Rise And (Really) Shine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q&A with 10almonds Subscribers!
Q: Would love to hear more ideas about effective first thing in the morning time management to get a great start on your day.
A: There are a lot of schools of thought about what’s best in this regard! Maybe we’ll do a main feature sometime. But some things that are almost universally agreed upon are:
- Prepare your to-do list the night before
- Have some sort of buffer between waking up and getting to productivity.
- For me (hi, your writer here) it’s my first coffee of the day. It’s not even about the caffeine, it’s about the ritual of it, it’s a marker that separates my night from the day and tells my brain what gear to get into.
- Others may like to exercise first thing in the morning
- For still yet others, it could be a shower, cold or otherwise
- Some people like a tall glass of lemon water to rehydrate after sleeping!
- If you take drinkable morning supplements such as this pretty awesome nootropic stack, it’s a great time for that and an excellent way to get the brain-juices flowing!
- When you do get to productivity: eat the frog first! What this means is: if eating a frog is the hardest thing you’ll have to do all day, do that first. Basically, tackle the most intimidating task first. That way, you won’t spend your day stressed/anxious and/or subconsciously wasting time in order to procrastinate and avoid it.
- Counterpart to the above: a great idea is to also plan something to look forward to when your working day is done. It doesn’t matter much what it is, provided it’s rewarding to you, that makes you keen to finish your tasks to get to it.
Have a question you’d like to see answered here? Hit reply to this email, or use the feedback widget at the bottom! We always love to hear from you
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Creatine: Very Different For Young & Old People
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the Deal with Creatine?
Creatine is best-known for its use as a sports supplement. It has a few other uses too, usually in the case of helping to treat (or recover from) specific medical conditions.
What actually is it?
Creatine is an organic compound formed from amino acids (mostly l-arginine and lysine, can be l-methionine, but that’s not too important for our purposes here).
We can take it as a supplement, we can get it in our diet (unless we’re vegan, because plants don’t make it; vertebrates do), and we can synthesize it in our own bodies.
What does it do?
While creatine supplements mostly take the form of creatine monohydrate, in the body it’s mostly stored in our muscle tissue as phosphocreatine, and it helps cells produce adenosine triphosphate, (ATP).
ATP is how energy is kept ready to use by cells, and is cells’ immediate go-to when they need to do something. For this reason, it’s highly instrumental in cell repair and rebuilding—which is why it’s used so much by athletes, especially bodybuilders or other athletes that have a vested interest in gaining muscle mass and enjoying faster recovery times.
See: Creatine use among young athletes
However! For reasons as yet not fully known, it doesn’t seem to have the same beneficial effect after a certain age:
What about the uses outside of sport?
Almost all studies outside of athletic performance have been on animals, despite it being suggested as potentially helpful for many things, including:
- Alzheimer’s disease
- Parkinson’s disease
- Huntington’s disease
- ischemic stroke
- epilepsy
- brain or spinal cord injuries
- motor neuron disease
- memory and brain function in older adults
However, research that’s been done on humans has been scant, if promising:
- A review of creatine supplementation in age-related diseases: more than a supplement for athletes
- Creatine supplementation and cognitive performance in elderly individuals
In short: creatine may reduce symptoms and slow the progression of some neurological diseases, although more research in humans is needed, and words such as “promising”, “potential”, etc are doing a lot of the heavy lifting in those papers we just cited.
Is it safe?
It seems so: Creatine supplementation and health variables: a retrospective study
Nor does it appear to create the sometimes-rumored kidney problems, cramps, or dehydration:
Where can I get it?
You can get it from pretty much any sports nutrition outlet, or you can order online. For example:
Share This Post
-
Why You’re Tired & How To Fix It
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Sadia Badiei. A dietician by academic and professional background, she’s nowadays hung up her lab coat for a chef’s jacket, and is best known for her “Pick Up Limes” brand. Today, we’ll be taking her advice on managing energy levels with what’s on our plates!
Quick note: our usual medical/legal disclaimer applies, and this article cannot diagnose you from afar, and thus neither can it make any certain prescription; this is for educational purposes, and aimed at being applicable to most of our readers.
There are many possible things that can cause chronic fatigue, and not all of them can be fixed by diet. Your doctor will have access to tests and such that we, being a humble health science publication, do not.
You may recognize her; we’ve featured her videos occasionally, mostly recently:
Pick Up A Zest For Life: 10 Lessons For A Healthy Mind & Body
But, what does she want us to know about living life with more energy?
It starts with balance
Badiei makes the case that we should strive for a nutritionally-balanced diet; that may not come as much of a revelation, but what does that look like for a vegan (Badiei advocates for plant-based eating)?
She recommends that our diet consist of:
- About 50% fruits and vegetables
- About 25% grains and starches
- About 25% proteins
- Modest amounts of fats
- A little of well-chosen dairy substitutions
- Finally, a few judicious supplements to top it off
That does add up to more than 100%, but 1) we did say “About n%” and 2) this is not a bad thing to note, actually, since Badiei advocates (as we do) for focussing more on what we add into our diet, rather than what we take out.
Breaking it down a little further, she recommends making sure to get “the foundational seven”, which is a little like “Dr. Greger’s Daily Dozen”, but in this case it’s counted on a per-food-type basis.
Thus, she recommends:
- Dark green leafy vegetables
- Assorted other non-starchy vegetables (your choice what kind)
- Fruit, of any kinds (unlike Dr. Greger separating berries)
- Grains and starches (so for example, potatoes are lumped in with rice here, botanically very different, but often fulfil a similar culinary role)
- Nuts and seeds
- Legumes
- Fortified dairy alternatives
For full details including how much of each, and “what counts”, etc, see:
Pick Up Limes | The Nourish Method
Time your carbs
Slow-release carbohydrates, those with the most fiber, are best most of the time, giving us more sustained fuel, keeping us energized for longer after meals—even if we would rather sleep:
She cites: Fiber and Saturated Fat Are Associated with Sleep Arousals and Slow Wave Sleep
Quick-release carbohydrates, those with what’s generally considered a less favorable carb:fiber ratio, are best if we’re going to eat nearer to bedtime. We know, eating before bed is often considered a bit of a no-no, but Badiei bids us indulge if we so desire, as the quicker-absorbed carbohydrates support tryptophan reaching our brain more efficiently, and thus promote sleep onset.
See also: Should You Go Light Or Heavy On Carbs?
About that fat
We mentioned (or rather, Badiei’s citation mentioned) saturated fat. It is indeed linked with difficulty falling asleep, and/but omega-3 fatty acids, on the other hand, promote better sleep.
She cites: The relationship between sleep duration, sleep quality and dietary intake in adults
While you’re enjoying those nuts and seeds (for the omega-3 fatty acids), you might also note that several also star in Badiei’s list of plant-based foods that are rich in tryptophan, such as soy, cashews, pumpkin seeds, sunflower seeds, beans, green vegetables, and mushrooms.
Micronutrients
Badiei’s focus here is on B-vitamins, iron, magnesium, selenium, and zinc. We imagine most of our readers here are taking steps to ensure to get a full daily coverage of vitamins and minerals anyway, but you might want to read what she has to say about iron on a plant-based diet, because the numbers may be different than you think.
The reason for this is that while animal products contain mostly heme iron, which is easier to absorb but associated with a risk increase in some diseases, plant-based foods usually* contain only non-heme iron, which is healthier but not as bioavailable, so if eating only plants, we need more of it:
Pick Up Limes | Iron on a Plant-Based Diet
*If you eat a carnivorous plant, guess what, it’ll have heme iron in it, tangling that food web.
“What if I know I have chronic fatigue for non-dietary reasons?”
Well, that sucks, and we’re not going to pretend the above will magically fix it. However, there are still things that can at least relatively improve your experience:
Eat To Beat Chronic Fatigue! Yes, Even When Fatigued Chronically
(it’s a good guide to being able to consistently eat healthily when your energy levels are consistently at minimal, meaning that a lot of common advice becomes unusable)
Take care!
Share This Post
-
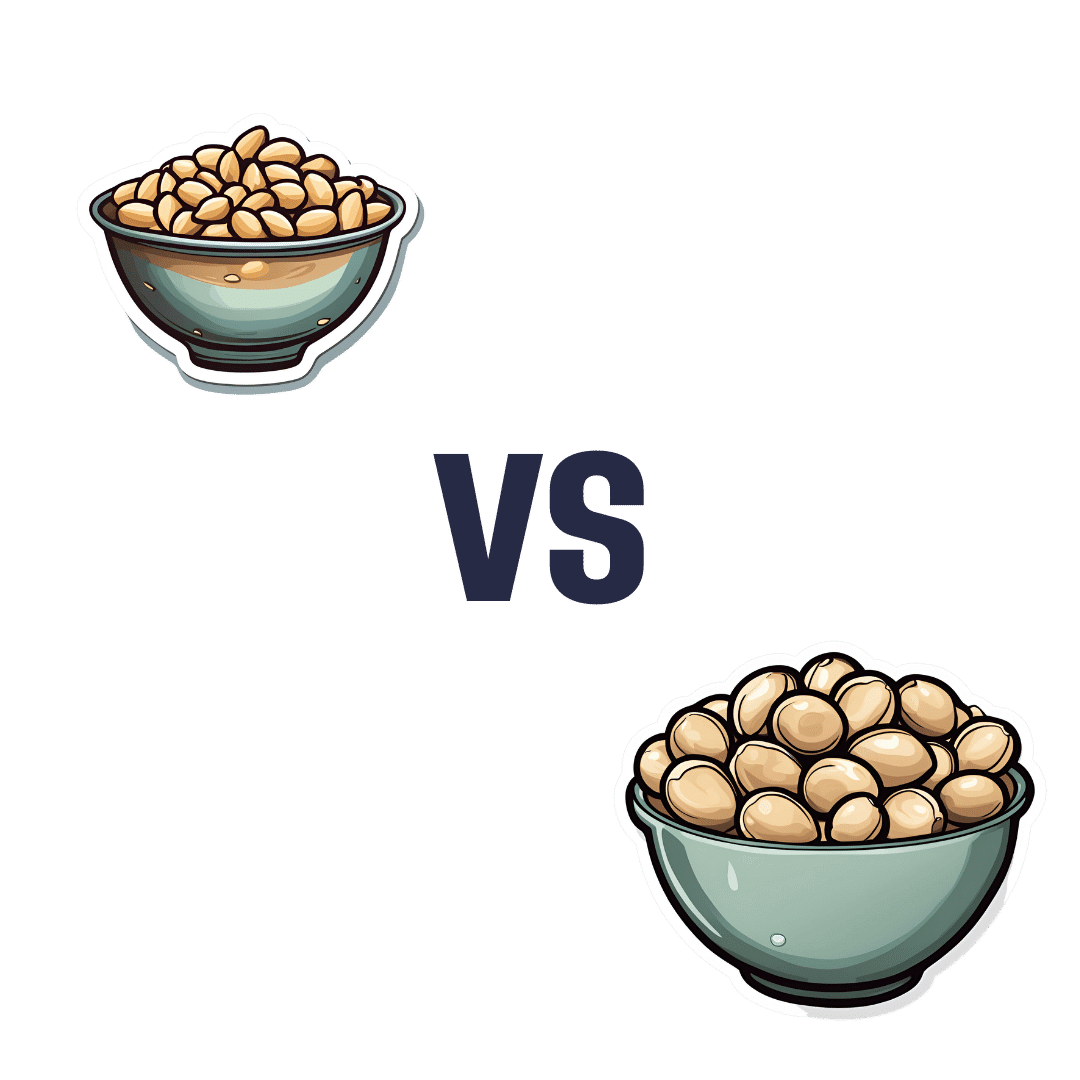
Pine Nuts vs Macadamia Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pine nuts to macadamias, we picked the pine nuts.
Why?
In terms of macros, it’s subjective depending on what you want to prioritize; the two nuts are equal in carbs, but pine nuts have more protein and macadamias have more fiber. We’d generally prioritize the fiber, which so far would give macadamias a win in this category, but if you prefer the protein, then consider it pine nuts. Next, we must consider fats; macadamias have slightly more fat, and of which, proportionally more saturated fat, resulting in 3x the total saturated fat compared to pine nuts, gram for gram. With this in mind, we consider this category a tie or a marginal nominal win for pine nuts.
In the category of vitamins, pine nuts have more of vitamins A, B2, B3, B9, E, K, and choline, while macadamias have more of vitamins B1, B5, B6, and C. A clear win for pine nuts this time, especially with pine nuts having more than 17x the vitamin E of macadamias.
When it comes to minerals, pine nuts have more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while macadamias have more calcium and selenium. Another easy win for pine nuts.
In short, enjoy either or both (diversity is good), but pine nuts are the healthier by most metrics.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Enjoy!
Share This Post
Related Posts
-
Vegan Eager for Milk Alternatives
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Q: Thanks for the info about dairy. As a vegan, I look forward to a future comment about milk alternatives
Thanks for bringing it up! What we research and write about is heavily driven by subscriber feedback, so notes like this really help us know there’s an audience for a given topic!
We’ll do a main feature on it, to do it justice. Watch out for Research Review Monday!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Therapeutic Journey – by Alain de Botton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve often featured The School of Life’s videos here on 10almonds, and most of those are written by (and often voiced by) Alain de Botton.
This book lays out the case for mental health being also just health, that no person is perfectly healthy all the time, and sometimes we all need a little help. While he does suggest seeking help from reliable outside sources, he also tells a lot about how we can improve things for ourselves along the way, whether by what we can control in our environment, or just what’s between our ears.
In the category of limitations, the book is written with the assumption that you are in a position to have access to a therapist of your choice, and in a sufficiently safe and stable life situation that there is a limit to how bad things can get.
The style is… Alain de Botton’s usual style. Well-written, clear, decisive, instructive, compassionate, insightful, thought-provoking.
Bottom line: this isn’t a book for absolutely everyone, but if your problems are moderate and your resources are comfortable, then this book has a lot of insights that can make your life more easy-going and joyful, without dropping the seriousness when appropriate.
Click here to check out A Therapeutic Journey, and perhaps begin one of your own!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
6 Worst Foods That Cause Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How many do you consume?
The hit list
Dr. Li bids us avoid:
High carb, low fiber foods: consuming a diet high in carbohydrates, particularly refined carbs like cakes, white bread, pizza, and sugary syrups, can significantly harm brain health. Over time, imbalanced (i.e. not balanced with fiber) carbohydrate consumption leads to the growth of visceral fat (not the same as subcutaneous fat, which is the squishy bits just under your skin; visceral fat is further underneath, around your viscera), , which triggers systemic inflammation and oxidative stress. These processes disrupt communication between brain cells, impair memory, and increase the risk of diseases like Alzheimer’s and Parkinson’s. High carb diets can also contribute to metabolic syndrome—a cluster of conditions, including diabetes, obesity and high blood pressure—that damage blood vessels, leading to strokes and vascular dementia.
Trans fats: these are region-bound, as they’re banned in some places and not others—check your local regulations. Found in processed foods such as fried items, baked goods, packaged snacks, and margarine, trans fats are created through hydrogenation, which makes fats more stable at room temperature. These artificial fats raise bad cholesterol, lower good cholesterol, and promote atherosclerosis. This damages the brain by reducing oxygen supply, triggering chronic inflammation, and increasing the risk of Alzheimer’s and dementia.
Sodas: regular consumption of sodas, whether sugary or artificially sweetened, is harmful to brain health. A single can of soda contains around 9 teaspoons of sugar, which overwhelms metabolism, contributes to insulin resistance, and leads to inflammation. These effects damage blood vessels and brain tissue, disrupt neuron function, and increase the risk of type 2 diabetes and dementia. Furthermore, insulin resistance caused by excessive sugar intake can impair neuronal survival, activate immune responses, and exacerbate cognitive decline. As for the artificial sweeteners, the mechanism of harm depends on the sweetener (and some can also mess up insulin response, for reasons that are not entirely clear yet, but they measurably do), but even picking the healthiest artificial sweetener, training your palate to enjoy hyper-sweetened things will tend to lead to more sugar-laden food choices in other parts of one’s diet.
Processed foods: arguably a broad category that encompasses some of the above, but it’s important to consider it separately for catch-all purposes: these convenience foods, laden with artificial preservatives, colors, and sweeteners, harm brain health through chronic inflammation and usually a lack of essential nutrients. Processed foods are also a significant source of microplastics, which have been found to accumulate in the arteries, contributing to plaque build-up, atherosclerosis, and reduced blood flow to the brain. This combination of inflammation and oxidative stress from microplastics damages brain cells, paving the way for cognitive decline and dementia.
Seafood with high mercury levels: large fish such as tuna, swordfish, sharks, and tilefish accumulate high amounts of mercury, a potent neurotoxin. Fish that are larger, older, and/or higher up the food chain will have the most mercury (and other cumulative contaminants, for that matter, but we’re considering mercury here). Mercury disrupts essential brain chemicals like dopamine and serotonin, triggering oxidative stress and damaging brain cells. Chronic exposure to mercury leads to inflammation and neuroinflammation, both of which increase the risk of Alzheimer’s and dementia.
Alcohol: contrary to popular belief, any amount of alcohol is detrimental to brain health. While red wine is often promoted for its health benefits, the purported positive effects come from polyphenols, not the alcohol itself, and (for example) resveratrol from red wine cannot be delivered in meaningful doses without drinking an impossibly large quantity. Alcohol is a neurotoxin that can damage or kill brain cells, impair neuronal communication, and lead to cognitive decline. Excessive drinking results in hangover symptoms like headaches and brain fog, which are indicators of its harmful impact on the brain. Chronic alcohol consumption exacerbates neuron death, increases inflammation, and raises the risk of dementia.
As for what to eat instead?
Dr. Li recommends including foods such as:
- foods rich in omega-3s that aren’t mercury-laden fish, e.g. flaxseeds, chia seeds, walnuts, and hemp seeds, as they reduce inflammation, protect blood vessel linings, and prevent vascular dementia.
- berries, and in particular he recommends organic strawberries, which are rich in ellagic acid and anthocyanins, which improve memory, reduce depressive symptoms, and enhance cognitive function.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: