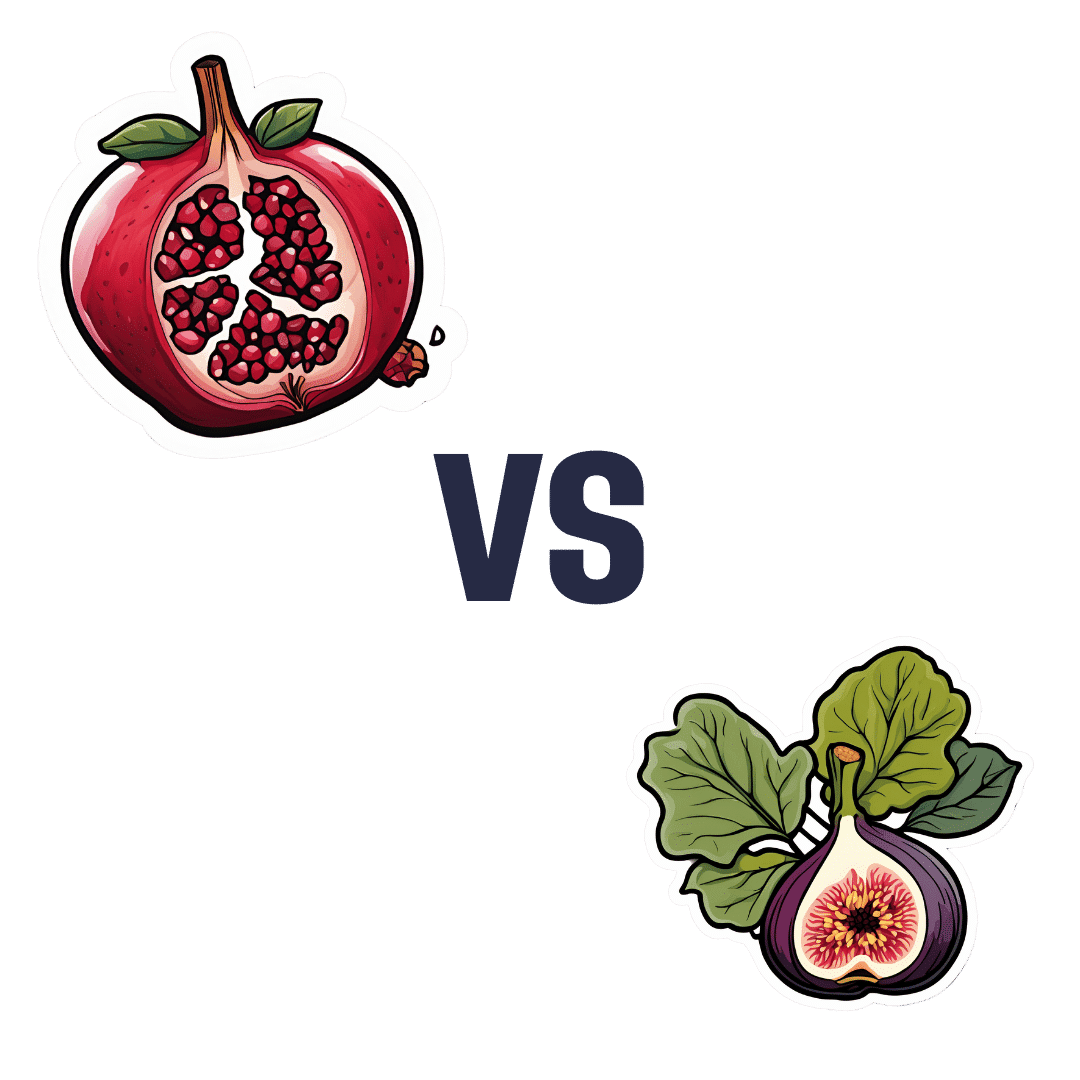
Pomegranate vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to figs, we picked the pomegranate.
Why?
In terms of macros, pomegranate has a lot more protein* and fiber, while the fig has more carbs. Thus, a win for pomegranate.
*Why such protein in a fruit? In both cases, it’s mostly from the seeds, which in both cases, we’re eating. However, pomegranates have a much greater seed-to-mass ratio than figs, and thus, a correspondingly higher amount of protein. Also some fats from the seeds, again more than figs, but the margin of difference is smaller, and not really enough to be of relevance.
In the category of vitamins, pomegranates lead with more of vitamins B1, B5, B9, C, E, K, and choline, while figs have more of vitamins A, B3, and B6. The largest margins of difference are in vitamins B9, E, and K, so all in pomegranate’s favor.
The minerals scene is closer to even; pomegranate has more copper, phosphorus, potassium, selenium, and zinc, while figs have more calcium, iron, magnesium, and manganese. Thus, a 5:4 lead for pomegranate, and the larger margins of difference are again for pomegranate.
In short, enjoy both, but pomegranates are the more nutritionally dense. Also, don’t throw away the peel! Dry it, and turn it into a powdered supplement—see our linked article below, for why:
Want to learn more?
You might like to read:
Pomegranate’s Health Gifts Are Mostly In Its Peel
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Think you’re good at multi-tasking? Here’s how your brain compensates – and how this changes with age
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re all time-poor, so multi-tasking is seen as a necessity of modern living. We answer work emails while watching TV, make shopping lists in meetings and listen to podcasts when doing the dishes. We attempt to split our attention countless times a day when juggling both mundane and important tasks.
But doing two things at the same time isn’t always as productive or safe as focusing on one thing at a time.
The dilemma with multi-tasking is that when tasks become complex or energy-demanding, like driving a car while talking on the phone, our performance often drops on one or both.
Here’s why – and how our ability to multi-task changes as we age.
Doing more things, but less effectively
The issue with multi-tasking at a brain level, is that two tasks performed at the same time often compete for common neural pathways – like two intersecting streams of traffic on a road.
In particular, the brain’s planning centres in the frontal cortex (and connections to parieto-cerebellar system, among others) are needed for both motor and cognitive tasks. The more tasks rely on the same sensory system, like vision, the greater the interference.
This is why multi-tasking, such as talking on the phone, while driving can be risky. It takes longer to react to critical events, such as a car braking suddenly, and you have a higher risk of missing critical signals, such as a red light.
The more involved the phone conversation, the higher the accident risk, even when talking “hands-free”.
Generally, the more skilled you are on a primary motor task, the better able you are to juggle another task at the same time. Skilled surgeons, for example, can multitask more effectively than residents, which is reassuring in a busy operating suite.
Highly automated skills and efficient brain processes mean greater flexibility when multi-tasking.
Adults are better at multi-tasking than kids
Both brain capacity and experience endow adults with a greater capacity for multi-tasking compared with children.
You may have noticed that when you start thinking about a problem, you walk more slowly, and sometimes to a standstill if deep in thought. The ability to walk and think at the same time gets better over childhood and adolescence, as do other types of multi-tasking.
When children do these two things at once, their walking speed and smoothness both wane, particularly when also doing a memory task (like recalling a sequence of numbers), verbal fluency task (like naming animals) or a fine-motor task (like buttoning up a shirt). Alternately, outside the lab, the cognitive task might fall by wayside as the motor goal takes precedence.
Brain maturation has a lot to do with these age differences. A larger prefrontal cortex helps share cognitive resources between tasks, thereby reducing the costs. This means better capacity to maintain performance at or near single-task levels.
The white matter tract that connects our two hemispheres (the corpus callosum) also takes a long time to fully mature, placing limits on how well children can walk around and do manual tasks (like texting on a phone) together.
For a child or adult with motor skill difficulties, or developmental coordination disorder, multi-tastking errors are more common. Simply standing still while solving a visual task (like judging which of two lines is longer) is hard. When walking, it takes much longer to complete a path if it also involves cognitive effort along the way. So you can imagine how difficult walking to school could be.
What about as we approach older age?
Older adults are more prone to multi-tasking errors. When walking, for example, adding another task generally means older adults walk much slower and with less fluid movement than younger adults.
These age differences are even more pronounced when obstacles must be avoided or the path is winding or uneven.
Older adults tend to enlist more of their prefrontal cortex when walking and, especially, when multi-tasking. This creates more interference when the same brain networks are also enlisted to perform a cognitive task.
These age differences in performance of multi-tasking might be more “compensatory” than anything else, allowing older adults more time and safety when negotiating events around them.
Older people can practise and improve
Testing multi-tasking capabilities can tell clinicians about an older patient’s risk of future falls better than an assessment of walking alone, even for healthy people living in the community.
Testing can be as simple as asking someone to walk a path while either mentally subtracting by sevens, carrying a cup and saucer, or balancing a ball on a tray.
Patients can then practise and improve these abilities by, for example, pedalling an exercise bike or walking on a treadmill while composing a poem, making a shopping list, or playing a word game.
The goal is for patients to be able to divide their attention more efficiently across two tasks and to ignore distractions, improving speed and balance.
There are times when we do think better when moving
Let’s not forget that a good walk can help unclutter our mind and promote creative thought. And, some research shows walking can improve our ability to search and respond to visual events in the environment.
But often, it’s better to focus on one thing at a time
We often overlook the emotional and energy costs of multi-tasking when time-pressured. In many areas of life – home, work and school – we think it will save us time and energy. But the reality can be different.
Multi-tasking can sometimes sap our reserves and create stress, raising our cortisol levels, especially when we’re time-pressured. If such performance is sustained over long periods, it can leave you feeling fatigued or just plain empty.
Deep thinking is energy demanding by itself and so caution is sometimes warranted when acting at the same time – such as being immersed in deep thought while crossing a busy road, descending steep stairs, using power tools, or climbing a ladder.
So, pick a good time to ask someone a vexed question – perhaps not while they’re cutting vegetables with a sharp knife. Sometimes, it’s better to focus on one thing at a time.
Peter Wilson, Professor of Developmental Psychology, Australian Catholic University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Are Fruit & Vegetable Extract Supplements Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we are always extolling the virtues of fruits and vegetables, but how much do those benefits still exist when we’re looking at a fruit and vegetable extract supplement?
We examined one aspect of this previously, here;
Mediterranean Diet… In A Pill?
This looked at getting the anti-inflammatory benefits of the Mediterranean diet, in supplement form, by providing extracts of 16 key plant extracts—which also provides an excellent shopping list, by the way, if you just want to skip the supplements and buy those plants; if nine top scientists (anti-aging specialists, neurobiologists, pharmacologists, and at least one professor of applied statistics) came to the conclusion that to get the absolute most bang-for-buck possible, those are the plants to get the phytochemicals from, then we’re not going to ignore that!
And yes, the short answer was “it does very significantly improve anti-inflammatory markers”, by the way.
But when it comes to benefits from polyphenols, anti-inflammatory powers are very much “low-hanging fruit”, so to speak. It’s the “fork found in kitchen” level of shocking revelation. It’s what polyphenols are best at (tied with antioxidant powers, which directly mediate their anti-inflammatory powers).
So, what about something more challenging, like brain benefits?
Underrated Brain Boosters
A European research team (Dr. Begoña Cerdá et al.) looked at the effects of polyphenol-rich nutraceuticals (plant extracts) on cognitive function and neuroprotection biomarkers.
It was a randomized, crossover, double-blind, sex-stratified, placebo-controlled clinical trial that had people take the supplement or a placebo for 16 weeks, have a 4-week washout phase (to minimize leftover effects contaminating the data) and then switching groups (still blinded to the placebo control) for 16 weeks.
They tested cognitive function and neuroprotection biomarkers in various ways before and after each of the testing phases (so, four testing sessions in total per person: before and after the supplement + before and after the placebo).
The results:
❝The results suggested that participants who consumed the polyphenol-rich nutraceutical demonstrated significant improvements in cognitive performance compared to the placebo group.
The Stroop Test scores indicated enhanced attention and inhibitory control, while RIST results suggested improvements in logical reasoning and memory. The Trail Making Test also revealed increased cognitive flexibility, highlighting the supplement’s potential to boost overall mental agility.
Furthermore, the ELISA results showed a notable increase in BDNF and CREB levels among participants who took the active supplement. BDNF is a protein that is essential for neuronal growth and survival, and its levels were significantly elevated, reinforcing its role in synaptic plasticity and long-term memory formation.
Additionally, CREB, a transcription factor involved in learning processes, also showed increased levels, supporting its function in cognitive enhancement.
Importantly, the correlation between improved test scores and higher biomarker levels suggested that polyphenols may directly influence brain function rather than merely offering general health benefits.
While the study focused on healthy adults, the findings also raised questions about whether similar interventions could benefit populations at risk for cognitive decline, including older adults and individuals with neurodegenerative conditions.❞
Key to abbreviations:
- RIST = Reynolds Intellectual Screening Test
- ELISA = Enzyme-Linked ImmunoSorbent Assays
- BDNF = Brain-Derived Neurotrophic Factor
- CREB = cAMP-Response Element Binding Protein
- cAMP = Cyclic Adenosine MonoPhosphate
Source: Daily fruit and vegetable extracts may boost brain power ← we quoted a pop-sci article for the above summary, for easier readability while still having the critical conclusions in one place
For those who do want to dive into the actual data and a lot more detail about the study methodology (which is well worth reading if you have the time, as it’s very good), here is the actual study:
If nothing else, be aware that the usual benchmark for statistical significance is p < 0.05, whereas the results in this study ranged from p < 0.01 to p < 0.001, in other words, ranging from 5x more significant than is required to be called “significant”, to 50x more significant than is required to be called “significant”.
In fewer words: impressively significant
In lay terms: the scientists are about as sure as scientists ever get about anything, that this supplement produces significant results
What was the supplement they tested?
Good news! It was…
- a commercially available supplement (JuicePlus), which is convenient, because it means we (and you, dear reader) can get it if we so choose
- not paid for by JuicePlus or anyone associated with them (indeed, the funding declaration on the study is “This research received no external funding”), so not subject to any conflict of interest that might introduce bias into the study
As for why they chose that one:
❝A unique aspect of the polyphenol-rich nutraceutical evaluated in this study lies in its composition, which integrates a blend of fruit, vegetable, and berry juice powders.
This product, Juice Plus+ Premium®, contains over 119 distinct polyphenolic compounds, including flavanols, anthocyanins, and flavones, as demonstrated in prior compositional analyses.
Compared to other polyphenol-based interventions, this nutraceutical stands out due to its comprehensive formulation, combining a wide range of bioactive compounds with complementary antioxidant and neuroprotective effects.
These characteristics ensure a more diverse interaction with neurobiological pathways, including those related to oxidative stress mitigation, synaptic plasticity, and cognitive function❞
Source: Ibid. (it’s in the introduction)
Want to try some?
We don’t sell it, but for your convenience, here’s where to get JuicePlus supplements Amazon 😎
Enjoy!
Share This Post
-
Is Sugar The New Smoking?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Could you do a this or that of which. Is worse, smoking cigarettes or having a sweet tooth? Also, perhaps have us evaluate one part of newsletter at a time, rather than overall. I especially appreciate your book reviews and often find them through my library system.❞
We’re glad you enjoy the book reviews! We certainly enjoy reading many books to write about them for you.
As for the idea having readers evaluate one part of the newsletter at a time, rather than overall, there is a technical limitation that embedded polls are very large, data-wise, so if we were to do a poll for each section, the email would then get clipped by gmail and other email providers. However, you are always more than welcome to do as you’ve done, and include comments about what section(s) you took the most value from.
Now, onto your main question/request: as it doesn’t quite fit the usual format for our This vs That section, we’ve opted to do it as a main feature here 🙂
So, let’s get into it…
Not a zero-sum game
First, let’s be clear that for most people there is no pressing reason that this should be an either/or decision. There is nothing inherent to quitting either one that makes the other loom larger.
However, that said, if you’re (speaking generally here, and not making any presumptions about the asker) currently smoking regularly and partaking of a lot of added sugar, then you may be wondering which you should prioritize quitting first—as it is indeed generally recommended to only try to quit one thing at a time.
Indeed, we wrote previously, as a guideline for “what to do in one what order”:
Not sure where to start? We suggest this order of priorities, unless you have a major health condition that makes something else a higher priority:
- If you smoke, stop
- If you drink, reduce, or ideally stop
- Improve your diet
About that diet…
Worry less about what to exclude, and instead focus on adding more variety of fruit/veg.
See also: Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
That said, if you’re looking for things to cut, sugar is a top candidate (and red meat is in clear second place albeit some way below)
That’s truncated from a larger list, but those were the top items.
You can read the rest in full, here: The Best Few Interventions For The Best Health: These Top 5 Things Make The Biggest Difference
The flipside of this “you can quit both” reality is that the inverse is also true: much like how having one disease makes it more likely we will get another, unhealthy habits tend to come in clusters too, as each will weaken our resolve with regard to the others. Thus, there is a sort of “comorbidity of habits” that occurs.
The good news is: the same can be said for healthy habits, so they (just like unhealthy habits) can support each other, stack, and compound. This means that while it may seem harder to quit two bad habits than one, in actual fact, the more bad habits you quit, the more it’ll become easy to quit the others. And similarly, the more good habits you adopt, the more it’ll become easy to adopt others.
See also: How To Really Pick Up (And Keep!) Those Habits
So, let’s keep that in mind, while we then look at the cases against smoking, and sugar:
The case against smoking
This is perhaps one of the easiest cases to make in the entirety of the health science world, and the only difficult part is knowing where to start, when there’s so much.
The World Health Organization leads with these key facts, on its tobacco fact sheet:
- Tobacco kills up to half of its users who don’t quit.
- Tobacco kills more than 8 million people each year, including an estimated 1.3 million non-smokers who are exposed to second-hand smoke.
- Around 80% of the world’s 1.3 billion tobacco users live in low- and middle-income countries.
- In 2020, 22.3% of the world’s population used tobacco: 36.7% of men and 7.8% of women.
- To address the tobacco epidemic, WHO Member States adopted the WHO Framework Convention on Tobacco Control (WHO FCTC) in 2003. Currently 182 countries are Parties to this treaty.
- The WHO MPOWER measures are in line with the WHO FCTC and have been shown to save lives and reduce costs from averted healthcare expenditure.
Source: World Health Organization | Tobacco
Now, some of those are just interesting sociological considerations (well, they are of practical use to the WHO whose job it is to offer global health policy guidelines, but for us at 10almonds, with the more modest goal of helping individual people lead their best healthy lives, there’s not so much that we can do with the Framework Convention on Tobacco Control, for example), but for the individual smoker, the first two are really very serious, so let’s take a closer look:
❝Tobacco kills up to half of its users who don’t quit.❞
A bold claim, backed up by at least three very large, very compelling studies:
- Mortality in relation to smoking: 50 years’ observations on male British doctors
- Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence
- Global burden of disease due to smokeless tobacco consumption in adults: an updated analysis of data from 127 countries
❝Tobacco kills more than 8 million people each year, including an estimated 1.3 million non-smokers who are exposed to second-hand smoke.❞
The WHO’s cited source for this was gatekept in a way we couldn’t access (and so probably most of our readers can’t either), but take a look at what the CDC has to say for the US alone (bearing in mind the US’s population of a little over 300,000,000, which is just 3.75% of the global population of a little over 8,000,000,000):
❝smoking causes more than 480,000 deaths [in the US] annually, with an estimated 41,000 deaths from secondhand smoke exposure, and it can reduce a person’s life expectancy by 10 years. Quitting smoking before the age of 40 reduces the risk of dying from smoking-related disease by about 90%❞
If we now remember that third bullet point, that said “Around 80% of the world’s 1.3 billion tobacco users live in low- and middle-income countries.”, then we can imagine the numbers are worse for many other countries, including large-population countries that have a lower median income than the US, such as India and Brazil.
Source for the CDC comment: Tobacco-Related Mortality
See also: AAMC | Smoking is still the leading cause of preventable death in the U.S.
We only have so much room here, but if that’s not enough…
More than 100 reasons to quit tobacco
The case against sugar
We reviewed an interesting book about this:
The Case Against Sugar – by Gary Taubes
But suffice it to say, added sugar is a big health problem; not in the same league as tobacco, but it’s big, because of how it messes with our metabolism (and when our metabolism goes wrong, everything else goes wrong):
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
The epidemiology of sugar consumption and related mortality is harder to give clear stats about than smoking, because there’s not a clear yes/no indicator, and cause and effect are harder to establish when the waters are so muddied by other factors. But for comparison, we’ll note that compared to the 480,000 deaths caused by tobacco in the US annually, the total death to diabetes (which is not necessarily “caused by sugar consumption”, but there’s at least an obvious link when it comes to type 2 diabetes and refined carbohydrates) was 101,209 deaths due to diabetes in 2022:
National Center for Health Statistics | Diabetes
Now, superficially, that looks like “ok, so smoking is just under 5x more deadly”, but it’s important to remember that almost everyone eats added sugar, whereas a minority of people smoke, and those are mortality per total US population figures, not mortality per user of the substance in question. So in fact, smoking is, proportionally to how many people smoke, many times more deadly than diabetes, which currently ranks 8th in the “top causes of death” list.
Note: we recognize that you did say “having a sweet tooth” rather than “consuming added sugar”, but it’s worth noting that artificial sweeteners are not a get-out-of-illness-free card either:
Let’s get back to sugar though, as while it’s a very different beast than tobacco, it is arguably addictive also, by multiple mechanisms of addiction:
The Not-So-Sweet Science Of Sugar Addiction
That said, those mechanisms of addiction are not necessarily as strong as some others, so in the category of what’s easy or hard to quit, this is on the easier end of things—not that that means it’s easy, just, quitting many drugs is harder. In any case, it can be done:
When It’s More Than “Just” Cravings: Beat Food Addictions!
In summary
Neither are good for the health, but tobacco is orders of magnitude worse, and should be the priority to quit, unless your doctor(s) tell you otherwise because of your personal situation, and even then, try to get multiple opinions to be sure.
Take care!
Share This Post
Related Posts
-
Best morning routine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve Got Questions? We’ve Got Answers!
Q: Best morning routine?
A: The best morning routine is whatever makes you feel most ready to take on your day!
This one’s going to vary a lot—one person’s morning run could be another person’s morning coffee and newspaper, for example.
In a nutshell, though, ask yourself these questions:
- How long does it take me to fully wake up in the morning, and what helps or hinders that?
- When I get out of bed, what do I really need before I can take on my day?
- If I could have the perfect morning, what would it look like?
- What can evening me do, to look after morning me’s best interests? (Semi-prepare breakfast ready? Lay out clothes ready? Running shoes? To-Do list?)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
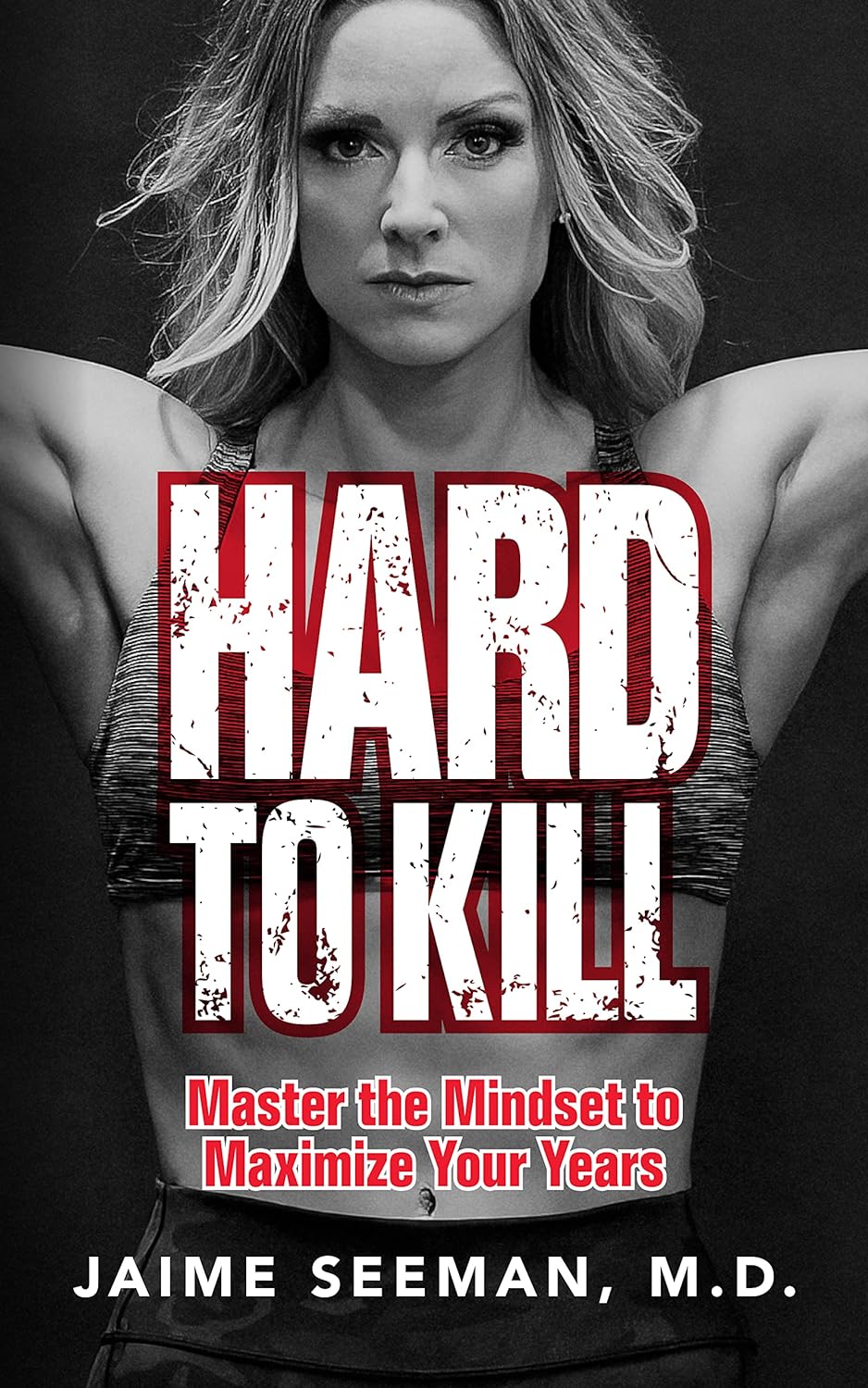
Hard to Kill – by Dr. Jaime Seeman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about Dr. Seeman’s method for robust health at all ages, focussing on:
- Nutrition
- Movement
- Sleep
- Mindset
- Environment
In this book, she expands on these things far more than we have room to in our little newsletter, including (importantly!) how each interplays with the others. She also follows up with an invitation to take the “Hard to Kill 30-Day Challenge”.
That said, in the category of criticism, it’s only 152 pages, and she takes some of that to advertise her online services in an effort to upsell the reader.
Nevertheless, there’s a lot of worth in the book itself, and the writing style is certainly easy-reading and compelling.
Bottom line: this book is half instructional, half motivational, and covers some very important areas of health.
Click here to check out “Hard to Kill”, and enjoy robust health at every age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between wholemeal and wholegrain bread? Not a whole lot
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you head to the shops to buy bread, you’ll face a variety of different options.
But it can be hard to work out the difference between all the types on sale.
For instance, you might have a vague idea that wholemeal or wholegrain bread is healthy. But what’s the difference?
Here’s what we know and what this means for shoppers in Australia and New Zealand.
Phish Photography/Shutterstock Let’s start with wholemeal bread
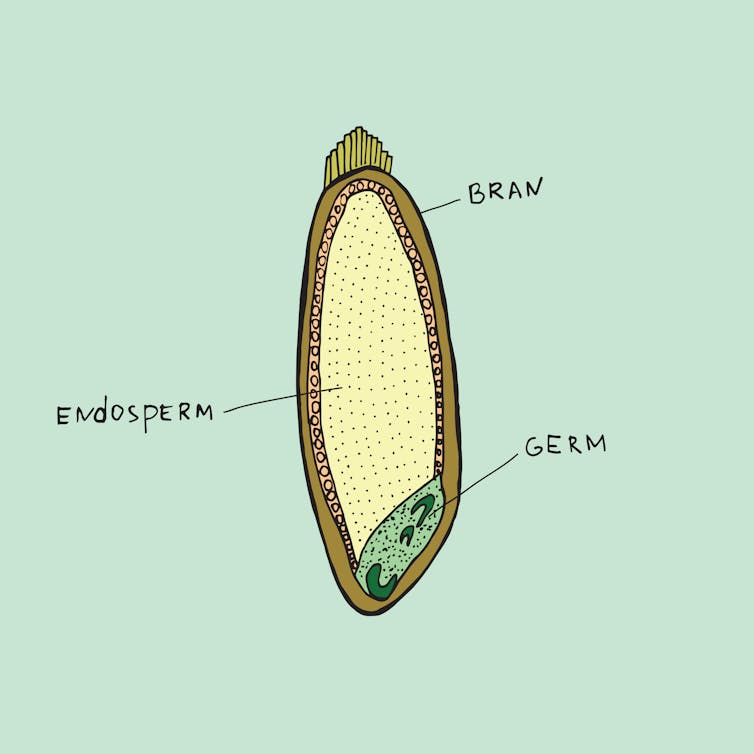
According to Australian and New Zealand food standards, wholemeal bread is made from flour containing all parts of the original grain (endosperm, germ and bran) in their original proportions.
Because it contains all parts of the grain, wholemeal bread is typically darker in colour and slightly more brown than white bread, which is made using only the endosperm.
Wholemeal flour is made from all parts of the grain. Rerikh/Shutterstock How about wholegrain bread?
Australian and New Zealand food standards define wholegrain bread as something that contains either the intact grain (for instance, visible grains) or is made from processed grains (flour) where all the parts of the grain are present in their original proportions.
That last part may sound familiar. That’s because wholegrain is an umbrella term that encompasses both bread made with intact grains and bread made with wholemeal flour. In other words, wholemeal bread is a type of wholegrain bread, just like an apple is a type of fruit.
Don’t be confused by labels such as “with added grains”, “grainy” or “multigrain”. Australian and New Zealand food standards don’t define these so manufacturers can legally add a small amount of intact grains to white bread to make the product appear healthier. This doesn’t necessarily make these products wholegrain breads.
So unless a product is specifically called wholegrain bread, wholemeal bread or indicates it “contains whole grain”, it is likely to be made from more refined ingredients.
Which one’s healthier?
So when thinking about which bread to choose, both wholemeal and wholegrain breads are rich in beneficial compounds including nutrients and fibre, more so than breads made from further-refined flour, such as white bread.
The presence of these compounds is what makes eating wholegrains (including wholemeal bread) beneficial for our overall health. Research has also shown eating wholegrains helps reduce the risk of common chronic diseases, such as heart disease.
The table below gives us a closer look at the nutritional composition of these breads, and shows some slight differences.
Wholegrain bread is slightly higher in fibre, protein, niacin (vitamin B3), iron, zinc, phosphorus and magnesium than wholemeal bread. But wholegrain bread is lower in carbohydrates, thiamin (vitamin B1) and folate (vitamin B9).
However the differences are relatively small when considering how these contribute to your overall dietary intake.
Which one should I buy?
Next time you’re shopping, look for a wholegrain bread (one made from wholemeal flour that has intact grains and seeds throughout) as your number one choice for fibre and protein, and to support overall health.
If you can’t find wholegrain bread, wholemeal bread comes in a very close second.
Wholegrain and wholemeal bread tend to cost the same, but both tend to be more expensive than white bread.
Margaret Murray, Senior Lecturer, Nutrition, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: