Paulina Porizkova (Former Supermodel) Talks Menopause, Aging, & Appearances
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are supermodels destined to all eventually become “Grizabella the Glamor Cat”, a washed-up shell of their former glory? Is it true that “men grow cold as girls grow old, and we all lose our charms in the end”? And what—if anything—can we do about it?
Insights from a retired professional
Paulina Porizkova is 56, and she looks like she’s… 56, maybe? Perhaps a little younger or a bit older depending on the camera and lighting and such.
It’s usually the case, on glossy magazine covers and YouTube thumbnails, that there’s a 20-year difference between appearance and reality, but not here. Why’s that?
Porizkova noted that many celebrities of a similar age look younger, and felt bad. But then she noted that they’d all had various cosmetic work done, and looked for images of “real” women in their mid-50s, and didn’t find them.
Note: we at 10almonds do disagree with one thing here: we say that someone who has had cosmetic work done is no less real for it; it’s a simple matter of personal choice and bodily autonomy. She is, in our opinion, making the same mistake as people make when they say such things as “real people, rather than models”, as though models are not also real people.
Porizkova found modelling highly lucrative but dehumanizing, and did not enjoy the objectification involved—and she enjoyed even less, when she reached a certain age, negative comments about aging, and people being visibly wrong-footed when meeting her, as they had misconceptions based on past images.
As a child and younger adult through her modelling career, she felt very much “seen and not heard”, and these days, she realizes she’s more interesting now but feels less seen. Menopause coincided with her marriage ending, and she felt unattractive and ignored by her husband; she questioned her self-worth, and felt very bad about it. Then her husband (they had separated, but had not divorced) died, and she felt even more isolated—but it heightened her sensitivity to life.
In her pain and longing for recognition, she reached out through her Instagram, crying, and received positive feedback—but still she struggles with expressing needs and feeling worthy.
And yet, when it comes to looks, she embraces her wrinkles as a form of expression, and values her natural appearance over cosmetic alterations.
She describes herself as a work in progress—still broken, still needing cleansing and healing, but proud of how far she’s come so far, and optimistic with regard to the future.
For all this and more in her own words, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Many Faces Of Cosmetic Surgery
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
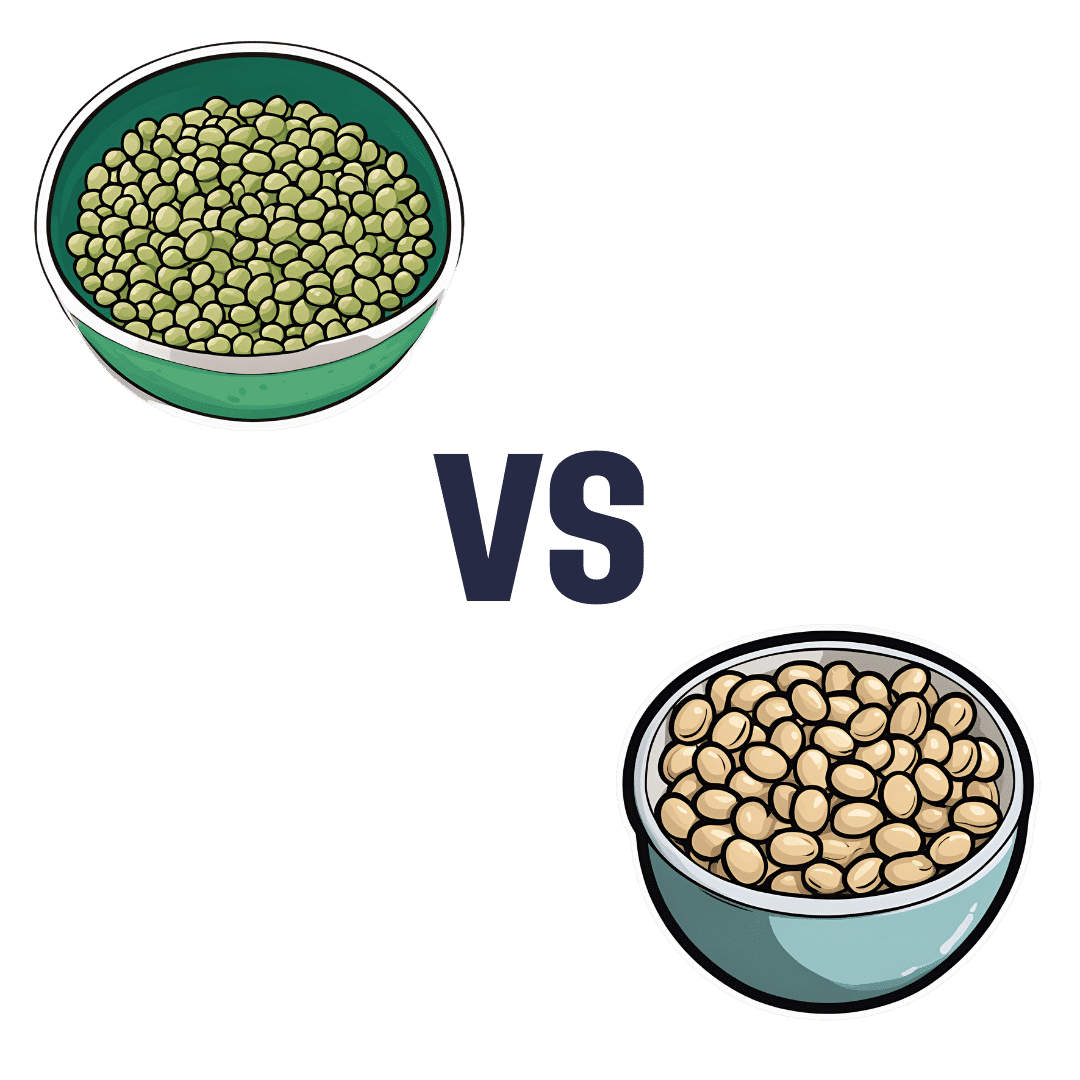
Mung Beans vs Soy Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to soy beans, we picked the soy.
Why?
Mung beans are great, but honestly, it’s not close:
In terms of macronutrients, soy has more than 2x the protein (of which, it’s also a complete protein, containing significant amounts of all essential amino acids) while mung beans have more than 2x the carbs. In their defense, mung beans also have very slightly more fiber, but the carb:fiber ratio is such that soy beans have the lower GI by far.
When it comes to vitamins, mung beans have more of vitamins A, B3, B5, and, B9, while soy beans have more of vitamins B2, B6, C, E, K, and choline, making for a moderate win for soy beans, especially as that vitamin K is more than 7x as much as mung beans have.
In the category of minerals, soy wins even more convincingly; soy beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. On the other hand, mung beans have more sodium.
In short, while mung beans are a very respectable option, they don’t come close to meaningfully competing with soy.
Want to learn more?
You might like to read:
How To Sprout Your Seeds, Grains, Beans, Etc
Take care!
Share This Post
-
How To Stay Alive (When You Really Don’t Want To)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Stay Alive (When You Really Don’t Want To)
A subscriber recently requested:
❝Request: more people need to be aware of suicidal tendencies and what they can do to ward them off❞
…and we said we’d do that one of these Psychology Sundays, so here we are, doing it!
First of all, we’ll mention that we did previously do a main feature on managing depression (in oneself or a loved one); here it is:
The Mental Health First Aid That You’ll Hopefully Never Need
Now, not all depression leads to suicidality, and not all suicide is pre-empted by depression, but there’s a large enough crossover that it seems sensible to put that article here, for anyone who might find it of use, or even just of interest.
Now, onwards, to the specific, and very important, topic of suicide.
This should go without saying, but some of today’s content may be a little heavy.
We invite you to read it anyway if you’re able, because it’s important stuff that we all should know, and not talking about it is part of what allows it to kill people.
So, let’s take a deep breath, and read on…
The risk factors
Top risk factors for suicide include:
- Not talking about it
- Having access to a firearm
- Having a plan of specifically how to commit suicide
- A lack of social support
- Being male
- Being over 40
Now, some of these are interesting sociologically, but aren’t very useful practically; what a convenient world it’d be if we could all simply choose to be under 40, for instance.
Some serve as alarm bells, such as “having a plan of specifically how to commit suicide”.
If someone has a plan, that plan’s never going to disappear entirely, even if it’s set aside!
(this writer is deeply aware of the specifics of how she has wanted to end things before, and has used the advice she gives in this article herself numerous times. So far so good, still alive to write about it!)
Specific advices, therefore, include:
Talk about it / Listen
Depending on whether it’s you or someone else at risk:
- Talk about it, if it’s you
- Listen attentively, if it’s someone else
There are two main objections that you might have at this point, so let’s look at those:
“I have nobody to talk to”—it can certainly feel that way, sometimes, but you may be surprised who would listen if you gave them the chance. If you really can’t trust anyone around you, there are of course suicide hotlines (usually per area, so we’ll not try to list them here; a quick Internet search will get you what you need).
If you’re worried it’ll result in bad legal/social consequences, check their confidentiality policy first:
- Some hotlines can and will call the police, for instance.
- Others deliberately have a set-up whereby they couldn’t even trace the call if they wanted to.
- On the one hand, that means they can’t intervene
- On the other hand, that means they’re a resource for anyone who will only trust a listener who can’t intervene.
“But it is just a cry for help”—then that person deserves help. What some may call “attention-seeking” is, in effect, care-seeking. Listen, without judgement.
Remove access to firearms, if applicable and possible
Ideally, get rid of them (safely and responsibly, please).
If you can’t bring yourself to do that, make them as inconvenient to get at as possible. Stored securely at your local gun club is better than at home, for example.
If your/their plan isn’t firearm-related, but the thing in question can be similarly removed, remove it. You/they do not need that stockpile of pills, for instance.
And of course you/they could get more, but the point is to make it less frictionless. The more necessary stopping points between thinking “I should just kill myself” and being able to actually do it, the better.
Have/give social support
What do the following people have in common?
- A bullied teenager
- A divorced 40-something who just lost a job
- A lonely 70-something with no surviving family, and friends that are hard to visit
Often, at least, the answer is: the absence of a good social support network
So, it’s good to get one, and be part of some sort of community that’s meaningful to us. That could look different to a lot of people, for example:
- A church, or other religious community, if we be religious
- The LGBT+ community, or even just a part of it, if that fits for us
- Any mutual-support oriented, we-have-this-shared-experience community, could be anything from AA to the VA.
Some bonus ideas…
If you can’t live for love, living for spite might suffice. Outlive your enemies; don’t give them the satisfaction.
If you’re going to do it anyway, you might as well take the time to do some “bucket list” items first. After all, what do you have to lose? Feel free to add further bucket list items as they occur to you, of course. Because, why not? Before you know it, you’ve postponed your way into a rich and fulfilling life.
Finally, some gems from Matt Haig’s “The Comfort Book”:
- “The hardest question I have been asked is: “How do I stay alive for other people if I have no one?” The answer is that you stay alive for other versions of you. For the people you will meet, yes, but also the people you will be.”
- “Stay for the person you will become”
- “You are more than a bad day, or week, or month, or year, or even decade”
- “It is better to let people down than to blow yourself up”
- “Nothing is stronger than a small hope that doesn’t give up”
- “You are here. And that is enough.”
You can find Matt Haig’s excellent “The Comfort Book” on Amazon, as well as his more well-known book more specifically on the topic we’ve covered today, “Reasons To Stay Alive“.
Share This Post
-
Dr. Greger’s Anti-Aging Eight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Greger’s Anti-Aging Eight
This is Dr. Michael Greger. We’ve featured him before: Brain Food? The Eyes Have It!
This time, we’re working from his latest book, the excellent “How Not To Age”, which we reviewed all so recently. It is very information-dense, but we’re going to be focussing on one part, his “anti-aging eight”, that is to say, eight interventions he rates the most highly to slow aging in general (other parts of the book pertained to slowing eleven specific pathways of aging, or preserving specific bodily functions against aging, for example).
Without further ado, his “anti-aging eight” are…
- Nuts
- Greens
- Berries
- Xenohormesis & microRNA manipulation
- Prebiotics & postbiotics
- Caloric restriction / IF
- Protein restriction
- NAD+
As you may have noticed, some of these are things might appear already on your grocery shopping list; others don’t seem so “household”. Let’s break them down:
Nuts, greens, berries
These are amongst the most nutrient-dense and phytochemical-useful parts of the diet that Dr. Greger advocates for in his already-famous “Dr. Greger’s Daily Dozen”.
For brevity, we’ll not go into the science of these here, but will advise you: eat a daily portion of nuts, a daily portion of berries, and a couple of daily portions of greens.
Xenohormesis & microRNA manipulation
You might, actually, have these on your grocery shopping list too!
Hormesis, you may recall from previous editions of 10almonds, is about engaging in a small amount of eustress to trigger the body’s self-strengthening response, for example:
Xenohormesis is about getting similar benefits, second-hand.
For example, plants that have been grown to “organic” standards (i.e. without artificial pesticides, herbicides, fertilizers) have had to adapt to their relatively harsher environment by upping their levels of protective polyphenols and other phytochemicals that, as it turns out, are as beneficial to us as they are to the plants:
Hormetic Effects of Phytochemicals on Health and Longevity
Additionally, the flip side of xenohormesis is that some plant compounds can themselves act as a source of hormetic stress that end up bolstering us. For example:
In essence, it’s not just that it has anti-oxidant effect; it also provides a tiny oxidative-stress immunization against serious sources of oxidative stress—and thus, aging.
MicroRNA manipulation is, alas, too complex to truly summarize an entire chapter in a line or two, but it has to do with genetic information from the food that we eat having a beneficial or deleterious effect to our own health:
Diet-derived microRNAs: unicorn or silver bullet?
A couple of quick takeaways (out of very many) from Dr. Greger’s chapter on this is to spring for the better quality olive oil, and skip the cow’s milk:
- Impact of Phenol-Enriched Virgin Olive Oils on the Postprandial Levels of Circulating microRNAs Related to Cardiovascular Disease
- MicroRNA exosomes of pasteurized milk: potential pathogens of Western diseases
Prebiotics & Postbiotics
We’re short on space, so we’ll link you to a previous article, and tell you that it’s important against aging too:
Making Friends With Your Gut (You Can Thank Us Later)
An example of how one of Dr. Greger’s most-recommended postbiotics helps against aging, by the way:
- The mitophagy activator urolithin A is safe and induces a molecular signature of improved mitochondrial and cellular health in humans
- Urolithin A improves muscle strength, exercise performance, and biomarkers of mitochondrial health in a randomized trial in middle-aged adults
(Urolithin can be found in many plants, and especially those containing tannins)
See also: How to Make Urolithin Postbiotics from Tannins
Caloric restriction / Intermittent fasting
This is about lowering metabolic load and promoting cellular apoptosis (programmed cell death; sounds bad; is good) and autophagy (self-consumption; again, sounds bad; is good).
For example, he cites the intermittent fasters’ 46% lower risk of dying in the subsequent years of follow-up in this longitudinal study:
For brevity we’ll link to our previous IF article, but we’ll revisit caloric restriction in a main feature on of these days:
Fasting Without Crashing? We sort the science from the hype!
Dr. Greger favours caloric restriction over intermittent fasting, arguing that it is easier to adhere to and harder to get wrong if one has some confounding factor (e.g. diabetes, or a medication that requires food at certain times, etc). If adhered to healthily, the benefits appear to be comparable for each, though.
Protein restriction
In contrast to our recent main feature Protein vs Sarcopenia, in which that week’s featured expert argued for high protein consumption levels, protein restriction can, on the other hand, have anti-aging effects. A reminder that our body is a complex organism, and sometimes what’s good for one thing is bad for another!
Dr. Greger offers protein restriction as a way to get many of the benefits of caloric restriction, without caloric restriction. He further notes that caloric restriction without protein restriction doesn’t decrease IGF-1 levels (a marker of aging).
However, for FGF21 levels (these are good and we want them higher to stay younger), what matters more than lowering proteins in general is lowering levels of the amino acid methionine—found mostly in animal products, not plants—so the source of the protein matters:
For example, legumes deliver only 5–10% of the methionine that meat does, for the same amount of protein, so that’s a factor to bear in mind.
NAD+
This is about nicotinamide adenine dinucleotide, or NAD+ to its friends.
NAD+ levels decline with age, and that decline is a causal factor in aging, and boosting the levels can slow aging:
Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
Can we get NAD+ from food? We can, but not in useful quantities or with sufficient bioavailability.
Supplements, then? Dr. Greger finds the evidence for their usefulness lacking, in interventional trials.
How to boost NAD+, then? Dr. Greger prescribes…
Exercise! It boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
Another study on resistance training found the same 127% boost:
Take care!
Share This Post
Related Posts
-
America Worries About Health Costs — And Voters Want to Hear From Biden and Republicans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
President Joe Biden is counting on outrage over abortion restrictions to help drive turnout for his reelection. Former President Donald Trump is promising to take another swing at repealing Obamacare.
But around America’s kitchen tables, those are hardly the only health topics voters want to hear about in the 2024 campaigns. A new KFF tracking poll shows that health care tops the list of basic expenses Americans worry about — more than gas, food, and rent. Nearly 3 in 4 adults — and majorities of both parties — say they’re concerned about paying for unexpected medical bills and other health costs.
“Absolutely health care is something on my mind,” Rob Werner, 64, of Concord, New Hampshire, said in an interview at a local coffee shop in January. He’s a Biden supporter and said he wants to make sure the Affordable Care Act, also known as Obamacare, is retained and that there’s more of an effort to control health care costs.
The presidential election is likely to turn on the simple question of whether Americans want Trump back in the White House. (Nikki Haley, the former South Carolina governor and U.S. ambassador to the United Nations, remained in the race for the Republican nomination ahead of Super Tuesday, though she had lost the first four primary contests.) And neither major party is basing their campaigns on health care promises.
But in the KFF poll, 80% of adults said they think it’s “very important” to hear presidential candidates talk about what they’d do to address health care costs — a subject congressional and state-level candidates can also expect to address.
“People are most concerned about out-of-pocket expenses for health care, and rightly so,” said Andrea Ducas, vice president of health policy at the Center for American Progress, a Washington, D.C.-based progressive think tank.
Here’s a look at the major health care issues that could help determine who wins in November.
Abortion
Less than two years after the Supreme Court overturned the constitutional right to an abortion, it is shaping up to be the biggest health issue in this election.
That was also the case in the 2022 midterm elections, when many voters rallied behind candidates who supported abortion rights and bolstered Democrats to an unexpectedly strong showing. Since the Supreme Court’s decision, voters in six states — including Kansas, Kentucky, and Ohio, where Republicans control the legislatures — have approved state constitutional amendments protecting abortion access.
Polls show that abortion is a key issue to some voters, said Robert Blendon, a public opinion researcher and professor emeritus at the Harvard T.H. Chan School of Public Health. He said up to 30% across the board see it as a “personal” issue, rather than policy — and most of those support abortion rights.
“That’s a lot of voters, if they show up and vote,” Blendon said.
Proposals to further protect — or restrict — abortion access could drive voter turnout. Advocates are working to put abortion-related measures on the ballot in such states as Arizona, Florida, Missouri, and South Dakota this November. A push in Washington toward a nationwide abortion policy could also draw more voters to the polls, Blendon said.
A surprise ruling by the Alabama Supreme Court in February that frozen embryos are children could also shake up the election. It’s an issue that divides even the anti-abortion community, with some who believe that a fertilized egg is a unique new person deserving of full legal rights and protections, and others believing that discarding unused embryos as part of the in vitro fertilization process is a morally acceptable way for couples to have children.
Pricey Prescriptions
Drug costs regularly rank high among voters’ concerns.
In the latest tracking poll, more than half — 55% — said they were very worried about being able to afford prescription drugs.
Biden has tried to address the price of drugs, though his efforts haven’t registered with many voters. While its name doesn’t suggest landmark health policy, the Inflation Reduction Act, or IRA, which the president signed in August 2022, included a provision allowing Medicare to negotiate prices for some of the most expensive drugs. It also capped total out-of-pocket spending for prescription drugs for all Medicare patients, while capping the price of insulin for those with diabetes at $35 a month — a limit some drugmakers have extended to patients with other kinds of insurance.
Drugmakers are fighting the Medicare price negotiation provision in court. Republicans have promised to repeal the IRA, arguing that forcing drugmakers to negotiate lower prices on drugs for Medicare beneficiaries would amount to price controls and stifle innovation. The party has offered no specific alternative, with the GOP-led House focused primarily on targeting pharmacy benefit managers, the arbitrators who control most Americans’ insurance coverage for medicines.
Costs of Coverage
Health care costs continue to rise for many Americans. The cost of employer-sponsored health plans have hit new highs in the past few months, raising costs for employers and workers alike. Experts have attributed the increase to high demand and expensive prices for certain drugs and treatments, notably weight loss drugs, as well as to medical inflation.
Meanwhile, the ACA is popular. The KFF poll found that more adults want to see the program expanded than scaled back. And a record 21.3 million people signed up for coverage in 2024, about 5 million of them new customers.
Enrollment in Republican-dominated states has grown fastest, with year-over-year increases of 80% in West Virginia, nearly 76% in Louisiana, and 62% in Ohio, according to the Centers for Medicare & Medicaid Services.
Public support for Obamacare and record enrollment in its coverage have made it politically perilous for Republicans to pursue the law’s repeal, especially without a robust alternative. That hasn’t stopped Trump from raising that prospect on the campaign trail, though it’s hard to find any other Republican candidate willing to step out on the same limb.
“The more he talks about it, the more other candidates have to start answering for it,” said Jarrett Lewis, a partner at Public Opinion Strategies, a GOP polling firm.
“Will a conversation about repeal-and-replace resonate with suburban women in Maricopa County?” he said, referring to the populous county in Arizona known for being a political bellwether. “I would steer clear of that if I was a candidate.”
Biden and his campaign have pounced on Trump’s talk of repeal. The president has said he wants to make permanent the enhanced premium subsidies he signed into law during the pandemic that are credited with helping to increase enrollment.
Republican advisers generally recommend that their candidates promote “a market-based system that has the consumer much more engaged,” said Lewis, citing short-term insurance plans as an example. “In the minds of Republicans, there is a pool of people that this would benefit. It may not be beneficial for everyone, but attractive to some.”
Biden and his allies have criticized short-term insurance plans — which Trump made more widely available — as “junk insurance” that doesn’t cover care for serious conditions or illnesses.
Entitlements Are Off-Limits
Both Medicaid and Medicare, the government health insurance programs that cover tens of millions of low-income, disabled, and older people, remain broadly popular with voters, said the Democratic pollster Celinda Lake. That makes it unlikely either party would pursue a platform that includes outright cuts to entitlements. But accusing an opponent of wanting to slash Medicare is a common, and often effective, campaign move.
Although Trump has said he wouldn’t cut Medicare spending, Democrats will likely seek to associate him with other Republicans who support constraining the program’s costs. Polls show that most voters oppose reducing any Medicare benefits, including by raising Medicare’s eligibility age from 65. However, raising taxes on people making more than $400,000 a year to shore up Medicare’s finances is one idea that won strong backing in a recent poll by The Associated Press and NORC Center for Public Affairs Research.
Brian Blase, a former Trump health adviser and the president of Paragon Health Institute, said Republicans, if they win more control of the federal government, should seek to lower spending on Medicare Advantage — through which commercial insurers provide benefits — to build on the program’s efficiencies and ensure it costs taxpayers less than the traditional program.
So far, though, Republicans, including Trump, have expressed little interest in such a plan. Some of them are clear-eyed about the perils of running on changing Medicare, which cost $829 billion in 2021 and is projected to consume nearly 18% of the federal budget by 2032.
“It’s difficult to have a frank conversation with voters about the future of the Medicare program,” said Lewis, the GOP pollster. “More often than not, it backfires. That conversation will have to happen right after a major election.”
Addiction Crisis
Many Americans have been touched by the growing opioid epidemic, which killed more than 112,000 people in the United States in 2023 — more than gun deaths and road fatalities combined. Rural residents and white adults are among the hardest hit.
Federal health officials have cited drug overdose deaths as a primary cause of the recent drop in U.S. life expectancy.
Republicans cast addiction as largely a criminal matter, associating it closely with the migration crisis at the U.S. southern border that they blame on Biden. Democrats have sought more funding for treatment and prevention of substance use disorders.
“This affects the family, the neighborhood,” said Blendon, the public opinion researcher.
Billions of dollars have begun to flow to states and local governments from legal settlements with opioid manufacturers and retailers, raising questions about how to best spend that money. But it isn’t clear that the crisis, outside the context of immigration, will emerge as a campaign issue.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut-Healthy Labneh Orecchiette
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Labneh (a sort of yogurt-cheese made from strained yogurt) is a great probiotic, and there’s plenty of resistant starch in this dish too, from how we cook, cool, and reheat the pasta. Add to this the lycopene from the tomatoes, the ergothioneine from the mushrooms, and the healthful properties of the garlic, black pepper, and red chili, and we have a very healthy dish!
You will need
- 10 oz labneh (if you can’t buy it locally, you can make your own by straining Greek yogurt through a muslin cloth, suspended over a bowl to catch the water that drips out, overnight—and yes, plant-based is also fine if you are vegan, and the gut benefits are similar because unlike vegan cheese, vegan yogurt is still fermented)
- 6 oz wholegrain orecchiette (or other pasta, but this shape works well for this sauce)
- ¼ bulb garlic, grated
- Juice of ½ lemon
- Large handful chopped parsley
- Large handful chopped dill
- 9 oz cherry tomatoes, halved
- 9 oz mushrooms (your choice what kind), sliced (unless you went for shiitake or similar, which don’t need it due to already being very thin)
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Cook the pasta as you normally would. Drain, and rinse with cold water. Set aside.
2) Combine the labneh with the garlic, black pepper, dill, parsley, and lemon juice, in a large bowl. Set aside.
3) Heat a little olive oil in a skillet; add the chili flakes, followed by the mushrooms. Cook until soft and browned, then add the tomatoes and fry for a further 1 minute—we want the tomatoes to be blistered, but not broken down. Stir in the MSG/salt, and take off the heat.
4) Refresh the pasta by passing a kettle of boiling water through it in a colander, then add the hot pasta to the bowl of labneh sauce, stirring to coat thoroughly.
5) Serve, spooning the mushrooms and tomatoes over the labneh pasta.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dates vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to grapes, we picked the dates.
Why?
It’s not close:
In terms of macros, dates have 4x the carbs and/but 8x the fiber, making for the lower glycemic index. Also, for what it’s worth, they have nearly 4x the protein, but probably nobody is eating either of these fruits for the protein. In any case, it’s an easy and clear win for dates in the category of macros.
In the category of vitamins, dates have more of vitamins B2, B3, B5, B6, B9, and choline, while grapes have more of vitamins B1, C, E, and K, making for a 6:4 win for dates.
When it comes to minerals, it’s more one-sided: dates have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while grapes have more manganese. An easy win for dates here.
Of course, enjoy either or both (diversity is good), but if you’re looking for nutrient density, dates are where it’s at.
Want to learn more?
You might like:
Can We Drink To Good Health? ← while there are polyphenols such as resveratrol in red wine that per se would boost heart health, there’s so little per glass that you may need 100–1000 glasses per day to get the dosage that provides benefits in mouse studies.
If you’re not a mouse, you might even need more than that!
To this end, many people prefer resveratrol supplementation ← link is to an example product on Amazon, but there are plenty more so feel free to shop around 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: