When A Period Is Very Late (Post-Menopause)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Knowledge Is Power Safety, Post-Menopause Too
Note: this article will be most relevant for a subset of our subscribership, but it’s a very large subset, so we’re going to go ahead and address the reader as “you”.
If, for example, you are a man and this doesn’t apply to you, we hope it will interest you anyway (we imagine there are women in your life).
PS: the appendicitis check near the end, works for anyone with an appendix
We’ve talked before about things that come with (and continue after) menopause:
- What You Should Have Been Told About The Menopause Beforehand
- What Menopause Does To The Heart
- Alzheimer’s Sex Differences May Not Be What They Appear
But what’s going on if certain menstrual symptoms reappear post-menopause (e.g. after more than a year with no menstruation)?
Bleeding
You should not, of course, be experiencing vaginal bleeding post-menopause. You may have seen “PSA” style posts floating around social media warning that this is a sign of cancer. And, it can be!
But it’s probably not.
Endometrial cancer (the kind that causes such bleeding) affects 2–3% of women, and of those reporting post-menopausal bleeding, the cause is endometrial cancer only 9% of those times.
So in other words, it’s not to be ignored, but for 9 people out of 10 it won’t be cancer:
Read more: Harvard Health | Postmenopausal bleeding: Don’t worry—but do call your doctor
Other more likely causes are uterine fibroids or polyps. These are unpleasant but benign, and can be corrected with surgery if necessary.
The most common cause, however is endometrial and/or vaginal atrophy resulting in tears and bleeding.
Tip: Menopausal HRT will often correct this.
Read more: The significance of “atrophic endometrium” in women with postmenopausal bleeding
(“atrophic endometrium” and “endometrial atrophy” are the same thing)
In summary: no need to panic, but do get it checked out at your earliest convenience. This is not one where we should go “oh that’s weird” and ignore.
Cramps
If you are on menopausal HRT, there is a good chance that these are just period cramps. They may feel different than they did before, because you didn’t ovulate and thus you’re not shedding a uterine lining now, but your body is going to do its best to follow the instructions given by the hormones anyway (hormones are just chemical messengers, after all).
If it is just this, then they will probably settle down to a monthly cycle and become quite predictable.
Tip: if it’s the above, then normal advice for period cramps will go here. We recommend ginger! It’s been found to be as effective as Novafen (a combination drug of acetaminophen (Tylenol), caffeine, and ibuprofen), in the task of relieving menstrual pain:
See: Effect of Ginger and Novafen on menstrual pain: A cross-over trial
It could also be endometriosis. Normally this affects those of childbearing age, but once again, exogenous hormones (as in menopausal HRT) can fool the body into doing it.
If you are not on menopausal HRT (or sometimes even if you are), uterine fibroids (as discussed previously) are once again a fair candidate, and endometriosis is also still possible, though less likely.
Special last note
Important self-check: if you are experiencing a sharp pain in that general area and are worrying if it is appendicitis (also a possibility), then pressing on the appropriately named McBurney’s point is a first-line test for appendicitis. If, after pressing, it hurts a lot more upon removal of pressure (rather than upon application of pressure), this is considered a likely sign of appendicitis. Get thee to a hospital, quickly.
And if it doesn’t? Still get it checked out at your earliest convenience, of course (better safe than sorry), but you might make an appointment instead of calling an ambulance.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reduce Your Skin Tag Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝As I get older, I seem to be increasingly prone to skin tags, which appear, seemingly out of nowhere, on my face, chest and back. My dermatologist happily burns them off – but is there anything I can do to prevent them?!❞
Not a lot! But, potentially something.
The main risk factor for skin tags is genetic, and you can’t change that in any easy way.
The other main risk factors are connected to each other:
Skin folds, and chafing
Skin tags mostly appear where chafing happens. This can be, for example:
- Inside joint articulations (especially groin and armpits)
- Between fat rolls (if you have them)
So, if you have fat rolls, then losing weight will also reduce the risk of skin tags.
Additionally, obesity and some often-related problems such as diabetes, hypertension, and an atherogenic lipid profile also increase the risk of skin tags (amongst other more serious things):
See: Association of Skin Tag with Metabolic Syndrome and its Components
As for the chafing, this can be reduced in various ways, including:
- losing weight if (and only if) you are carrying excess weight
- dressing against chafing (consider your underwear choices, for example)
- keeping hair in the armpits and groin (it’s part of what it’s there for)
See also: Simply The Pits: These Underarm Myths!
Take care!
Share This Post
-
Frozen/Thawed/Refrozen Meat: How Much Is Safety, And How Much Is Taste?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What You Can (And Can’t) Safely Do With Frozen Meat
Yesterday, we asked you:
❝You have meat in the freezer. How long is it really safe to keep it?❞
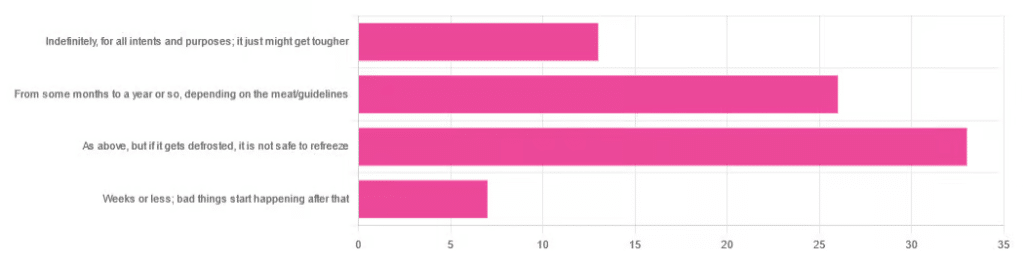
…and got a range of answers, mostly indicating to a) follow the instructions (a very safe general policy) and b) do not refreeze if thawed because that would be unsafe. Fewer respondents indicated that meat could be kept for much longer than guidelines say, or conversely, that it should only be kept for weeks or less.
So, what does the science say?
Meat can be kept indefinitely (for all intents and purposes) in a freezer; it just might get tougher: True or False?
False, assuming we are talking about a normal household electrical freezer that bottoms out at about -18℃ / 0℉.
Fun fact: cryobiologists cryopreserve tissue samples (so basically, meat) at -196℃ / -320℉, and down at those temperatures, the tissues will last a lot longer than you will (and, for all practical purposes: indefinitely). There are other complications with doing so (such as getting the sample through the glass transition point without cracking it during the vitrification process) but those are beyond the scope of this article.
If you remember back to your physics or perhaps chemistry classes at school, you’ll know that molecules move more quickly at higher temperatures, and more slowly at lower ones, only approaching true stillness as they near absolute zero (-273℃ / -459℉ / 0K ← we’re not saying it’s ok, although it is; rather, that is zero kelvin; no degree sign is used with kelvins)
That means that when food is frozen, the internal processes aren’t truly paused; it’s just slowed to a point of near imperceptibility.
So, all the way up at the relatively warm temperatures of a household freezer, a lot of processes are still going on.
What this means in practical terms: those guidelines saying “keep in the freezer for up to 4 months”, “keep in the freezer for up to 9 months”, “keep in the freezer for up to 12 months” etc are being honest with you.
More or less, anyway! They’ll usually underestimate a little to be on the safe side—but so should you.
Bad things start happening within weeks at most: True or False?
False, for all practical purposes. Again, assuming a normal and properly-working household freezer as described above.
(True, technically but misleadingly: the bad things never stopped; they just slowed down to a near imperceptible pace—again, as described above)
By “bad” here we should clarify we mean “dangerous”. One subscriber wrote:
❝Meat starts losing color and flavor after being in the freezer for too long. I keep meat in the freezer for about 2 months at the most❞
…and as a matter of taste, that’s fair enough!
It is unsafe to refreeze meat that has been thawed: True or False?
False! Assuming it has otherwise been kept chilled, just the same as for fresh meat.
Food poisoning comes from bacteria, and there is nothing about the meat previously having been frozen that will make it now have more bacteria.
That means, for example…
- if it was thawed (but chilled) for a period of time, treat it like you would any other meat that has been chilled for that period of time (so probably: use it or freeze it, unless it’s been more than a few days)
- if it was thawed (and at room temperature) for a period of time, treat it like you would any other meat that has been at room temperature for that period of time (so probably: throw it out, unless the period of time is very small indeed)
The USDA gives for 2 hours max at room temperature before considering it unsalvageable, by the way.
However! Whenever you freeze meat (or almost anything with cells, really), ice crystals will form in and between cells. How much ice crystallization occurs depends on several variables, with how much water there is present in the food is usually the biggest factor (remember that animal cells are—just like us—mostly water).
Those ice crystals will damage the cell walls, causing the food to lose structural integrity. When you thaw it out, the ice crystals will disappear but the damage will be left behind (this is what “freezer burn” is).
So if your food seems a little “squishy” after having been frozen and thawed, that’s why. It’s not rotten; it’s just been stabbed countless times on a microscopic level.
The more times you freeze and thaw and refreeze food, the more this will happen. Your food will degrade in structural integrity each time, but the safety of it won’t have changed meaningfully.
Want to know more?
Further reading:
You can thaw and refreeze meat: five food safety myths busted
Take care!
Share This Post
-
Yes, you do need to clean your tongue. Here’s how and why
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Has your doctor asked you to stick out your tongue and say “aaah”? While the GP assesses your throat, they’re also checking out your tongue, which can reveal a lot about your health.
The doctor will look for any changes in the tongue’s surface or how it moves. This can indicate issues in the mouth itself, as well as the state of your overall health and immunity.
But there’s no need to wait for a trip to the doctor. Cleaning your tongue twice a day can help you check how your tongue looks and feels – and improve your breath.
luisrsphoto/Shutterstock What does a healthy tongue look like?
Our tongue plays a crucial role in eating, talking and other vital functions. It is not a single muscle but rather a muscular organ, made up of eight muscle pairs that help it move.
The surface of the tongue is covered by tiny bumps that can be seen and felt, called papillae, giving it a rough surface.
These are sometimes mistaken for taste buds – they’re not. Of your 200,000-300,000 papillae, only a small fraction contain taste buds. Adults have up to 10,000 taste buds and they are invisible to the naked eye, concentrated mainly on the tip, sides and back of the tongue. https://www.youtube.com/embed/uYvpUl7li9Y?wmode=transparent&start=0
A healthy tongue is pink although the shade may vary from person to person, ranging from dark to light pink.
A small amount of white coating can be normal. But significant changes or discolouration may indicate a disease or other issues.
How should I clean my tongue?
Cleaning your tongue only takes around 10-15 seconds, but it’s is a good way to check in with your health and can easily be incorporated into your teeth brushing routine.
Build-up can occur if you stop brushing or scraping your tongue even for a few days. Anthony Shkraba/Pexels You can clean your tongue by gently scrubbing it with a regular toothbrush. This dislodges any food debris and helps prevent microbes building up on its rough textured surface.
Or you can use a special tongue scraper. These curved instruments are made of metal or plastic, and can be used alone or accompanied by scrubbing with your toothbrush.
Your co-workers will thank you as well – cleaning your tongue can help combat stinky breath. Tongue scrapers are particularly effective at removing the bacteria that commonly causes bad breath, hidden in the tongue’s surface.
What’s that stuff on my tongue?
So, you’re checking your tongue during your twice-daily clean, and you notice something different. Noting these signs is the first step. If you observe any changes and they worry you, you should talk to your GP.
Here’s what your tongue might be telling you.
White coating
Developing a white coating on the tongue’s surface is one of the most common changes in healthy people. This can happen if you stop brushing or scraping the tongue, even for a few days.
In this case, food debris and microbes have accumulated and caused plaque. Gentle scrubbing or scraping will remove this coating. Removing microbes reduces the risk of chronic infections, which can be transferred to other organs and cause serious illnesses.
Scrubbing or scraping your tongue only takes around ten seconds and can be done while brushing your teeth. Ketut Subiyanto/Pexels Yellow coating
This may indicate oral thrush, a fungal infection that leaves a raw surface when scrubbed.
Oral thrush is common in elderly people who take multiple medications or have diabetes. It can also affect children and young adults after an illness, due to the temporary suppression of the immune system or antibiotic use.
If you have oral thrush, a doctor will usually prescribe a course of anti-fungal medication for at least a month.
Black coating
Smoking or consuming a lot of strong-coloured food and drink – such as tea and coffee, or dishes with tumeric – can cause a furry appearance. This is known as a black hairy tongue. It’s not hair, but an overgrowth of bacteria which may indicate poor oral hygiene.
Smoking can add to poor oral hygiene and make the tongue look black. Sophon Nawit/Shutterstock Pink patches
Pink patches surrounded by a white border can make your tongue look like a map – this is called “geographic tongue”. It’s not known what causes this condition, which usually doesn’t require treatment.
Pain and inflammation
A red, sore tongue can indicate a range of issues, including:
- nutritional deficiencies such as folic acid or vitamin B12
- diseases including pernicious anaemia, Kawasaki disease and scarlet fever
- inflammation known as glossitis
- injury from hot beverages or food
- ulcers, including cold sores and canker sores
- burning mouth syndrome.
Dryness
Many medications can cause dry mouth, also called xerostomia. These include antidepressants, anti-psychotics, muscle relaxants, pain killers, antihistamines and diuretics. If your mouth is very dry, it may hurt.
What about cancer?
White or red patches on the tongue that can’t be scraped off, are long-standing or growing need to checked out by a dental professional as soon as possible, as do painless ulcers. These are at a higher risk of turning into cancer, compared to other parts of the mouth.
Oral cancers have low survival rates due to delayed detection – and they are on the rise. So checking your tongue for changes in colour, texture, sore spots or ulcers is critical.
Dileep Sharma, Professor and Head of Discipline – Oral Health, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Why Many Nonprofit (Wink, Wink) Hospitals Are Rolling in Money
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One owns a for-profit insurer, a venture capital company, and for-profit hospitals in Italy and Kazakhstan; it has just acquired its fourth for-profit hospital in Ireland. Another owns one of the largest for-profit hospitals in London, is partnering to build a massive training facility for a professional basketball team, and has launched and financed 80 for-profit start-ups. Another partners with a wellness spa where rooms cost $4,000 a night and co-invests with “leading private equity firms.”
Do these sound like charities?
These diversified businesses are, in fact, some of the country’s largest nonprofit hospital systems. And they have somehow managed to keep myriad for-profit enterprises under their nonprofit umbrella — a status that means they pay little or no taxes, float bonds at preferred rates, and gain numerous other financial advantages.
Through legal maneuvering, regulatory neglect, and a large dollop of lobbying, they have remained tax-exempt charities, classified as 501(c)(3)s.
“Hospitals are some of the biggest businesses in the U.S. — nonprofit in name only,” said Martin Gaynor, an economics and public policy professor at Carnegie Mellon University. “They realized they could own for-profit businesses and keep their not-for-profit status. So the parking lot is for-profit; the laundry service is for-profit; they open up for-profit entities in other countries that are expressly for making money. Great work if you can get it.”
Many universities’ most robust income streams come from their technically nonprofit hospitals. At Stanford University, 62% of operating revenue in fiscal 2023 was from health services; at the University of Chicago, patient services brought in 49% of operating revenue in fiscal 2022.
To be sure, many hospitals’ major source of income is still likely to be pricey patient care. Because they are nonprofit and therefore, by definition, can’t show that thing called “profit,” excess earnings are called “operating surpluses.” Meanwhile, some nonprofit hospitals, particularly in rural areas and inner cities, struggle to stay afloat because they depend heavily on lower payments from Medicaid and Medicare and have no alternative income streams.
But investments are making “a bigger and bigger difference” in the bottom line of many big systems, said Ge Bai, a professor of health care accounting at the Johns Hopkins University Bloomberg School of Public Health. Investment income helped Cleveland Clinic overcome the deficit incurred during the pandemic.
When many U.S. hospitals were founded over the past two centuries, mostly by religious groups, they were accorded nonprofit status for doling out free care during an era in which fewer people had insurance and bills were modest. The institutions operated on razor-thin margins. But as more Americans gained insurance and medical treatments became more effective — and more expensive — there was money to be made.
Not-for-profit hospitals merged with one another, pursuing economies of scale, like joint purchasing of linens and surgical supplies. Then, in this century, they also began acquiring parts of the health care systems that had long been for-profit, such as doctors’ groups, as well as imaging and surgery centers. That raised some legal eyebrows — how could a nonprofit simply acquire a for-profit? — but regulators and the IRS let it ride.
And in recent years, partnerships with, and ownership of, profit-making ventures have strayed further and further afield from the purported charitable health care mission in their community.
“When I first encountered it, I was dumbfounded — I said, ‘This not charitable,’” said Michael West, an attorney and senior vice president of the New York Council of Nonprofits. “I’ve long questioned why these institutions get away with it. I just don’t see how it’s compliant with the IRS tax code.” West also pointed out that they don’t act like charities: “I mean, everyone knows someone with an outstanding $15,000 bill they can’t pay.”
Hospitals get their tax breaks for providing “charity care and community benefit.” But how much charity care is enough and, more important, what sort of activities count as “community benefit” and how to value them? IRS guidance released this year remains fuzzy on the issue.
Academics who study the subject have consistently found the value of many hospitals’ good work pales in comparison with the value of their tax breaks. Studies have shown that generally nonprofit and for-profit hospitals spend about the same portion of their expenses on the charity care component.
Here are some things listed as “community benefit” on hospital systems’ 990 tax forms: creating jobs; building energy-efficient facilities; hiring minority- or women-owned contractors; upgrading parks with lighting and comfortable seating; creating healing gardens and spas for patients.
All good works, to be sure, but health care?
What’s more, to justify engaging in for-profit business while maintaining their not-for-profit status, hospitals must connect the business revenue to that mission. Otherwise, they pay an unrelated business income tax.
“Their CEOs — many from the corporate world — spout drivel and turn somersaults to make the case,” said Lawton Burns, a management professor at the University of Pennsylvania’s Wharton School. “They do a lot of profitable stuff — they’re very clever and entrepreneurial.”
The truth is that a number of not-for-profit hospitals have become wealthy diversified business organizations. The most visible manifestation of that is outsize executive compensation at many of the country’s big health systems. Seven of the 10 most highly paid nonprofit CEOs in the United States run hospitals and are paid millions, sometimes tens of millions, of dollars annually. The CEOs of the Gates and Ford foundations make far less, just a bit over $1 million.
When challenged about the generous pay packages — as they often are — hospitals respond that running a hospital is a complicated business, that pharmaceutical and insurance execs make much more. Also, board compensation committees determine the payout, considering salaries at comparable institutions as well as the hospital’s financial performance.
One obvious reason for the regulatory tolerance is that hospital systems are major employers — the largest in many states (including Massachusetts, Pennsylvania, Minnesota, Arizona, and Delaware). They are big-time lobbying forces and major donors in Washington and in state capitals.
But some patients have had enough: In a suit brought by a local school board, a judge last year declared that four Pennsylvania hospitals in the Tower Health system had to pay property taxes because its executive pay was “eye popping” and it demonstrated “profit motives through actions such as charging management fees from its hospitals.”
A 2020 Government Accountability Office report chided the IRS for its lack of vigilance in reviewing nonprofit hospitals’ community benefit and recommended ways to “improve IRS oversight.” A follow-up GAO report to Congress in 2023 said, “IRS officials told us that the agency had not revoked a hospital’s tax-exempt status for failing to provide sufficient community benefits in the previous 10 years” and recommended that Congress lay out more specific standards. The IRS declined to comment for this column.
Attorneys general, who regulate charity at the state level, could also get involved. But, in practice, “there is zero accountability,” West said. “Most nonprofits live in fear of the AG. Not hospitals.”
Today’s big hospital systems do miraculous, lifesaving stuff. But they are not channeling Mother Teresa. Maybe it’s time to end the community benefit charade for those that exploit it, and have these big businesses pay at least some tax. Communities could then use those dollars in ways that directly benefit residents’ health.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ghanaian Red Bean & Sweet Potato Groundnut Stew
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a dish popular in principle throughout West Africa. We say “in principle” because that’s a big place, and there is a lot of regional variation. The archetypal peanut stew is from Senegal (as maafe) or Mali (as tigadèguèna), but for its more balanced nutritional profile we’ve chosen one from Ghana—and since there are regional variations within Ghana too, we should specify that this one is from the south.
If you are allergic to nuts, you can substitute a seed butter (or tahini) for the nut butter, and omit the nuts—this will work in culinary terms and be fine healthwise, but we can’t claim it would be the same dish, having lost its defining ingredient. If your allergy is solely to peanuts, then substituting with any oily nut would work. So, not almonds for example, but cashews or even walnuts would be fine.
You will need
- 1½ lbs sweet potatoes, peeled and cut into ½” cubes
- 2 cups low-sodium vegetable stock
- 2 cans kidney beans, drained, cooked, and rinsed (or 2 cups same; cooked, drained, and rinsed)
- 1 can chopped tomatoes
- ½ cup unsalted dry-roasted peanuts
- 1 onion, chopped
- 1 red bell pepper, deseeded and chopped
- ¼ bulb garlic, finely chopped
- 2 heaped tbsp unsalted peanut butter, minimal (ideally: no) additives
- 2 tsp white miso paste
- 2 tsp grated fresh ginger
- 1 tsp ground cumin
- 1 tsp cayenne pepper
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- ½ tsp coarsely ground nigella seeds
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, or other pan suitable for both frying and fitting the entire stew in. Fry the onions until softened, turn the heat down low, and add the garlic, ginger, red bell pepper, cumin, cayenne, black pepper, and MSG/salt.
2) Add ¼ cup of the vegetable stock, and the sweet potato, and turn the heat back up, on high for about 30 seconds to get it to temperature, and then take it down to a simmer.
3) Stir in the miso paste and chopped tomatoes.
4) Add most of the rest of the vegetable stock, keeping ¼ cup aside. Simmer for about 20 minutes.
5) Stir in the kidney beans, and simmer for about 30 minutes more—the sweet potato should be soft now; if it isn’t, let it simmer a while longer until it is.
6) Combine the peanut butter with the remaining ¼ cup vegetable stock, and blend until smooth. Stir it into the stew.
7) If the stew is looking more like a soup than a stew, take out 1 cup and blend this 1 cup to a purée, adding it back in.
8) Add half the peanuts unto the stew. Taste, and adjust the seasonings if necessary.
9) Crush the remaining peanuts using a pestle and mortar; not too much though; you want them broken into bits, not pulverised.
10) Garnish with the crushed nuts and nigella seeds, and serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we used 4/5 today!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Not To Die – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed this book some years ago, but we’re revisiting it now because:
- It really is a book that should be in every healthspan-enjoyer’s collection
- Our book reviews back then were not as comprehensive as now (though we still generally try to fit into the “it takes about one minute to read this review” idea, sometimes we’ll spend a little extra time).
Dr. Greger (of “Dr. Greger’s Daily Dozen” fame) outlines for us in cold hard facts and stats what’s most likely to be our cause of death. While this is not a cheery premise for a book, he then sets out to work back from there—what could have prevented those specific things?
Thus, while the book doesn’t confer immortality (the title is not “how to not die”, after all), it does teach us how not to die—i.e, from heart disease, lung diseases, brain diseases, digestive cancers, infections, diabetes, high blood pressure, liver disease, blood cancers, kidney disease, breast cancer, suicidal depression, prostate cancer, Parkinson’s disease, and even iatrogenic causes.
This it does with a lot of solid science, explained for the layperson, and/but without holding back when it comes to big words, and a lot of them, at that. If you want to add in daily exercises, just lifting the book could be a start; weighing in at 678 pages, it’s an information-dense tome that’s more likely to be sifted through than read cover-to-cover.
The style is thus dense science somewhat editorialized for lay readability, and well-evidenced with around 3,000 citations. That’s not a typo; there are 178 pages of bibliography at the back with about 15–20 scientific references per page.
In terms of practical use, he does also devote chapters to that, it’s not just all textbook. Indeed, he discusses the reasonings behind the items, portion sizes, and quantities of his “daily dozen” foods, so that the reader will understand how much bang-for-buck they deliver, and then it’ll seem a lot less like an arbitrary list, and more likely to be adopted and maintained.
Bottom line: if you care about not getting life-threatening illnesses (which at the end of the day, come to most people at some point), then this book is a must-read.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: