How to Stop Negative Thinking – by Daniel Paul
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Just think positive thoughts” is all well and good, but it doesn’t get much mileage in the real world, does it?
What Daniel Paul offers is a lot better than that. Taking a CBT approach, he recommends tips and tricks, gives explanations and exercises, and in short, puts tools in the reader’s toolbox.
But it doesn’t stop at just stopping negative thinking. Rather, it takes a holistic approach to also improve your general life…
- Bookending your day with a good start and finish
- Scheduling a time for any negative thinking that does need to occur (again with the useful realism!)
- Inviting the reader to take on small challenges, of the kind that’ll have knock-on effects that add and multiply and compound as we go
The format is very easy-reading, and we love that there are clear section headings and chapter summaries, too.
Bottom line: definitely a book with the potential to improve your life from day one, and that’ll keep you coming back to it as a cheatsheet and references source.
Get your copy of “How to Stop Negative Thinking” from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Wholewheat Bread vs Seeded White – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing wholewheat bread to seeded bread, we picked the wholewheat.
Why?
First, we will acknowledge that this is a false dichotomy; it is possible to have seeded wholewheat bread. However, it is very common to have wholewheat bread that isn’t seeded, and white bread that is seeded. So, it’s important to be able to decide which is the healthier option, since very often, this false dichotomy is what’s on offer.
We will also advise checking labels (or the baker, if getting from a bakery) to ensure that visibly brown bread is actually wholewheat, and not just dyed brown with caramel coloring or such (yes, that is a thing that some companies do).
Now, as for why we chose the wholewheat over the seeded white…
In terms of macronutrients, wholewheat bread has (on average; individual breads may vary of course) has 2x the protein and a lot more fiber.
Those seeds in seeded bread? They just aren’t enough to make a big impact on the overall nutritional value of the bread in those regards. Per slice, you are getting, what, 10 seeds maybe? This is not a meaningful dietary source of much.
Seeded bread does have proportionally more healthy fats, but the doses are still so low as to make it not worth the while; it just looks like a lot of expressed as a percentage of comparison, because of the wholewheat bread has trace amounts, and the seeded bread has several times those trace amounts, it’s still a tiny amount. So, we’d recommend looking to other sources for those healthy fats.
Maybe dip your bread, of whatever kind, into extra virgin olive oil, for example.
Wholewheat bread of course also has a lower glycemic index. Those seeds in seeded white bread don’t really slow it down at all, because they’re not digested until later.
Want to learn more?
You might like to read:
- Carb-Strong or Carb-Wrong?
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Gluten: What’s The Truth?
Enjoy!
Share This Post

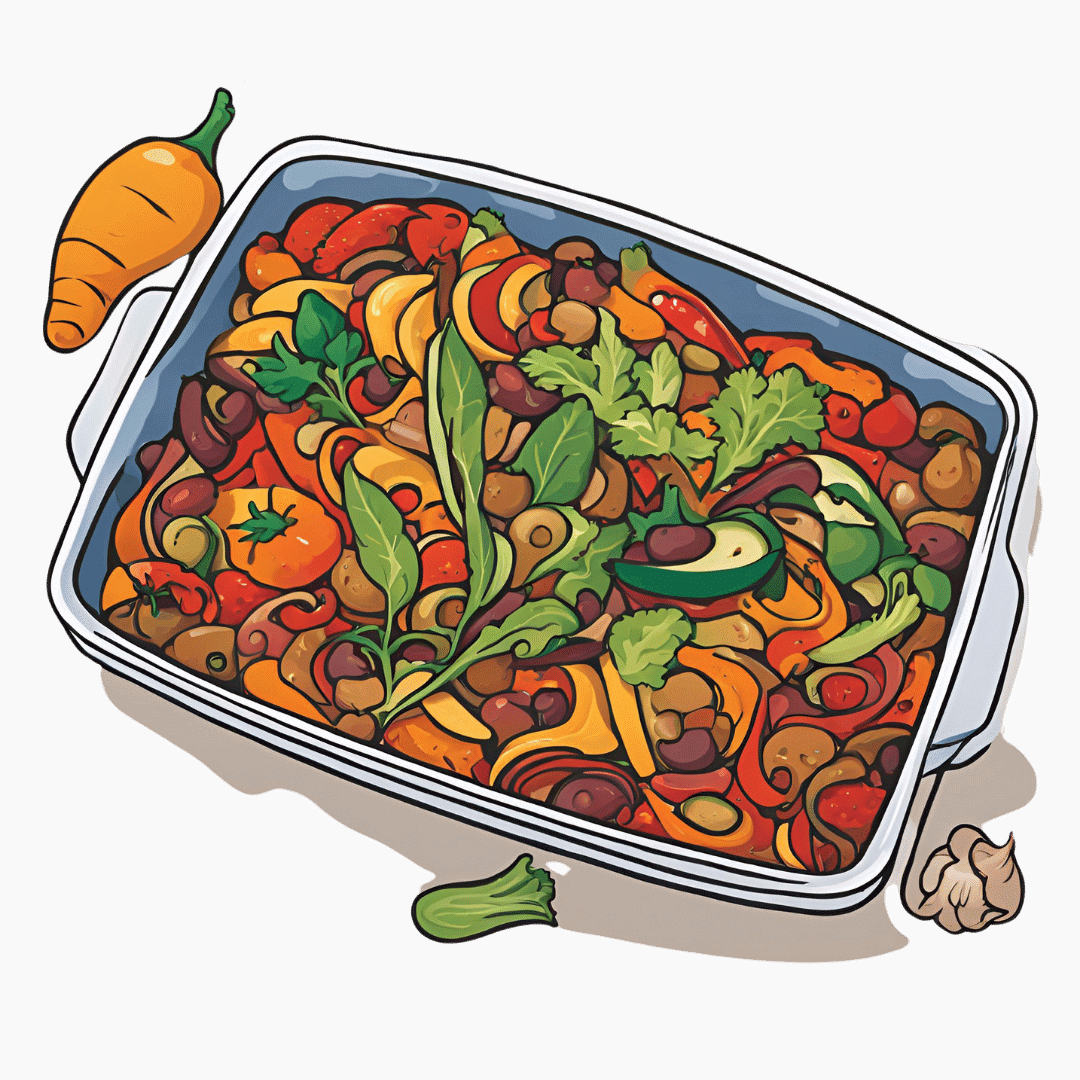
Oven-Roasted Ratatouille
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a supremely low-effort, high-yield dish. It’s a nutritional tour-de-force, and very pleasing to the tastebuds too. We use flageolet beans in this recipe; they are small immature kidney beans. If they’re not available, using kidney beans or really any other legume is fine.
You will need
- 2 large zucchini, sliced
- 2 red peppers, sliced
- 1 large eggplant, sliced and cut into semicircles
- 1 red onion, thinly sliced
- 2 cans chopped tomatoes
- 2 cans flageolet beans, drained and rinsed (or 2 cups same, cooked, drained, and rinsed)
- ½ bulb garlic, crushed
- 2 tbsp extra virgin olive oil
- 1 tbsp balsamic vinegar
- 1 tbsp black pepper, coarse ground
- 1 tbsp nutritional yeast
- 1 tbsp red chili pepper flakes (omit or adjust per your heat preferences)
- ½ tsp MSG or 1 tsp low-sodium salt
- Mixed herbs, per your preference. It’s hard to go wrong with this one, but we suggest leaning towards either basil and oregano or rosemary and thyme. We also suggest having some finely chopped to go into the dish, and some held back to go on the dish as a garnish.
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Mix all the ingredients (except the tomatoes and herbs) in a big mixing bowl, ensuring even distribution.
2) Add the tomatoes. The reason we didn’t add these before is because it would interfere with the oil being distributed evenly across the vegetables.
3) Transfer to a deep-walled oven tray or an ovenproof dish, and roast for 30 minutes.
4) Stir, add the chopped herbs, stir again, and return to the oven for another 30 minutes.
5) Serve (hot or cold), adding any herb garnish you wish to use.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Take care!
Share This Post

Artichoke vs Heart of Palm– Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to heart of palm, we picked the artichoke.
Why?
If you were thinking “isn’t heart of palm full of saturated fat?” then no… Palm oil is, but heart of palm itself has 0.62g/100g fat, of which, 0.13g saturated fat. So, negligible.
As for the rest of the macros, artichoke has more protein, carbs, and fiber, thus being the “more food per food” option. Technically heart of palm has the lower glycemic index, but they are both low-GI foods, so it’s really not a factor here.
Vitamins are where artichoke shines; artichoke has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline, while heart of palm is not higher in any vitamins.
The minerals situation is more balanced: artichoke has more copper, magnesium, phosphorus, and potassium, while heart of palm has more iron, manganese, selenium, and zinc.
Adding up the categories, the winner of this “vegetables with a heart” face-off is clearly artichoke.
Fun fact: in French, “to have the heart of an artichoke” (avoir le coeur d’un artichaut) means to fall in love easily. Perfect vegetable for a romantic dinner, perhaps (especially with all those generous portions of B-vitamins)!
Want to learn more?
You might like to read:
Artichoke vs Cabbage – Which is Healthier?
Take care!
Share This Post
Related Posts

Sweet Dreams Are Made of THC (Or Are They?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I’m one of those older folks that have a hard time getting 7 hrs. I know a lot of it my fault…like a few beers at nite…🥰am now trying THC gummies for anxiety, instead of alcohol……less calories 😁how does THC affect our sleep,? Safer than alcohol…..I know your next article 😊😊😊😊❣️😊alot of us older kids do take gummies 😲😲😲thank you❞
Great question! We wrote a little about CBD gummies (not THC) before:
…and went on to explore THC’s health benefits and risks here:
For starters, let’s go ahead and say: you’re right that it’s safer (for most people) than alcohol—but that’s not a strong claim, because alcohol is very bad for pretty much everything, including sleep.
So how does THC measure up when it comes to sleep quality?
Good news: it affects the architecture of sleep in such a way that you will spend longer in deep sleep (delta wave activity), which means you get more restorative and restful sleep!
See also: Alpha, beta, theta: what are brain states and brain waves? And can we control them?
Bad news: it does so at the cost of reducing your REM sleep, which is also necessary for good brain health, and will cause cognitive impairment if you skip too much. Normally, if you are sleep-deprived, the brain will prioritize REM sleep at the cost of other kinds of sleep; it’s that important. However, if you are chemically impaired from getting healthy REM sleep, there’s not much your brain can do to save you from the effects of REM sleep loss.
See: Cannabis, Cannabinoids, and Sleep: a Review of the Literature
This is, by the way, a reason that THC gets prescribed for some sleep disorders, in cases where the initial sleep disruption was because of nightmares, as it will reduce those (along with any other dreams, as collateral damage):
One thing to be careful of if using THC as a sleep aid is that withdrawal may make your symptoms worse than they were to start with:
Updates in the use of cannabis for insomnia
With all that in mind, you might consider (if you haven’t already tried it) seeing whether CBD alone improves your sleep, as while it does also extend time in deep sleep, it doesn’t reduce REM nearly as much as THC does:
👆 this study was paid for by the brand being tested, so do be aware of potential publication bias. That’s not to say the study is necessarily corrupt, and indeed it probably wasn’t, but rather, the publication of the results was dependent on the company paying for them (so hypothetically they could have pulled funding from any number of other research groups that didn’t get the results they wanted, leaving this one to be the only one published). That being said, the study is interesting, which is why we’ve linked it, and it’s a good jumping-off-point for finding a lot of related papers, which you can see listed beneath it.
CBD also has other benefits of its own, even without THC:
CBD Oil: What Does The Science Say?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Surviving with Beans And Rice – by Eliza Whool
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’d like to be well-set the next time a crisis shuts down supply lines, this is one of those books you’ll want to have read.
Superficially, “have in a large quantity of dried beans and rice” is good advice, but obvious. Why a book?
Whool gives a lot of advice on keeping your nutrition balanced while subsisting on the same quite few ingredients, which is handy.
More than that, she offers 100 recipes using the ingredients that will be in your long-term pantry. That’s over three months without repeating a meal! And if you don’t think rice and beans can be tasty and exciting and varied, then most of the chefs of the Global South might want to have a word about that.
Anyway, we’re not here to sell you rice and beans (we’re just enthusiastic and correct). What we are here to do is to give you a fair overview of this book.
The recipes are just-the-recipes, very simple clear instructions, one two-page spread per recipe. Most of the book is devoted to these. As a quick note, it does cover making things gluten-free if necessary, and other similar adjustments for medical reasons.
The planning-and-storage section of the book is helpful too though, especially as it covers common mistakes to avoid.
Bottom line: this is a great book, and remember what we said about doing the things now that future you will thank you for!
Get yourself a copy of Surviving with Beans And Rice from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

The Sucralose News: Scaremongering Or Serious?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the news on sucralose?
These past days the press has been abuzz with frightening tales:
- This Common Artificial Sweetener Can Break Down DNA, Scientists Warn
- Sucralose Damages DNA, Linked to Leaky Gut
- Chemical found in common sweetener damages DNA
- Chemical found in widely used sweetener breaks up DNA
- Chemical from Splenda breaks up DNA
How true and/or serious is this?
Firstly, let’s manage expectations. Pineapple juice also breaks down DNA, but is not generally considered a health risk. So let’s keep that in mind, while we look into the science.
Is sucralose as scary as pineapple juice, or is it something actually dangerous?
The new study (that sparked off these headlines)
The much-referenced study is publicly available to read in full—here it is:
You may notice that this doesn’t have quite the snappy punchiness of some of the headlines, but let’s break this down, if you’ll pardon the turn of phrase:
- Toxicological: pertaining to whether or not it has toxic qualities
- Pharmacokinetic: the science of asking, of chemicals in bodies, “where did it come from; where did it go; what could it do there; what can we know?”
- Sucralose-6-acetate: an impurity that can be found in sucralose. For perspective, the study found that the sucralose in Splenda contained “up to” 0.67% sucralose-6-acetate.
- Sucralose: a modified form of sucrose, that makes it hundreds of times sweeter, and non-caloric because the body cannot break it down so it’s treated as a dietary fiber and just passes through
- In vitro: things are happening in petri dishes, not in animals (human or otherwise), which would be called “in vivo”
- Screening assays: “we set up a very closed-parameters chemical test, to see what happens when we add this to this” ⇽ oversimplification, but this is the basic format of a screening assay
Great, now we understand the title, but what about the study?
Researchers looked primarily at the effects of sucralose-6-acetate and sucralose (together and separately) on epithelial cells (these are very simple cells that are easy to study; conveniently, they are also most of what makes up our intestinal walls). For this, they used a fancy way of replicating human intestinal walls, that’s actually quite fascinating but beyond the scope of today’s newsletter. Suffice it to say: it’s quite good, and/but has its limitations too. They also looked at some in vivo rat studies.
What they found was…
Based on samples from the rat feces (somehow this didn’t make it into the headlines), it appears that sucralose may be acetylated in the intestines. What that means is that we, if we are like the rats (definitely not a given, but a reasonable hypothesis), might convert up to 10% of sucralose into sucralose-6-acetate inside us. Iff we do, the next part of the findings become more serious.
Based on the in vitro simulations, both sucralose and sucralose-6-acetate reduced intestinal barrier integrity at least a little, but sucralose-6-acetate was the kicker when it came to most of the effects—at least, so we (reasonably!) suppose.
Basically, there’s a lot of supposition going on here but the suppositions are reasonable. That’s how science works; there’s usually little we can know for sure from a single study; it’s when more studies roll in that we start to get a more complete picture.
What was sucralose-6-acetate found to do? It increased the expression of genes associated with inflammation, oxidative stress, and cancer (granted those three things generally go together). So that’s a “this probably has this end result” supposition.
More concretely, and which most of the headlines latched onto, it was found (in vitro) to induce cytogenic damage, specifically, of the clastogenic variety (produces DNA strand breaks—so this is different than pineapple’s bromelain and DNA-helicase’s relatively harmless unzipping of genes).
The dose makes the poison
So, how much is too much and is that 0.67% something to worry about?
- Remembering the rat study, it may be more like 10% once our intestines have done their thing. Iff we’re like rats.
- But, even if it’s only 0.67%, this will still be above the “threshold of toxicological concern for genotoxicity”, of 0.15µg/person/day.
- On the other hand, the fact that these were in vitro studies is a serious limitation.
- Sometimes something is very dangerous in vitro, because it’s being put directly onto cells, whereas in vivo we may have mechanisms for dealing with that.
We won’t know for sure until we get in vivo studies in human subjects, and that may not happen any time soon, if ever, depending on the technical limitations and ethical considerations that sometimes preclude doing certain studies in humans.
Bottom line:
- The headlines are written to be scary, but aren’t wrong; their claims are fundamentally true
- What that means for us as actual humans may not be the same, however; we don’t know yet
- For now, it is probably reasonable to avoid sucralose just in case
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: