Recognize The Early Symptoms Of Parkinson’s Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Parkinson’s disease is a degenerative condition with wide-reaching implications for health. While there is currently no known cure, there are treatments, so knowing about it sooner rather than later is important.
Spot The Signs
There are two main kinds of symptoms, motor and non-motor.
Motor symptoms include:
- trembling that occurs when muscles are relaxed; often especially visible in the fingers
- handwriting changes—not just because of the above, but also often getting smaller
- blank expression, on account of fewer instruction signals getting through to the face
- frozen gait—especially difficulty starting walking, and a reduced arm swing
Non-motor symptoms include:
- loss of sense of smell—complete, or a persistent reduction of
- sleepwalking, or sleep-talking, or generally acting out dreams while asleep
- constipation—on an ongoing basis
- depression/anxiety, especially if there was no prior history of these conditions
For more detail on each of these, as well as what steps you might want to take, check out what Dr. Luis Zayas has to say:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Citicoline vs Parkinson’s (And More)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 5 Foods Seniors Should Eat To Sleep Better Tonight (And 5 To Avoid)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, a sleep specialist, advises:
A prescription for rest
Dr. Breus’s top 5 foods to eat for a good night’s sleep are:
1) Chia seeds: high in fiber, protein, omega-3s, calcium, magnesium, phosphorus, and tryptophan, they help raise melatonin levels for better sleep. The high fiber content also reduces late-night snacking, and in any case, it’s recommended to eat them 2–3 hours before bed. As for how, they can be added to smoothies, baked goods, salads, or made into chia seed pudding.
2) Nuts (especially pistachios & almonds): both of these nuts are rich in B vitamins and melatonin, so take your pick! He does recommend, however, no more than ¼ cup about 1.5 hours before bed. Either can be eaten as-is or with an unsweetened Greek yogurt.
3) Bananas (especially banana tea): contain magnesium, especially in the peel. Boil an organic banana (with peel) in water and drink the water, which provides magnesium and helps improve sleep. It’s recommended to drink it about an hour before bed.
10almonds tip: he doesn’t mention this, but if you prefer, you can also simply eat it—banana peel is perfectly edible, and is not tough when cooked. If you’ve ever had plantains, you’ll know how they are, and bananas (and their peel) are much softer than plantains. Boiling is fine, or alternatively you can wrap them in foil and bake them. The traditional way is to cook them in the leaves, but chances are you live somewhere that doesn’t grow bananas locally and so they didn’t come with leaves, so foil is fine.
4) Tart cherries: are rich in melatonin, antioxidants, and other anti-inflammatory compounds, which all help with falling asleep faster and reducing night awakenings. Can be consumed as juice, dried fruit, or tart cherry extract capsules. Suggested intake: once in the morning and once an hour before bed.
5) Kiwis: are high in serotonin, which aids melatonin production and sleep. This also helps regulate cortisol levels (lower cortisol promotes sleep). He recommends eating kiwi fruit about 2 hours before bed.
Also, in the category of foods (or rather: food types) to avoid before bed…
- High quantities of red meat: can disrupt sleep-related amino acid balance.
- Acidic foods: can cause acid reflux.
- High sugar foods: can slow melatonin production when consumed in the evening.
- Caffeine-rich foods & drinks: includes chocolate and coffee; avoid in the evening.
- Large meals before bed: digestion is less efficient when lying down, causing sleep disruption.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Calculate (And Enjoy) The Perfect Night’s Sleep ← Our “Expert Insights” main feature on Dr. Breus
Take care!
Share This Post
-
How to Be Your Own Therapist – by Owen O’Kane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Finding the right therapist can be hard. Sometimes, even just accessing a therapist, any therapist, can be hard, if circumstances are adverse. Sometimes we’d like therapy, but want to feel “better prepared for it” before we do.
Owen O’Kane, a highly qualified and well-respected psychotherapist, wants to put some tools in our hands. The premise of this book is that “in 10 minutes a day” one can give oneself an amount of therapy that will be beneficial.
Naturally, in 10 minutes a day, this isn’t going to be the kind of therapy that will work through major traumas, so what can it do?
Those 10 minutes are spread into three sessions:
- 4 minutes in the morning
- 3 minutes in the afternoon
- 3 minutes in the evening
The idea is:
- To do a quick mental health “check-in” before the day gets started, ascertain what one needs in that context, and make a simple plan to get/have it.
- To keep one’s mental health on track by taking a little pause to reassess and adjust if necessary
- To reflect on the day, amplify the positive, and let go of the negative to what extent is practical, in order to rest well ready for the next day
Where O’Kane excels is in explaining how to do those things in a way that is neither overly simplistic and wishy-washy, nor so arcane and convoluted as to create more work and render the day more difficult.
In short, this book is a great prelude to (or adjunct to) formal therapy, and for those for whom therapy isn’t accessible and/or desired, a great way to keep oneself on a mentally healthy track.
Share This Post
-
7 Essential Devices For Hand Arthritis: Regain Control of Your Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Diana Girnita is a double board-certified physician in rheumatology and internal medicine. With a PhD in immunology (on top of her MD), and training at Harvard and top universities, she founded Rheumatologist OnCall, offering integrative medicine to broaden rheumatology access. Here’s what she has to say about things that make life easier:
Get your hands on these…
The seven devices that Dr. Girnita recommends are:
- Hand grip strengthener: helps build grip strength with a spring-loaded mechanism. Regular use can improve strength and reduce pain.
- Finger exerciser: different device; similar principle: it strengthens hand and finger muscles using resistance, enhancing hand function.
- Moisturizing paraffin bath: a heated paraffin wax bath that soothes hands, providing heat therapy and moisturizing the skin.
- Weighted silverware: weighted utensils (knives, forks, spoons) make gripping easier and provide stability for eating.
- Foam tubing grips: foam covers to make kitchen tools, toothbrushes, and hairbrushes easier to grip.
- Electric can-opener: reduces strain in opening cans, making meal preparation more accessible.
- Compression gloves: provide gentle compression to reduce swelling and pain, improving hand flexibility and circulation.
- Door knob cover grips: make it easier to turn doorknobs by providing a larger surface to grip.
- Wider-grip pens: ergonomically designed pens with a larger diameter and softer grip reduce hand strain while writing.
This writer, who does not have arthritis but also does not have anything like the grip strength she used to, also recommends a jar opener like this one.
As a bonus, if you spend a lot of time writing at a computer, an ergonomic split keyboard like this one goes a long way to avoiding carpal tunnel syndrome, and logically must be better for arthritis than a regular keyboard; another excellent thing to have (that again this writer uses and swears by) is an ergonomic vertical mouse like this one (aligns the wrist bones correctly; the “normal” horizontal version is woeful for the carpal bones). These things are both also excellent to help avoid worsening peripheral neuropathy (something that troubles this writer’s wrists if she’s not careful, due to old injuries there).
For more on the seven things otherwise listed above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Avoiding/Managing Rheumatoid Arthritis
- Avoiding/Managing Osteoarthritis
- Managing Chronic Pain (Realistically!)
Take care!
Share This Post
Related Posts
-
Waist Size Worries: Age-Appropriate Solutions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝My BMI is fine, but my waist is too big. What do I do about that? I am 5′ 5″ tall and 128 pounds and 72 years old.❞
It’s hard to say without knowing about your lifestyle (and hormones, for that matter)! But, extra weight around the middle in particular is often correlated with high levels of cortisol, so you might find this of benefit:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Protein vs Sarcopenia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein vs Sarcopenia
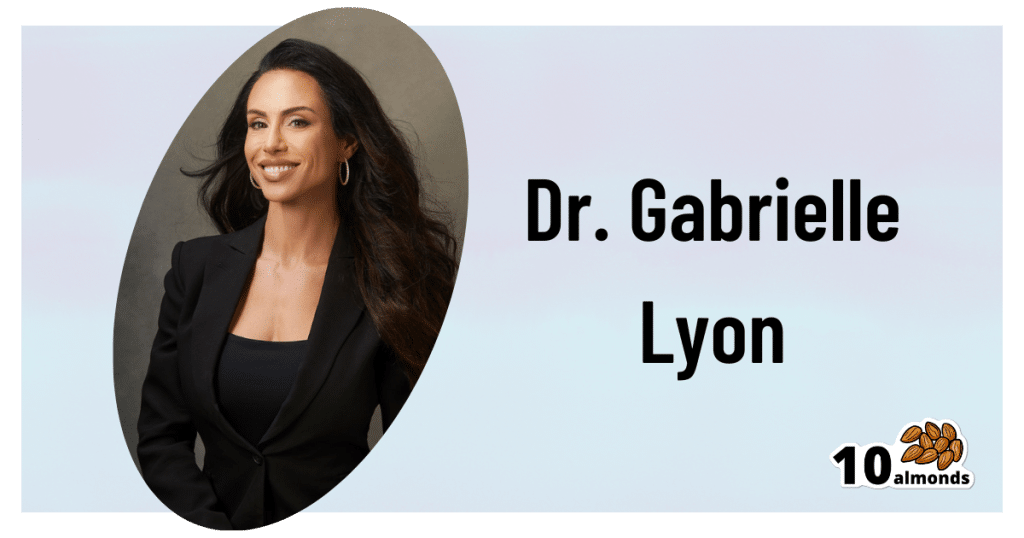
This is Dr. Gabrielle Lyon. A medical doctor, she’s board-certified in family medicine, and has also engaged in research and clinical practice in the fields of geriatrics and nutritional sciences.
A quick note…
We’re going to be talking a bit about protein metabolism today, and it’s worth noting that Dr. Lyon personally is vehemently against vegetarianism/veganism, and considers red meat to be healthy.
Scientific consensus on the other hand, holds that vegetarianism and veganism are fine for most people if pursued in an informed and mindful fashion, that white meat and fish are also fine for most people, and red meat is simply not.
If you’d like a recap on the science of any of that:
- Protein: How Much Do We Need, Really?
- Plant vs Animal Protein: Diversity is Key
- Do We Need Animal Products to be Healthy?
Nevertheless, if we look at the science that she provides, the advice is sound when applied to protein in general and without an undue focus on red meat.
How much protein is enough?
In our article linked above, we gave 1–2g/kg/day
Dr. Lyons gives the more specific 1.6g/kg/day for adults older than 40 (this is where sarcopenia often begins!) and laments that many sources offer 0.8g/kg.
To be clear, that “per kilogram” means per kilogram of your bodyweight. For Americans, this means dividing lbs by 2.2 to get the kg figure.
Why so much protein?
Protein is needed to rebuild not just our muscles, but also our bones, joint tissues, and various other parts of us:
We Are Such Stuff As Fish Are Made Of
Additionally, our muscles themselves are important for far more than just moving us (and other things) around.
As Dr. Lyon explains: sarcopenia, the (usually age-related) loss of muscle mass, does more than just make us frail; it also messes up our metabolism, which in turn messes up… Everything else, really. Because everything depends on that.
This is because our muscles themselves use a lot of our energy, and/but also store energy as glycogen, so having less of them means:
- getting a slower metabolism
- the energy that can’t be stored in muscle tissue gets stored somewhere else (like the liver, and/or visceral fat)
So, while for example the correlation between maintaining strong muscles and avoiding non-alcoholic fatty liver disease may not be immediately obvious, it is clear when one follows the metabolic trail to its inevitable conclusion.
Same goes for avoiding diabetes, heart disease, and suchlike, though those things are a little more intuitive.
How can we get so much protein?
It can seem daunting at first to get so much protein if you’re not used to it, especially as protein is an appetite suppressant, so you’ll feel full sooner.
It can especially seem daunting to get so much protein if you’re trying to avoid too many carbs, and here’s where Dr. Lyon’s anti-vegetarianism does have a point: it’s harder to get lean protein without meat/fish.
That said, “harder” does not mean “impossible” and even she acknowledges that lentils are great for this.
If you’re not vegetarian or vegan, collagen supplementation is a good way to make up any shortfall, by the way.
And for everyone, there are protein supplements available if we want them (usually based on whey protein or soy protein)
Anything else we need to do?
Yes! Eating protein means nothing if you don’t do any resistance work to build and maintain muscle. This can take various forms, and Dr. Lyon recommends lifting weights and/or doing bodyweight resistance training (calisthenics, Pilates, etc).
Here are some previous articles of ours, consistent with the above:
- Resistance Is Useful! (Especially As We Get Older)
- Overdone It? How To Speed Up Recovery After Exercise
- How To Do HIIT (Without Wrecking Your Body)
- Exercises To Do (And Ones To Avoid) If You Have Osteoporosis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’m So Effing Tired – by Dr. Amy Shah
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy sometimes to feel like we know more or less what we should be doing… If only we had the energy to get going!
- We know we want a better diet… But we don’t have the time/energy to cook so will go for the quickest option even when it’s not the best?
- We know we should exercise… But feel we just need to crash out on the couch for a bit first?
- We would dearly love to get better sleep… But our responsibilities aren’t facilitating that?
…and so on. Happily, Dr. Amy Shah is here with ways to cut through the Gordian Knot that is this otherwise self-perpetuating cycle of exhaustion.
Most of the book is based around tackling what Dr. Shah calls “the energy trifecta“:
- Hormone levels
- Immune system
- Gut health
You’ll note (perhaps with relief) that none of these things require an initial investment of energy that you don’t have… She’s not asking you to hit the gym at 5am, or magically bludgeon your sleep schedule into its proper place, say.
Instead, what she gives is practical, actionable, easy changes that don’t require much effort, to gently slide us back into the fast lane of actually having energy to do stuff!
In short: if you’ve ever felt like you’d like to implement a lot of very common “best practice” lifestyle advice, but just haven’t had the energy to get going, there’s more value in this handbook than in a thousand motivational pep talks.
Click here to check out “I’m So Effing Tired” and get on a better track of life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: