Do we need animal products to be healthy?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do we need animal products to be healthy?
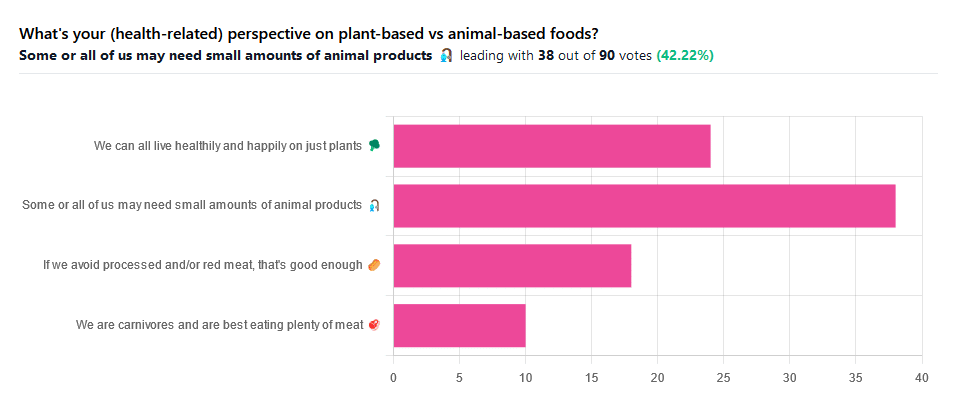
We asked you for your (health-related) perspective on plant-based vs anima-based foods, and got the above-pictured spread of answers.
“Some or all of us may need small amounts of animal products” came out on top with more votes than the two more meat-eatery options combined, and the second most popular option was the hard-line “We can all live healthily and happily on just plants”.
Based on these answers, it seems our readership has quite a lot of vegans, vegetarians, and perhaps “flexitarians” who just have a little of animal products here and there.
Perhaps we should have seen this coming; the newsletter is “10almonds”, not “10 rashers of bacon”, after all.
But what does the science say?
We are carnivores and are best eating plenty of meat: True or False?
False. Let’s just rip the band-aid off for this one.
In terms of our anatomy and physiology, we are neither carnivores nor herbivores:
- We have a mid-length digestive tract (unlike carnivores and herbivores who have short and long ones, respectively)
- We have a mouthful of an assortment of teeth; molars and premolars for getting through plants from hard nuts to tough fibrous tubers, and we have incisors for cutting into flesh and (vestigial, but they’re there) canines that really serve us no purpose now but would have been a vicious bite when they were bigger, like some other modern-day primates.
- If we look at our closest living relatives, the other great apes, they are mostly frugivores (fruit-eaters) who supplement their fruity diet with a small quantity of insects and sometimes other small animals—of which they’ll often eat only the fatty organ meat and discard the rest.
And then, there’s the health risks associated with meat. We’ll not linger on this as we’ve talked about it before, but for example:
- Processed Meat Consumption and the Risk of Cancer: A Critical Evaluation of the Constraints of Current Evidence from Epidemiological Studies
- Red Meat Consumption (Heme Iron Intake) and Risk for Diabetes and Comorbidities?
- Health Risks Associated with Meat Consumption: A Review of Epidemiological Studies
- Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake With Incident Cardiovascular Disease and All-Cause Mortality
- Meat consumption: Which are the current global risks? A review of recent (2010-2020) evidences
If we avoid processed and/or red meat, that’s good enough: True or False?
True… Ish.
Really this one depends on one’s criteria for “good enough”. The above-linked studies, and plenty more like them, give the following broad picture:
- Red and/or processed meats are unequivocally terrible for the health in general
- Other mammalian meats, such as from pigs, are really not much better
- Poultry, on the other hand, the science is less clear on; the results are mixed, and thus so are the conclusions. The results are often barely statistically significant. In other words, when it comes to poultry, in the matter of health, the general consensus is that you can take it or leave it and will be fine. Some studies have found firmly for or against it, but the consensus is a collective scientific shrug.
- Fish, meanwhile, has almost universally been found to be healthful in moderation. You may have other reasons for wanting to avoid it (ethics, environmentalism, personal taste) but those things are beyond the scope of this article.
Some or all of us may need small amounts of animal products: True or False?
True! With nuances.
Let’s divide this into “some” and “all”. Firstly, some people may have health conditions and/or other mitigating circumstances that make an entirely plant-based diet untenable.
We’re going light on quotations from subscriber comments today because otherwise this article will get a bit long, but here’s a great example that’s worth quoting, from a subscriber who voted for this option:
❝I have a rare genetic disease called hereditary fructose intolerance. It means I lack the enzyme, Aldolase B, to process fructose. Eating fruits and veggies thus gives me severe hypoglycemia. I also have anemia caused by two autoimmune diseases, so I have to eat meat for the iron it supplies. I also supplement with iron pills but the pills alone can’t fix the problem entirely.❞
And, there’s the thing. Popular vegan talking-points are very good at saying “if you have this problem, this will address it; if you have that problem, that will address it”, etc. For every health-related objection to a fully plant-based diet there’s a refutation… Individually.
But actual real-world health doesn’t work like that; co-morbidities are very common, and in some cases, like our subscriber above, one problem undermines the solution to another. Add a third problem and by now you really just have to do what you need to do to survive.
For this reason, even the Vegan Society’s definition of veganism includes the clause “so far as is possible and practicable”.
Now, as for the rest of us “all”.
What if we’re really healthy and are living in optimal circumstances (easy access to a wide variety of choice of food), can we live healthily and happily just on plants?
No—on a technicality.
Vegans famously need to supplement vitamin B12, which is not found in plants. Ironically, much of the B12 in animal products comes from the animals themselves being given supplements, but that’s another matter. However, B12 can also be enjoyed from yeast. Popular options include the use of yeast extract (e.g. Marmite) and/or nutritional yeast in cooking.
Yeast is a single-celled microorganism that’s taxonomically classified as a fungus, even though in many ways it behaves like an animal (which series of words may conjure an amusing image, but we mean, biologically speaking).
However, it’s also not technically a plant, hence the “No—on a technicality”
Bottom line:
By nature, humans are quite versatile generalists when it comes to diet:
- Most of us can live healthily and happily on just plants if we so choose.
- Some people cannot, and will require varying kinds (and quantities) of animal products.
- As for red and/or processed meats, we’re not the boss of you, but from a health perspective, the science is clear: unless you have a circumstance that really necessitates it, just don’t.
- Same goes for pork, which isn’t red and may not be processed, but metabolically it’s associated with the same problems.
- The jury is out on poultry, but it strongly appears to be optional, healthwise, without making much of a difference either way
- Fish is roundly considered healthful in moderation. Enjoy it if you want, don’t if you don’t.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Buckwheat vs Rye – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing buckwheat to rye, we picked the buckwheat.
Why?
Both are good, wholegrain options for most people! On which note, yes, we are comparing whole groats* vs whole grains here, respectively.
*buckwheat is, you may remember, a flowering plant and not technically a grain or even a grass (and is very unrelated to wheat; it’s as closely related to wheat as a lionfish is to a lion).
In terms of macros, buckwheat has more protein, while rye has more carbs and fiber, the ratios of which mean that rye has the higher glycemic index. All in all, we’re calling this category a win for buckwheat on the basis of those things, but really, both are fine.
When it comes to vitamins, buckwheat has more of vitamins B1, B3, B6, B7, B9, K, and choline, while rye has more of vitamins B2, B5, and E. An easy win for buckwheat here.
In the category of minerals, buckwheat has more copper, calcium, iron, magnesium, phosphorus, potassium, and zinc, while rye has more manganese and selenium. Another clear win for buckwheat.
Lastly. it’s worth noting that while buckwheat does not contain gluten, rye does. So, if you’re avoiding gluten, buckwheat is the option to choose here for that reason too.
If you don’t have celiac disease, wheat allergy, gluten intolerance, or something like that, then rye is still very worthwhile; buckwheat may have won on numbers in each category, but rye wasn’t far behind on anything; the margins of difference were quite small today.
Still, buckwheat is the best all-rounder here!
Want to learn more?
You might like to read:
- Grains: Bread Of Life, Or Cereal Killer?
- Gluten: What’s The Truth?
- Eat More (Of This) For Lower Blood Pressure
Take care!
Share This Post
-
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With one in four Australian adults experiencing problems with incontinence, some people look to supplements for relief.
With ingredients such as pumpkin seed oil and soybean extract, a range of products promise relief from frequent bathroom trips.
But do they really work? Let’s sift through the claims and see what the science says about their efficacy.
Christian Moro/Shutterstock What is incontinence?
Incontinence is the involuntary loss of bladder or bowel control, leading to the unintentional leakage of urine or faeces. It can range from occasional minor leaks to a complete inability to control urination and defecation.
This condition can significantly impact daily activities and quality of life, and affects women more often than it affects men.
Some people don’t experience bladder leakage but can sometimes feel an urgent need to go to the bathroom. This is known as overactive bladder syndrome, and occurs when the muscles around the bladder tighten on their own, which greatly reduces its capacity. The result is the person feels the need to go to the bathroom much more frequently.
There are many potential causes of incontinence and overactive bladders, including menopause, pregnancy and child birth, urinary tract infections, pelvic floor disorders, and an enlarged prostate. Conditions such as diabetes, neurological disorders and certain medications (such as diuretics, sleeping pills, antidepressants and blood-pressure drugs) can also contribute.
While pelvic muscle rehabilitation and behavioural techniques for bladder retraining can be helpful, some people are interested in pharmaceutical solutions.
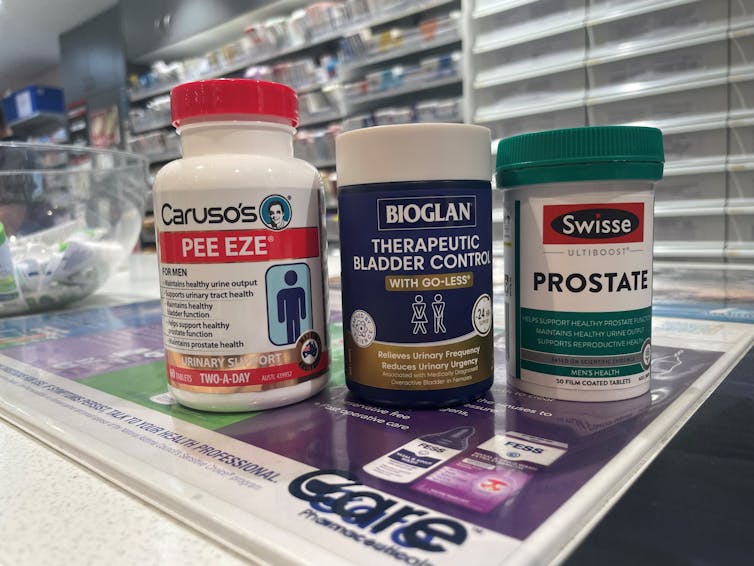
What’s in these products?
A number of supplements are available in Australia that include ingredients used in traditional medicine for urinary incontinence and overactive bladders. The three most common ingredients are:
- Cucurbita pepo (pumpkin seed extract)
- glycine max (soybean extract)
- an extract from the bark of the Crateva magna or nurvala (Varuna) tree.
The supplements have common ingredients. Author How are they supposed to work?
Pumpkin seeds are rich in plant sterols that are thought to reduce the testosterone-related enlargement of the prostate, as well as having broader anti-inflammatory effects. The seed extracts can also contain oleic acid, which may help increase bladder capacity by relaxing the muscles around the organ.
Soybean extracts are rich in isoflavones, especially daidzen and genistein. Like olieic acid, these are thought to act on the muscles around the bladder. Because isoflavones are similar in structure to the female hormone oestrogen, soy extracts may be most beneficial for postmenopausal women who have overactive bladders.
Crateva extract is rich in lupeol- and sterol-based chemicals which have strong anti-inflammatory effects. This has benefits not just for enlarged prostates but possibly also for reducing urinary tract infections.
Do they actually work?
It’s important to note that the government has only approved these types of supplements as “listed medicines”. This means the ingredients have only been assessed for safety. The companies behind the products have not had to provide evidence they actually work.
A 2014 clinical trial examined a combined pumpkin seed and soybean extract called cucurflavone on people with overactive bladders. The 120 participants received either a placebo or a daily 1,000mg dose of the herbal mixture over a period of 12 weeks.
By the end of study, those in the cucurflavone group went to the bathroom around three fewer times per day, compared with people in the control group, who only went to the bathroom on average one fewer time each day.
In a different trial, researchers examined a combination of Crateva bark extract with herbal extracts of horsetail and Japanese evergreen spicebush, called Urox.
For the 150 participants, the Urox formulation helped participants go to the bathroom less frequently when compared with placebo treatment.
After eight weeks of treatment, participants in the placebo group were going to the bathroom to urinate 11 times per day. Those in the Urox group were only going around to 7.5 times per day. And those who took Urox also needed to go to the bathroom one fewer time during the night.
Finally, another study also examined a Creteva, horsetail and Japanese spicebush combination, but this time in children. They were given either a 420mg dose of the supplement or a placebo, and then monitored for how many times they wet the bed.
After two months of taking the supplement, slightly more than 40% of the 24 kids in the supplement group wet the bed less often.
While these results may look promising, there are considerable limitations to the studies which means the data may not be reliable. For example, the trials didn’t include enough participants to have reliable data. To conclusively provide efficacy, final-stage clinical trials require data for between 300 and 3,000 patients.
From the studies, it is also not clear whether some participants were also taking other medicines as well as the supplement. This is important, as medications can interfere with how the supplements work, potentially making them less or more effective.
What if you want to take them?
If you have incontinence or an overactive bladder, you should always discuss this with your doctor, as it may due to a serious or treatable underlying condition.
Otherwise, your GP may give you strategies or exercises to improve your bladder control, prescribe medications or devices, or refer you to a specialist.
If you do decide to take a supplement, discuss this with your doctor and local pharmacist so they can check that any product you choose will not interfere with any other medications you may be taking.
Nial Wheate, Professor of Pharmaceutical Chemistry, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Best Workouts for Women Over 40 To Give Your Metabolism A Makeover
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
After 40, the usual course of events goes: your lean muscle mass decreases, which slows your metabolism and makes it easier to gain fat. At the same time, bone density decreases, increasing the risk of osteoporosis and frailty. This leads to lower mobility, flexibility, and overall frustration.
But it doesn’t have to be that way! Fitness coach Jessica Cooke explains how:
It all depends on this
Strength training helps counteract these effects by increasing lean muscle mass, which boosts metabolism and fat burning. It also improves bone density, reducing the risk of osteoporosis. Plus, it builds strength, fitness, and a toned physique.
The best part? It doesn’t require long workouts—short, effective sessions work best.
While walking is very beneficial for general health, it doesn’t provide the resistance needed to build muscle. Without resistance, your body composition won’t change, and so your metabolism will remain the same. Strength training is essential for burning fat at rest and improving overall fitness.
You don’t have to do high-impact exercises or jumping to see results. Low-impact strength training is effective and gentle on the joints. Lifting weights or using your body weight in a controlled manner will help build muscle and improve strength.
Many women only do cardio and neglect strength training, leading to minimal progress. Another common mistake is overcomplicating workouts—simple, consistent strength training is all you need.
Aim to strength train three times per week for 20 minutes. Focus on compound movements that work multiple muscle groups, such as:
- squats
- lunges
- deadlifts
- press-ups
- shoulder presses
- upright rows
- planks
- glute bridges
- sit-ups
- Russian twists
Start with light (e.g. 2-3 kg) weights and maintain proper form.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Don’t Let Menopause Run You Down: 4 Critical Things Female Runners Should Know
Take care!
Share This Post
Related Posts
-
Capsaicin For Weight Loss And Against Inflammation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Capsaicin’s Hot Benefits
Capsaicin, the compound in hot peppers that makes them spicy, is a chemical irritant and a neurotoxin. However, humans being humans, we decided to eat them for fun.
In contrast to many other ways in which humans recreationally enjoy things that are objectively poisonous, consuming capsaicin (in moderation) is considered to have health benefits, such as aiding weight loss (by boosting metabolism) and reducing inflammation.
Let’s see what the science says…
First: is it safe?
Capsaicin is classified as “Generally Recognized As Safe”. That said, the same mechanism that causes them to boost metabolism, does increase blood pressure:
Mechanisms underlying the hypertensive response induced by capsaicin
If you are in good cardiovascular health, this increase should be slight and not pose any threat, unless for example you enter a chili-eating contest when not acclimated to such:
Capsaicin and arterial hypertensive crisis
As ever, if unsure, do check with your doctor first, especially if you are taking any blood pressure medications, or otherwise have known blood pressure issues.
Does it really boost metabolism?
It certainly does; it works by increasing oxygen consumption and raising body temperature, both of which mean more calories will be burned for the same amount of work:
Dietary capsaicin and its anti-obesity potency: from mechanism to clinical implications
This means, of course, that chili peppers enjoy the status of being functionally a “negative calorie” food, and a top-tier one at that:
Chili pepper as a body weight-loss food
Here’s a good quality study that showed a statistically significant* fat loss improvement over placebo:
*To put it in numbers, the benefit was:
- 5.91 percentage points lower body fat percentage than placebo
- 6.68 percentage points greater change in body fat mass than placebo
See also: Difference between percentages and percentage points
For those who prefer big reviews than single studies, we’ve got you covered:
Does it really reduce inflammation?
Counterintuitive as it may seem, yes. By means of reducing oxidative stress. Given that things that reduce oxidative stress tend to reduce inflammation, and in turn tend to reduce assorted disease risks (from diabetes to cancer to Alzheimer’s), this probably has more knock-on benefits too, but we don’t have room to explore all of those today.
Fresh peppers are best for this, but dried peppers (such as when purchased as a ground spice in the supermarket, or when purchased as a capsule-based supplement) still have a very respectable anti-inflammatory effect:
- Capsaicinoids, Polyphenols and Antioxidant Activities of Capsicum annuum: Comparative Study of the Effect of Ripening Stage and Cooking Methods
- A Review on the Effect of Drying on Antioxidant Potential of Fruits and Vegetables
How much should we take?
It’s recommended to start at a low dose and gradually increase it, but 2–6mg of capsaicin per day is the standard range used in studies.
If you’re getting this from peppers, then for example cayenne pepper (a good source of capsaicin) contains around 2.5mg of capsaicin per 1 gram of cayenne.
In the case of capsules, if for example you don’t like eating hot pepper, this will usually mean taking 2–6 capsules per day, depending on dosage.
Make sure to take it with plenty of water!
Where can we get it?
Fresh peppers or ground spice from your local grocery store is fine. Your local health food store probably sells the supplements, too.
If you’d like to buy it online, here is an example product on Amazon.
Note: options on Amazon were more limited than usual, so this product is not vegan, and probably not halal or kosher, as the capsule contains an unspecified gelatin.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eggplant vs Zucchini – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing eggplant to zucchini, we picked the zucchini.
Why?
In terms of macros, eggplant has more carbs and fiber while zucchini has more protein; we’ll generally prioritize fiber, so call this a subjective win for eggplant in this category, though an argument could be made for a tie.
In the category of vitamins, eggplant has more of vitamins B3, B5, and E, while zucchini has more of vitamins A, B1, B2, B6, B9, C, K, and choline, scoring a win for zucchini here.
Looking at minerals, eggplant has more copper, manganese, and selenium, while zucchini has more calcium, iron, magnesium, phosphorus, potassium and zinc, meaning another win for zucchini in this round.
In terms of polyphenols, eggplant has a greater variety of polyphenols, while zucchini has greater total mass of polyphenols, so we’re calling this one a tie.
Adding up the sections makes for an overall win for zucchini, but by all means enjoy either or both (perhaps together!); diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Simple Japanese Habits For Healthier & Longer Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You don’t have to be Japanese or live in Okinawa to enjoy the benefits of healthy longevity. A lot of it comes down to simple habits:
Easy to implement
We’ll not keep the 10 habits a mystery; they are:
- Start the day with hot water: drinking hot water in the morning helps with hydration, warming the body, and aiding digestion.
- Enjoy a hearty breakfast: Japanese breakfasts are traditionally filling, nutritious, and help promote energy and longevity. Typical components include rice, miso soup, fish, and pickles.
- Take balanced meals: Japanese education emphasizes nutrition from a young age, promoting balanced meals with proteins, fiber, and vitamins & minerals.
- Enjoy fermented foods: fermented foods, such as nattō and soy-based condiments, support digestion, heart health, and the immune system.
- Drink green tea and matcha: both are rich in health benefits; preparing matcha mindfully adds a peaceful ritual to daily life too.
- Keep the “80% full” rule: “hara hachi bu” encourages eating until 80% full, which can improve longevity and, of course, prevent overeating.
- Use multiple small dishes: small servings and a variety of dishes help prevent overeating and ensure a diverse intake of nutrients.
- Gratitude before and after meals: saying “itadakimasu” and “gochisousama” promotes mindful eating, and afterwards, good digestion. Speaking Japanese is of course not the key factor here, but rather, do give yourself a moment of reflection before and after meals.
- Use vinegar in cooking: vinegar, often used in sushi rice and sauces like ponzu, adds flavor and offers health benefits, mostly pertaining to blood sugar balance.
- Eat slowly: Eating at a slower pace will improve digestion, and can enhance satiety and prevent accidentally overeating.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Get More Out Of What’s On Your Plate
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: