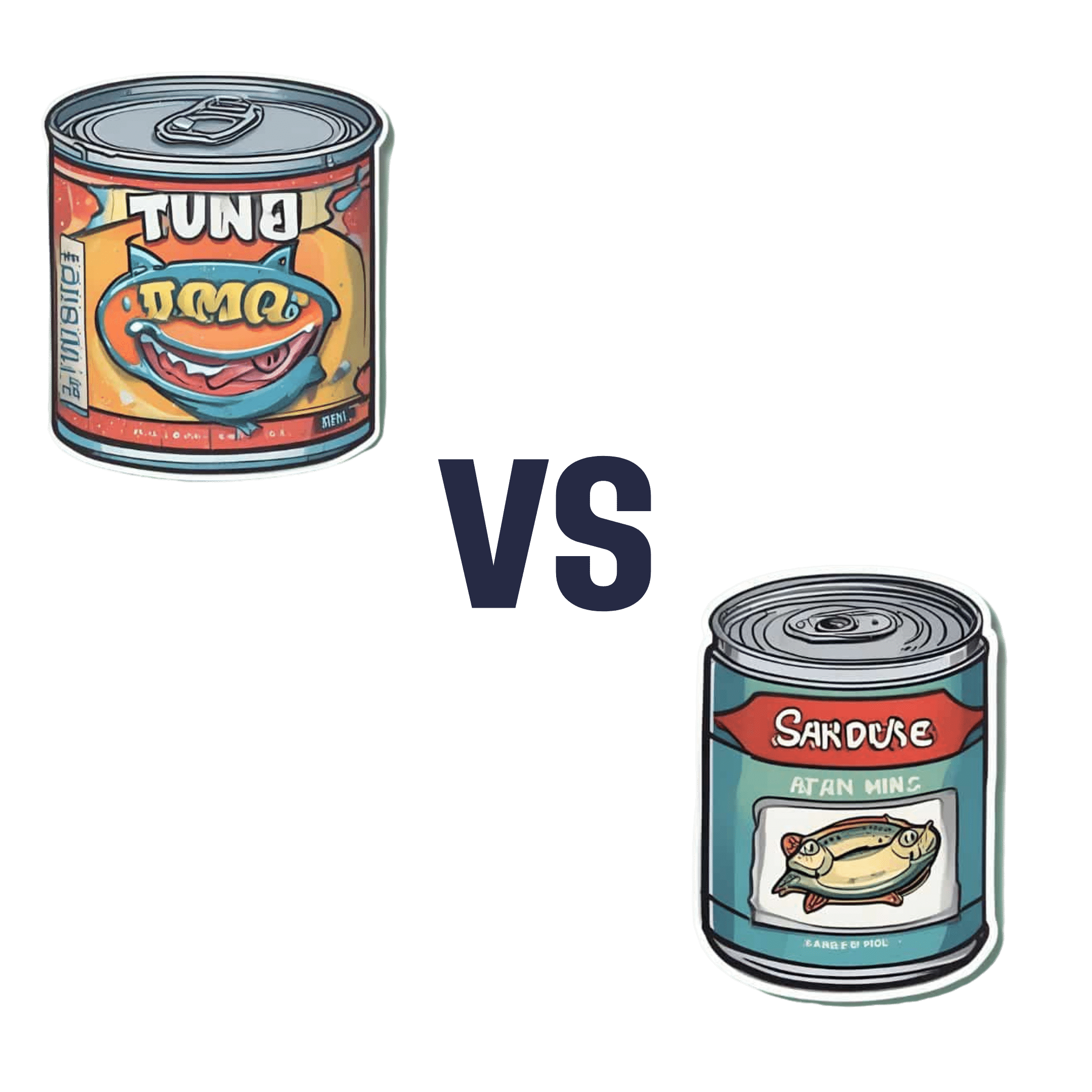
Canned Tuna vs Canned Sardines – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing canned tuna to canned sardines, we picked the sardines.
Why?
This comparison is unfair, but practical—because both are sold next to each other in the supermarket and often used for similar things.
It’s unfair because in a can of tuna, there is tuna meat, whereas in a can of sardines, there is sardine meat, skin, and bones.
Consequently, sardines outperform tuna in almost everything, because a lot of nutrients are in the skin and bones.
To be completely unambiguous:
Sardines have more vitamins and minerals by far (special shout-out to calcium, of which sardines contain 6000% more), and more choline (which is sometimes reckoned as a vitamin, sometimes not).
Tuna does have marginally more protein, and less fat. If you are trying to limit your cholesterol intake, then that could be an argument for choosing tuna over sardines.
All in all: the sardines are more nutrient dense by far, are good sources of vitamins and minerals that tuna contains less of (and in many cases only trace amounts of), and for most people this will more than offset the difference in cholesterol, especially if having not more than one can per day.
About that skin and bones…
That’s where the real benefit for your joints lies, by the way!
See: We Are Such Stuff As Fish Are Made Of
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: