In Plain English…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: Love to have someone research all the additives in our medicines, (risk of birth control and breast cancer) and what goes in all of our food and beverages. So much info out there, but there are so many variations, you never know who to believe.
That’s a great idea! There are a lot of medicines and food and beverages out there, so that’s quite a broad brief, but! We could well do a breakdown of very common additives, and demystify them, sorting them into good/bad/neutral, e.g:
- Ascorbic acid—Good! This is Vitamin C
- Acetic acid—Neutral! This is vinegar
- Acetylsalicylic acid—Good or Bad! This is aspirin (a painkiller and blood-thinning agent, can be good for you or can cause more problems than it solves, depending on your personal medical situation. If in doubt, check with your doctor)
- Acesulfame K—Generally Neutral! This is a sweetener that the body can’t metabolize, so it’s also not a source of potassium (despite containing potassium) and will generally do nothing. Unless you have an allergy to it, which is rare but is a thing.
- Sucralose—Neutral! This is technically a sugar (as is anything ending in -ose), but the body can’t metabolize it and processes it as a dietary fiber instead. We’d list it as good for that reason, but honestly, we doubt you’re eating enough sucralose to make a noticeable difference to your daily fiber intake.
- Sucrose—Bad! This is just plain sugar
Sometimes words that sound the same can ring alarm bells when they need not, for example there’s a big difference between:
- Potassium iodide (a good source of potassium and iodine)
- Potassium cyanide (the famous poison; 300mg will kill you; half that dose will probably kill you)
- Cyanocobalamine (Vitamin B12)
Let us know if there are particular additives (or particular medications) you’d like us to look at!
While for legal reasons we cannot give medical advice, talking about common contraindications (e.g., it’s generally advised to not take this with that, as one will stop the other from working, etc) is definitely something we could do.
For example! St. John’s Wort, very popular as a herbal mood-brightener, is on the list of contraindications for so many medications, including:
- Antidepressants
- Birth control pills
- Cyclosporine, which prevents the body from rejecting transplanted organs
- Some heart medications, including digoxin and ivabradine
- Some HIV drugs, including indinavir and nevirapine
- Some cancer medications, including irinotecan and imatinib
- Warfarin, an anticoagulant (blood thinner)
- Certain statins, including simvastatin
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Q: As to specific health topics, I would love to see someone address all these Instagram ads targeted to women that claim “You only need to ‘balance your hormones’ to lose weight, get ripped, etc.” What does this mean? Which hormones are they all talking about? They all seem to be selling a workout program and/or supplements or something similar, as they are ads, after all. Is there any science behind this stuff or is it mostly hot air, as I suspect?
Thank you for asking this, as your question prompted yesterday’s main feature, What Does “Balancing Your Hormones” Even Mean?
That’s a great suggestion also about addressing ads (and goes for health-related things in general, not just hormonal stuff) and examining their claims, what they mean, how they work (if they work!), and what’s “technically true but may be misleading* cause confusion”
*We don’t want companies to sue us, of course.
Only, we’re going to need your help for this one, subscribers!
See, here at 10almonds we practice what we preach. We limit screen time, we focus on our work when working, and simply put, we don’t see as many ads as our thousands of subscribers do. Also, ads tend to be targeted to the individual, and often vary from country to country, so chances are good that we’re not seeing the same ads that you’re seeing.
So, how about we pull together as a bit of a 10almonds community project?
- Step 1: add our email address to your contacts list, if you haven’t already
- Step 2: When you see an ad you’re curious about, select “share” (there is usually an option to share ads, but if not, feel free to screenshot or such)
- Step 3: Send the ad to us by email
We’ll do the rest! Whenever we have enough ads to review, we’ll do a special on the topic.
We will categorically not be able to do this without you, so please do join in—Many thanks in advance!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Stop Negative Thinking – by Daniel Paul
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Just think positive thoughts” is all well and good, but it doesn’t get much mileage in the real world, does it?
What Daniel Paul offers is a lot better than that. Taking a CBT approach, he recommends tips and tricks, gives explanations and exercises, and in short, puts tools in the reader’s toolbox.
But it doesn’t stop at just stopping negative thinking. Rather, it takes a holistic approach to also improve your general life…
- Bookending your day with a good start and finish
- Scheduling a time for any negative thinking that does need to occur (again with the useful realism!)
- Inviting the reader to take on small challenges, of the kind that’ll have knock-on effects that add and multiply and compound as we go
The format is very easy-reading, and we love that there are clear section headings and chapter summaries, too.
Bottom line: definitely a book with the potential to improve your life from day one, and that’ll keep you coming back to it as a cheatsheet and references source.
Get your copy of “How to Stop Negative Thinking” from Amazon today!
Share This Post
-
Plum vs Persimmon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plum to persimmon, we picked the plum.
Why?
Looking at the macros first, persimmon has 3x the carbs for only the same amount of fiber, on account of which plum has the lower glycemic index, so we’ll go with plum here, though your opinion could vary.
In terms of vitamins, it’s much less subjective: plums have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, E, K, and choline, while persimmon has more vitamin C. So, unless you have scurvy, plums will be the best choice for most people.
In the category of minerals, plums have more copper, magnesium, manganese, and zinc, while persimmon has more calcium, iron, phosphorus, and potassium—thus, a 4:4 tie on minerals.
Adding up the sections gives an overall win for plums, but of course, enjoy either or both; diversity is good!
PS: plums have an extra bonus too; check out the link below…
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← plums kill cancer cells while sparing healthy ones
Enjoy!
Share This Post
-
I’ve recovered from a cold but I still have a hoarse voice. What should I do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold, flu, COVID and RSV have been circulating across Australia this winter. Many of us have caught and recovered from one of these common upper respiratory tract infections.
But for some people their impact is ongoing. Even if your throat isn’t sore anymore, your voice may still be hoarse or croaky.
So what happens to the voice when we get a virus? And what happens after?
Here’s what you should know if your voice is still hoarse for days – or even weeks – after your other symptoms have resolved.
Why does my voice get croaky during a cold?
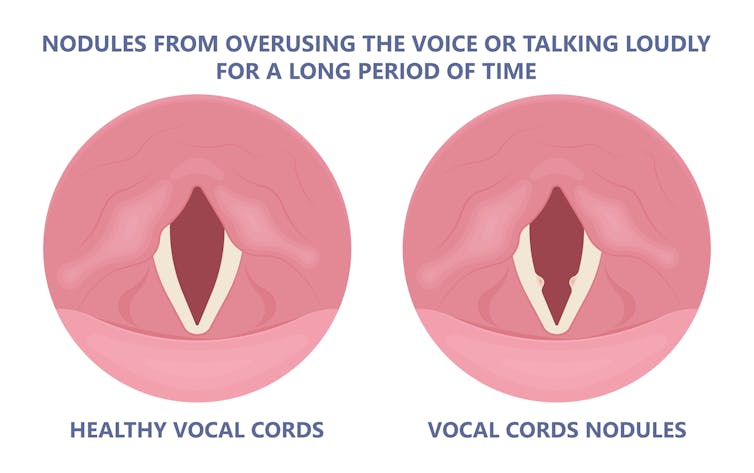
A healthy voice is normally clear and strong. It’s powered by the lungs, which push air past the vocal cords to make them vibrate. These vibrations are amplified in the throat and mouth, creating the voice we hear.
The vocal cords are two elastic muscles situated in your throat, around the level of your laryngeal prominence, or Adam’s apple. (Although everyone has one, it tends to be more pronounced in males.) The vocal cords are small and delicate – around the size of your fingernail. Any small change in their structure will affect how the voice sounds.
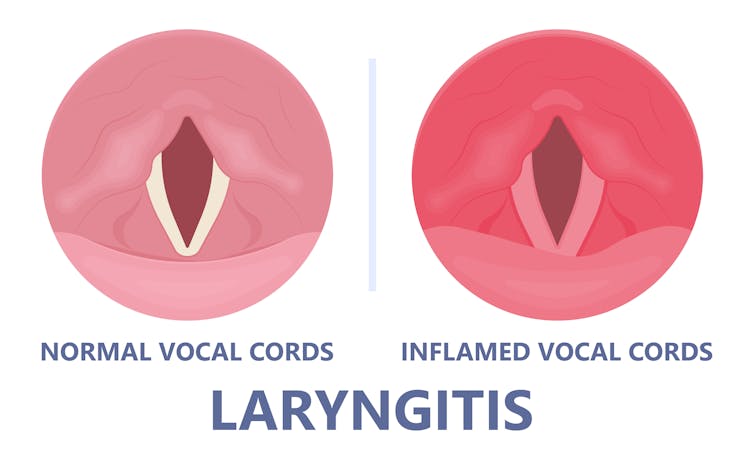
When the vocal cords become inflamed – known as laryngitis – your voice will sound different. Laryngitis is a common part of upper respiratory tract infections, but can also be caused through misuse.
Viruses such as the common cold can inflame the vocal cords. Pepermpron/Shutterstock Catching a virus triggers the body’s defence mechanisms. White blood cells are recruited to kill the virus and heal the tissues in the vocal cords. They become inflamed, but also stiffer. It’s harder for them to vibrate, so the voice comes out hoarse and croaky.
In some instances, you may find it hard to speak in a loud voice or have a reduced pitch range, meaning you can’t go as high or loud as normal. You may even “lose” your voice altogether.
Coughing can also make things worse. It is the body’s way of trying to clear the airways of irritation, including your own mucus dripping onto your throat (post-nasal drip). But coughing slams the vocal cords together with force.
Chronic coughing can lead to persistent inflammation and even thicken the vocal cords. This thickening is the body trying to protect itself, similar to developing a callus when a pair of new shoes rubs.
Thickening on your vocal cords can lead to physical changes in the vocal cords – such as developing a growth or “nodule” – and further deterioration of your voice quality.
Coughing and exertion can cause inflamed vocal cords to thicken and develop nodules. Pepermpron/Shutterstock How can you care for your voice during infection?
People who use their voices a lot professionally – such as teachers, call centre workers and singers – are often desperate to resume their vocal activities. They are more at risk of forcing their voice before it’s ready.
The good news is most viral infections resolve themselves. Your voice is usually restored within five to ten days of recovering from a cold.
Occasionally, your pharmacist or doctor may prescribe cough suppressants to limit additional damage to the vocal cords (among other reasons) or mucolytics, which break down mucus. But the most effective treatments for viral upper respiratory tract infections are hydration and rest.
Drink plenty of water, avoid alcohol and exposure to cigarette smoke. Inhaling steam by making yourself a cup of hot water will also help clear blocked noses and hydrate your vocal cords.
Rest your voice by talking as little as possible. If you do need to talk, don’t whisper – this strains the muscles.
Instead, consider using “confidential voice”. This is a soft voice – not a whisper – that gently vibrates your vocal cords but puts less strain on your voice than normal speech. Think of the voice you use when communicating with someone close by.
During the first five to ten days of your infection, it is important not to push through. Exerting the voice by talking a lot or loudly will only exacerbate the situation. Once you’ve recovered from your cold, you can speak as you would normally.
What should you do if your voice is still hoarse after recovery?
If your voice hasn’t returned to normal after two to three weeks, you should seek medical attention from your doctor, who may refer you to an ear nose and throat specialist.
If you’ve developed a nodule, the specialist would likely refer you to a speech pathologist who will show you how to take care of your voice. Many nodules can be treated with voice therapy and don’t require surgery.
You may have also developed a habit of straining your vocal cords, if you forced yourself to speak or sing while they were inflamed. This can be a reason why some people continue to have a hoarse voice even when they’ve recovered from the cold.
In those cases, a speech pathologist may play a valuable role. They may teach you to exercises that make voicing more efficient. For example, lip trills (blowing raspberries) are a fun and easy way you can learn to relax the voice. This can help break the habit of straining your voice you may have developed during infection.
Yeptain Leung, Postdoctoral Research and Lecturer of Speech Pathology, School of Health Sciences, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
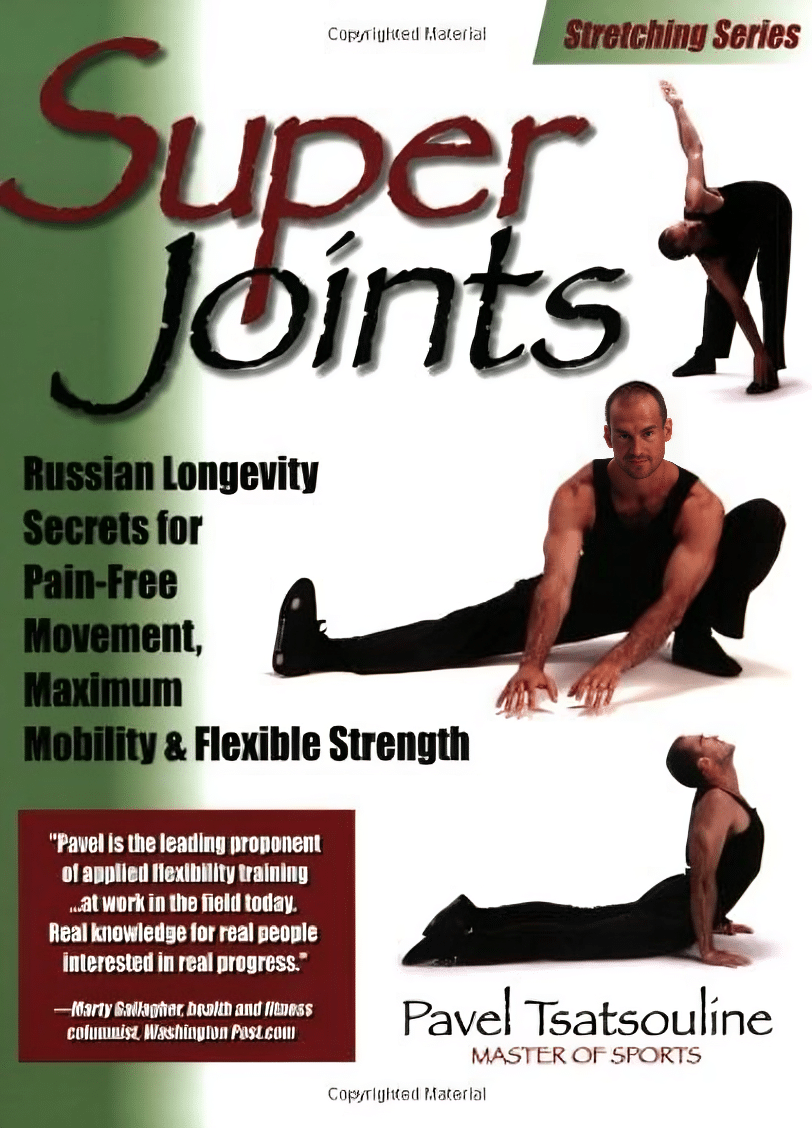
Super Joints – by Pavel Tsatsouline
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those of us for whom mobility and pain-free movement are top priorities, this book has us covered. So what’s different here, compared to your average stretching book?
It’s about functional strength with the stretches. The author’s background as a special forces soldier means that his interest was not in doing arcane yoga positions so much as being able to change direction quickly without losing speed or balance, get thrown down and get back up without injury, twist suddenly without unpleasantly wrenching anything (of one’s own, at least), and generally be able to take knocks without taking damage.
While we are hopefully not having to deal with such violence in our everyday lives, the robustness of body that results from these exercises is one that certainly can go a long way to keep us injury-free.
The exercises themselves are well-described, clearly and succinctly, with equally clear illustrations.
Note: the paperback version is currently expensive, probably due to supply and demand, but if you select the Kindle version, it’s much cheaper with no loss of quality (because the illustrations are black-on-white line-drawings and very clear; perfect for Kindle e-ink)
The style of the book is very casual and conversational, yet somehow doesn’t let that distract it from being incredibly information dense; there is no fluff here, just valuable guidance.
Bottom line: if you would like to be more robust with non-nonsense exercises, then this book is a fine choice.
Click here to check out Super Joints, and make yours flexible and strong!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stickers and wristbands aren’t a reliable way to prevent mosquito bites. Here’s why
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protecting yourself and family from mosquito bites can be challenging, especially in this hot and humid weather. Protests from young children and fears about topical insect repellents drive some to try alternatives such as wristbands, patches and stickers.
These products are sold online as well as in supermarkets, pharmacies and camping stores. They’re often marketed as providing “natural” protection from mosquitoes.
But unfortunately, they aren’t a reliable way to prevent mosquito bites. Here’s why – and what you can try instead.
Why is preventing mosquito bites important?
Mosquitoes can spread pathogens that make us sick. Japanese encephalitis and Murray Valley encephalitis viruses can have potentially fatal outcomes. While Ross River virus won’t kill you, it can cause potentially debilitating illnesses.
Health authorities recommend preventing mosquito bites by: avoiding areas and times of the day when mosquitoes are most active; covering up with long sleeved shirts, long pants, and covered shoes; and applying a topical insect repellent (a cream, lotion, or spray).
I don’t want to put sticky and smelly repellents on my skin!
While for many people, the “sting” of a biting mosquitoes is enough to prompt a dose of repellent, others are reluctant. Some are deterred by the unpleasant feel or smell of insect repellents. Others believe topical repellents contain chemicals that are dangerous to our health.
However, many studies have shown that, when used as recommended, these products are safe to use. All products marketed as mosquito repellents in Australia must be registered by the Australian Pesticides and Veterinary Medicines Authority; a process that provides recommendations for safe use.
How do topical repellents work?
While there remains some uncertainty about how the chemicals in topical insect repellents actually work, they appear to either block the sensory organs of mosquitoes that drive them to bite, or overpower the smells of our skin that helps mosquitoes find us.
Diethytolumide (DEET) is a widely recommended ingredient in topical repellents. Picaridin and oil of lemon eucalyptus are also used and have been shown to be effective and safe.
How do other products work?
“Physical” insect-repelling products, such as wristbands, coils and candles, often contain a botanically derived chemical and are often marketed as being an alternative to DEET.
However, studies have shown that devices such as candles containing citronella oil provide lower mosquito-bite prevention than topical repellents.
A laboratory study in 2011 found wristbands infused with peppermint oil failed to provide full protection from mosquito bites.
Even as topical repellent formulations applied to the skin, these botanically derived products have lower mosquito bite protection than recommended products such as those containing DEET, picaridin and oil of lemon eucalyptus.
Wristbands infused with DEET have shown mixed results but may provide some bite protection or bite reduction. DEET-based wristbands or patches are not currently available in Australia.
There is also a range of mosquito repellent coils, sticks, and other devices that release insecticides (for example, pyrethroids). These chemicals are primarily designed to kill or “knock down” mosquitoes rather than to simply keep them from biting us.
What about stickers and patches?
Although insect repellent patches and stickers have been available for many years, there has been a sudden surge in their marketing through social media. But there are very few scientific studies testing their efficacy.
Our current understanding of the way insect repellents work would suggest these small stickers and patches offer little protection from mosquito bites.
At best, they may reduce some bites in the way mosquito coils containing botanical products work. However, the passive release of chemicals from the patches and stickers is likely to be substantially lower than those from mosquito coils and other devices actively releasing chemicals.
One study in 2013 found a sticker infused with oil of lemon eucalyptus “did not provide significant protection to volunteers”.
Clothing impregnated with insecticides, such as permethrin, will assist in reducing mosquito bites but topical insect repellents are still recommended for exposed areas of skin.
Take care when using these products
The idea you can apply a sticker or patch to your clothing to protect you from mosquito bites may sound appealing, but these devices provide a false sense of security. There is no evidence they are an equally effective alternative to the topical repellents recommended by health authorities around the world. It only takes one bite from a mosquito to transmit the pathogens that result in serious disease.
It is also worth noting that there are some health warnings and recommendations for their use required by Australian Pesticides and Veterinary Medicines Authority. Some of these products warn against application to the skin (recommending application to clothing only) and to keep products “out of reach of children”. This is a challenge if attached to young children’s clothing.
Similar warnings are associated with most other topical and non-topical mosquito repellents. Always check the labels of these products for safe use recommendations.
Are there any other practical alternatives?
Topical insect repellents are safe and effective. Most can be used on children from 12 months of age and pose no health risks. Make sure you apply the repellent as a thin even coat on all exposed areas of skin.
But you don’t need “tropical strength” repellents for short periods of time outdoors; a range of formulations with lower concentrations of repellent will work well for shorter trips outdoors. There are some repellents that don’t smell as strong (for example, children’s formulations, odourless formulations) or formulations that may be more pleasant to use (for example, pump pack sprays).
Finally, you can always cover up. Loose-fitting long-sleeved shirts, long pants, and covered shoes will provide a physical barrier between you and mosquitoes on the hunt for your or your family’s blood this summer.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
New Year, New Health Habits?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of the year, and many of us hope to make this our healthiest year yet—or at least significantly improve it in some particular area that’s important to us! So, what news from the health world?
The rise of GLP-1 agonists continues
GLP-1 agonists have surged in popularity in the past year, and it looks like that trend is set to continue in the new one. The title of the below-linked pop-science article is slightly misleading, it’s not “almost three quarters of UK women”, but rather, “72% of the women using the digital weight loss platform Juniper”, which means the sample is confined to people interested in weight loss. Still, of those interested in weight loss, 72% is a lot, and the sample size was over 1000:
Read in full: New Year, new approach to weight loss: Almost three quarters of UK women are considering using GLP-1s in 2025
Related: 5 ways to naturally boost the “Ozempic Effect” ← these natural methods “hack” the same metabolic pathways as GLP-1 agonists do (it has to do with incretin levels), causing similar results
The lesser of two evils
Smoking is terrible, for everything. Vaping is… Not great, honestly, but as the below-discussed study shows, at the very least it results in much less severe respiratory symptoms than actual smoking. For many, vaping is a halfway-house to actually quitting; for some, it’s just harm reduction, and that too can be worthwhile.
We imagine that probably very few 10almonds readers smoke cigarettes, but we know quite a few use cannabis, which is discussed also:
Read in full: Switching to e-cigarettes may ease respiratory symptoms, offering hope for smokers
Related: Vaping: A Lot Of Hot Air? ← we look at the pros, cons, and popular beliefs that were true a little while ago but now they’re largely not (because of regulatory changes re what’s allowed in vapes)
Sometimes, more is more
The below-linked pop-science article has a potentially confusingly-worded title that makes it sound like increased exercise duration results in decreasing marginal returns (i.e., after a certain point, you’re getting very limited extra benefits), but in fact the study says the opposite.
Rather, increased moderate exercise (so, walking etc) results in a commensurately decreasing weight and a decreasing waistline.
In short: walk more, lose more (pounds and inches). The study examined those who moved their bodies for 150–300 minutes per week:
Read in full: Increased exercise duration linked to decreasing results in weight and waistline
Related: The Doctor Who Wants Us To Exercise Less, & Move More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: