Palliative care as a true art form
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How do you ease the pain from an ailment amidst lost words? How can you serve the afflicted when lines start to blur? When the foundation of communication begins to crumble, what will be the pillar health-care professionals can lean on to support patients afflicted with dementia during their final days?
The practice of medicine is both highly analytical and evidence based in nature. However, it is considered a “practice” because at the highest level, it resembles a musician navigating an instrument. It resembles art. Between lab values, imaging techniques and treatment options, the nuances for individualized patient care so often become threatened.
Dementia, a non-malignant terminal illness, involves the progressive cognitive and social decline in those afflicted. Though there is no cure, dementia is commonly met in the setting of end-of-life care. During this final stage of life, the importance of comfort via symptomatic management and communication usually is a priority in patient care. But what about the care of a patient suffering from dementia? While communication serves as the vehicle to deliver care at a high level, medical professionals are suddenly met with a roadblock. And there … behind the pieces of shattered communication and a dampened map of ethical guidelines, health-care providers are at a standstill.
It’s 4:37 a.m. You receive a text message from the overnight nurse at a care facility regarding a current seizure. After lorazepam is ordered and administered, Mr. H, a quick-witted 76-year-old, stabilizes. Phenobarbital 15mg SC qhs was also added to prevent future similar events. You exhale a sigh of relief.
Mr. H. has been admitted to the floor 36 hours earlier after having a seizure while playing poker with colleagues. Since he became your patient, he’s shared many stories from professional and family life with you, along with as many jokes as he could fit in between. However, over the course of the next seven days, Mr. H. would develop aspiration pneumonia, progressing to ventilator dependency and, ultimately, multi-organ failure with rapid cognitive decline.
What strategies and tools would you use to maximize the well-being of your patient during his decline? How would you bridge the gap of understanding between the patient’s family and health-care team to provide the standard of care that all patients are owed?
To give Mr. H. the type of care he would have wanted, upon his hospital admission, he should have been questioned about his understanding of illness along with the goals of care of the medical team. The patient should have been informed that it is imperative to adhere to the medical regimen implemented by his team along with the risks of not doing so. In the event disease-related complications arose, advanced directives should have been documented to avoid any unnecessary measures.
It is important to note, that with each change in status of the patient’s health status, the goal of treatment must be reassessed. The patient or surrogate decision-maker’s understanding of these goals is paramount in maintaining the patient’s autonomy. It is often said that effective communication is the bedrock of a healthy relationship. This is true regardless of type of relationship.
This is why I and Megan Vierhout wrote Integrated End of Life Care in Dementia: A Comprehensive Guide, a book targeted at providing a much-needed road map to navigate the many challenges involved in end-of-life care for individuals with dementia. Ultimately, our aim is to provide a compass for both health-care professionals and the families of those affected by the progressive effects of dementia. We provide practical advice on optimizing communication with individuals with dementia while taking their cognitive limitations, preferences and needs into account.
I invite you to explore the unpredictable terrain of end-of-life care for patients with dementia. Together, we can pave a smoother, sturdier path toward the practice of medicine as a true art form.
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
New News From The Centenarian Blue Zones
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Blue To Green…
We sometimes write about supercentenarians, which word is usually used in academia to refer to people who are not merely over 100 years of age, but over 110 years. These people can be found in many countries, but places where they have been found to be most populous (as a percentage of the local population) have earned the moniker “Blue Zones”—of which Okinawa and Sardinia are probably the most famous, but there are others too.
This is in contrast to, for example “Red Zones”, a term often used for areas where a particular disease is endemic, or areas where a disease is “merely” epidemic, but particularly rife at present.
In any case, back to the Blue Zones, where people live the longest and healthiest—because the latter part is important too! See also:
- Lifespan: how long we live
- Healthspan: how long we stay healthy (portmanteau of “healthy lifespan”)
Most of our readers don’t live in a Blue Zone (in fact, many live in the US, which is a COVID Red Zone, a diabetes Red Zone, and a heart disease Red Zone), but that doesn’t mean we can’t all take tips from the Blue Zones and apply them, for example:
- The basics: The Blue Zones’ Five Pillars Of Longevity
- Going beyond: The Five Key Traits Of Healthy Aging
You may be wondering… How much good will this do me? And, we do have an answer for that:
When All’s Said And Done, How Likely Are You To Live To 100?
Now that we’re all caught-up…
The news from the Blues
A team of researchers did a big review of observational studies of centenarians and near-centenarians (aged 95+). Why include the near-centenarians, you ask? Well, most of the studies are also longitudinal, and if we’re doing an observational study of the impact of lifestyle factors on a 100-year-old, it’s helpful to know what they’ve been doing recently. Hence nudging the younger-end cutoff a little lower, so as to not begin each study with fresh-faced 100-year-olds whom we know nothing about.
Looking at thousands of centenarians (and near-centenarians, but also including some supercentenarians, up the age of 118), the researchers got a lot of very valuable data, far more than we have room to go into here (do check out the paper at the bottom of this article, if you have time; it’s a treasure trove of data), but one of the key summary findings was a short list of four factors they found contributed the most to extreme longevity:
- A diverse diet with low salt intake: in particular, a wide variety of plant diversity, including protein-rich legumes, though fish featured prominently also. On average they got 57% and 65% of their energy intake from carbohydrates, 12% to 32% from protein, and 27% to 31% from fat. As for salt, they averaged 1.6g of sodium per day, which is well within the WHO’s recommendation of averaging under 2g of sodium per day. As a matter of interest, centenarians in Okinawa itself averaged 1.1g of sodium per day.
- Low medication use: obviously there may be a degree of non-causal association here, i.e. the same people who just happened to be healthier and therefore lived longer, correspondingly took fewer medications—they took fewer medications because they were healthier; they weren’t necessarily healthier because they took fewer medications. That said, overmedication can be a big problem, especially in places with a profit motive like the US, and can increase the risk of harmful drug interactions, and side effects that then need more medications to treat the side effects, as well as direct iatrogenic damage (i.e. this drug treats your condition, but as the cost of harming you in some other way). Naturally, sometimes we really do need meds, but it’s a good reminder to do a meds review with one’s doctor once in a while, and see if everything’s still of benefit.
- Getting good sleep: not shocking, and this one’s not exactly news. But what may be shocking is that 68% of centenarians reported consistently getting enough good-quality sleep. To put that into perspective, only 35% of 10almonds readers reported regularly getting sleep in the 7–9 hours range.
- Rural living environment: more than 75% of the centenarians and near-centenarians lived in rural areas. This is not usually something touted as a Blue Zones thing on lists of Blue zones things, but this review strongly highlighted it as very relevant. In the category of things that are more obvious once it’s pointed out, though, this isn’t necessarily such a difference between “country folk” and “city folk”, so much as the ability to regularly be in green spaces has well-established health benefits physically, mentally, and both combined (such as: neurologically).
And showing that yes, even parks in cities make a significant difference:
Want to know more?
You can read the study in full here:
A systematic review of diet and medication use among centenarians and near-centenarians worldwide
Take care!
Share This Post
-
Vitamin D2 vs Vitamin D3: What You Would Benefit From Knowing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Hi, is there any important difference between vitamin d2 and vitamin d3? Is one better than the other?❞
There is indeed! And one is better than the other!
Where they come from
You’ll find a lot of sources that will tell you “Vitamin D2 is from plants, D3 is from animals”, and in fact only the second half of that is true.
In nature, there are no plants that are known to produce vitamin D.
Vitamin D2, however, is produced by many fungi, as well as algae, neither of which are part of the Kingdom Plantae.
Vitamin D3, meanwhile, is produced by many animals (including humans).
When “the sun” is sometimes considered a source of vitamin D, that’s true only insofar as the sun is also a source of tomatoes, for example, which required the sun to grow. While we humans (and other animals) cannot photosynthesize in general, producing vitamin D is something we can do if exposed to UV light (such as from the sun).
However, of course exposure to UV light (such as from the sun) comes with other problems, so… Should we get sun exposure or not?
We weighed up the balance of evidence, here: The Sun Exposure Dilemma
If, like this writer, you are a mostly crepuscular being who avoids the sun, we have good news: mushrooms can do the sunbathing for us!
❝Exposing mushrooms to UV (from sunlight or in a laboratory) increases the amount of vitamin D in mushrooms by nearly eightfold. Putting five store-bought button mushrooms in the sun, or just one portobello mushroom, produces 24 µg of vitamin D, which translates to nearly 1000 international units, providing the amount of vitamin D one needs in an entire day, and the equivalent found in most vitamin D supplements.
If you’re wondering if the vitamin D from mushrooms actually makes it into your bloodstream, it does. A recent meta-analysis of randomized controlled trials showed that tanned (UV-exposed) mushrooms may be effective in increasing active vitamin D levels in adults with low levels of vitamin D, and studies (randomised controlled trials) have shown that it may be just as effective as supplements at increasing vitamin D levels in the blood (here, and here).
Some research is very positive, saying that putting your mushrooms in direct sunlight for 10–15 minutes may provide you with 100% of your daily vitamin D needs, and the vitamin D content in sunlight-exposed mushrooms may be retained with refrigeration for up to 8 days.
The production of vitamin D may be increased by a further 30% by placing them in the sun with the underside, or gills, facing up, or by 60% if you slice them.❞
Read all about it: Tan your mushrooms, not your skin
Which is better?
In few words: D3 is better.
They both do the exact same job, but with D3, you simply get more bang-for-buck:
❝The WMD in change in total 25(OH)D based on 12 daily dosed vitamin D2-vitamin D3 comparisons, analyzed using liquid chromatography-tandem mass spectrometry, was 10.39 nmol/L (40%) lower for the vitamin D2 group compared with the vitamin D3 group.
Vitamin D3 leads to a greater increase of 25(OH)D than vitamin D2, even if limited to daily dose studies, but vitamin D2 and vitamin D3 had similar positive impacts on their corresponding 25(OH)D hydroxylated forms.❞
Note: “WMD” here means “weighted mean difference”, not “weapons of mass destruction”
About that “and importance of BMI”, by the way: in persons with a BMI >25, there was no longer a difference between the two forms. Literally, no difference at all; the difference was reduced to 0%.
Another study found similarly, but with different numbers (finding a greater difference), and without recording BMI as a factor:
❝D3 is approximately 87% more potent in raising and maintaining serum 25(OH)D concentrations and produces 2- to 3-fold greater storage of vitamin D than does equimolar D2.❞
See the paper: Vitamin D3 Is More Potent Than Vitamin D2 in Humans
“Well that sucks, because I’m vegan”
Fear not, you can get vegan D3 too.
Much like “you can’t get vegan B12” (but you can; it’s made by yeast), there are vegan D3 supplements, made by lichen.
The trouble with lichen, when it comes to classifying it, it that it’s actually a hybrid colony of many small, strange things (beyond the scope of this article, but they are fascinating, so this writer is holding herself back by the scruff of the neck from explaining in detail), some of which are technically part of Kingdom Animalia, but it is hard to find even the most ardent vegan who will object to consuming bacteria, for example.
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
But watch out with the doses, if supplementing vitamin D in either form, because…
Vit D + Calcium: Too Much Of A Good Thing? ← this also talks about safe and effective doses, and what goes wrong if you take too much
Take care!
Share This Post
-
Rosehip’s Benefits, Inside & Out
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s In The Hips
Rosehip (often also written: “rose hip”, “rosehips”, or “rose hips”, but we’ll use the singular compound here to cover its use as a supplement) is often found as an extra ingredient in various supplements, and also various herbal teas. But what is it and what does it actually do?
What it is: it’s the fruiting body that appears on rose plants underneath where the petals appear. They are seasonal.
As for what it does, read on…
Anti-inflammatory
Rosehip is widely sought for (and has been well-studied for) its anti-inflammatory powers.
Because osteoarthritis is one of the most common inflammatory chronic diseases around, a lot of the studies are about OA, but the mechanism of action is well-established as being antioxidant and anti-inflammatory in general:
❝Potent antioxidant radical scavenging effects are well documented for numerous rose hip constituents besides Vitamin C.
Furthermore, anti-inflammatory activities include the reduction of pro-inflammatory cytokines and chemokines, reduction of NF-kB signaling, inhibition of pro-inflammatory enzymes, including COX1/2, 5-LOX and iNOS, reduction of C-reactive protein levels, reduction of chemotaxis and chemoluminescence of PMNs, and an inhibition of pro-inflammatory metalloproteases.❞
Note that while rosehip significantly reduces inflammation, it doesn’t affect the range of movement in OA—further making clear its mechanism of action:
Read: Rosa canina fruit (rosehip) for osteoarthritis: a cochrane review
Anti-aging
This is partly about its antioxidant effect, but when it comes to skin, also partly its high vitamin C content. In this 8-week study, for example, taking 3mg/day resulted in significant reductions of many measures of skin aging:
Heart healthy
The dose required to achieve this benefit is much higher, but nonetheless its effectiveness is clear, for example:
❝Daily consumption of 40 g of rose hip powder for 6 weeks can significantly reduce cardiovascular risk in obese people through lowering of systolic blood pressure and plasma cholesterol levels. ❞
~ Dr. Mona Landin-Olsson et al.
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Share This Post
Related Posts
-
Beat The Heat, With Fat
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Surviving Summer
Summer is upon us, for those of us in the Northern Hemisphere anyway, and given that nowadays each year tends to be hotter than the one before, on average, it pays to be prepared.
We’ve talked about dealing with the heat before:
Sun, Sea, And Sudden Killers To Avoid
All the above advice stands this summer too, but today we’re going to speak a little extra on not having a “default body”.
For much of medical literature and common health advice, the default body is that of a slim and/or athletic white cis man aged 25–35 with no disabilities.
When it comes to “women’s health”, this is often confined to “the bikini zone” and everything else is commonly treated based on research conducted with men.
Today we’ll be looking at a particular challenge for a wide variety of people, when it comes to heat…
Beating the heat, with fat
If you are fat, and/or have a bit of a tummy, and/or have breasts, this one’s for you.
Fat acts as an insulator, which naturally does no favors in hot weather. Carrying the weight around is also extra exercise, which also becomes a problem in hot weather. Fat people usually sweat more than thin people do, as a result.
Sweat is great for cooling down the body, because it takes heat with it when it evaporates off. However, that only works if it can evaporate off, and it can’t evaporate off if it’s trapped in a skin fold / fat roll.
If you’re fat, you may have plenty of those; if you have a bit of a tummy (if you’re not fat generally, this might be a leftover from pregnancy, or weight loss, or something else; how it got there doesn’t matter for our purposes today), you’ll have at least one under it, and if you have breasts, unless they’re quite small, you’ll have one under each breast, and potentially your cleavage may become an issue too.
Note: if you are perhaps a man who has fat in the place where breasts go, then medically this goes for you too, except that there’s not a societal expectation that you wear bra. Use today’s information as you see fit.
Sweat-wicking hacks
We don’t want sweat to stay in those folds—both because then it’s not doing its cooling-down job, and also, because it can cause a rash, and even yeast infections and/or bacterial infections.
So, we want there to be some barrier there. You could use something like vaseline or baby powder, as to prevent chafing, but fat better (more effective, and less messy) is to have some kind of cloth there that can wick the sweat away.
There are made-for-purpose curved cotton bands that exist, called “tummy liners”; here’s an example product on Amazon, or you could make your own if you’re so inclined. They’re breathable, absorbent, and reduce friction too, making everything a lot more comfortable.
And for breasts? Same deal, there are made-for-purpose cotton bra-liners that exist; here’s an example product on Amazon, or again, you could make your own if you feel so inclined. The important part is that it makes things so much comfortable, because let’s face it: wearing a bra in the summer is not comfortable.
So with these, it can become more comfortable (and the cotton liners are flat, so they’re not visible if one’s wearing a t-shirt or similar-coverage garment). You could go braless, of course, but then you’re back to having sweaty folds, so if you’re doing something other than swimming or lying on your back, you might want something there.
Different hydration rules
“People should drink this much per day” and guess what, those guidelines were based on, drumroll please, not fat people.
Sweating more means needing to hydrate more, and even without breaking a sweat, having a larger body than average (be it muscle, fat, or both) means having more body to hydrate. That’s simple math.
So instead, a good general guideline is half an ounce of water per your weight in pounds, per day:
How much water do I need each day?
Another good general guideline is to simply drink “little and often”, that is to say, always have a (hydrating!) drink on the go.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why do some people’s hair and nails grow quicker than mine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout recorded history, our hair and nails played an important role in signifying who we are and our social status. You could say, they separate the caveman from businessman.
It was no surprise then that many of us found a new level of appreciation for our hairdressers and nail artists during the COVID lockdowns. Even Taylor Swift reported she cut her own hair during lockdown.
So, what would happen if all this hair and nail grooming got too much for us and we decided to give it all up. Would our hair and nails just keep on growing?
The answer is yes. The hair on our head grows, on average, 1 centimeter per month, while our fingernails grow an average of just over 3 millimetres.
When left unchecked, our hair and nails can grow to impressive lengths. Aliia Nasyrova, known as the Ukrainian Rapunzel, holds the world record for the longest locks on a living woman, which measure an impressive 257.33 cm.
When it comes to record-breaking fingernails, Diana Armstrong from the United States holds that record at 1,306.58 cm.
Most of us, however, get regular haircuts and trim our nails – some with greater frequency than others. So why do some people’s hair and nails grow more quickly?
Jari Lobo/Pexels Remind me, what are they made out of?
Hair and nails are made mostly from keratin. Both grow from matrix cells below the skin and grow through different patterns of cell division.
Nails grow steadily from the matrix cells, which sit under the skin at the base of the nail. These cells divide, pushing the older cells forward. As they grow, the new cells slide along the nail bed – the flat area under the fingernail which looks pink because of its rich blood supply.
Nails, like hair, are made mostly of keratin. Scott Gruber/Unsplash A hair also starts growing from the matrix cells, eventually forming the visible part of the hair – the shaft. The hair shaft grows from a root that sits under the skin and is wrapped in a sac known as the hair follicle.
This sac has a nerve supply (which is why it hurts to pull out a hair), oil-producing glands that lubricate the hair and a tiny muscle that makes your hair stand up when it’s cold.
At the follicle’s base is the hair bulb, which contains the all-important hair papilla that supplies blood to the follicle.
Matrix cells near the papilla divide to produce new hair cells, which then harden and form the hair shaft. As the new hair cells are made, the hair is pushed up above the skin and the hair grows.
But the papilla also plays an integral part in regulating hair growth cycles, as it sends signals to the stem cells to move to the base of the follicle and form a hair matrix. Matrix cells then get signals to divide and start a new growth phase.
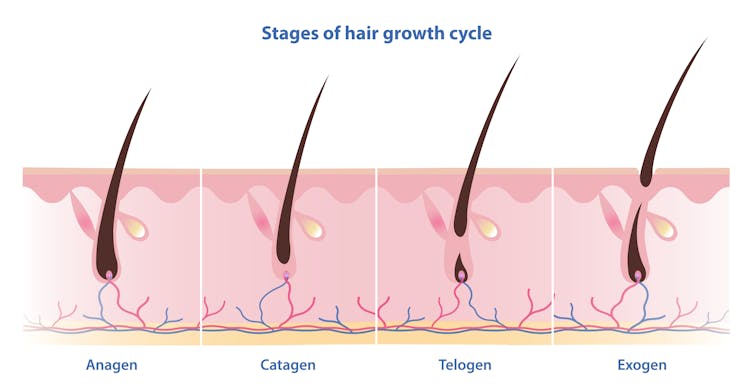
Unlike nails, our hair grows in cycles
Scientists have identified four phases of hair growth, the:
- anagen or growth phase, which lasts between two and eight years
- catagen or transition phase, when growth slows down, lasting around two weeks
- telogen or resting phase, when there is no growth at all. This usually lasts two to three months
- exogen or shedding phase, when the hair falls out and is replaced by the new hair growing from the same follicle. This starts the process all over again.
Hair follicles enter these phases at different times so we’re not left bald. Mosterpiece/Shutterstock Each follicle goes through this cycle 10–30 times in its lifespan.
If all of our hair follicles grew at the same rate and entered the same phases simultaneously, there would be times when we would all be bald. That doesn’t usually happen: at any given time, only one in ten hairs is in the resting phase.
While we lose about 100–150 hairs daily, the average person has 100,000 hairs on their head, so we barely notice this natural shedding.
So what affects the speed of growth?
Genetics is the most significant factor. While hair growth rates vary between individuals, they tend to be consistent among family members.
Nails are also influenced by genetics, as siblings, especially identical twins, tend to have similar nail growth rates.
Genetics have the biggest impact on growth speed. Cottonbro Studio/Pexels But there are also other influences.
Age makes a difference to hair and nail growth, even in healthy people. Younger people generally have faster growth rates because of the slowing metabolism and cell division that comes with ageing.
Hormonal changes can have an impact. Pregnancy often accelerates hair and nail growth rates, while menopause and high levels of the stress hormone cortisol can slow growth rates.
Nutrition also changes hair and nail strength and growth rate. While hair and nails are made mostly of keratin, they also contain water, fats and various minerals. As hair and nails keep growing, these minerals need to be replaced.
That’s why a balanced diet that includes sufficient nutrients to support your hair and nails is essential for maintaining their health.
Nutrition can impact hair and nail growth. Cottonbro Studio/Pexels Nutrient deficiencies may contribute to hair loss and nail breakage by disrupting their growth cycle or weakening their structure. Iron and zinc deficiencies, for example, have both been linked to hair loss and brittle nails.
This may explain why thick hair and strong, well-groomed nails have long been associated with perception of good health and high status.
However, not all perceptions are true.
No, hair and nails don’t grow after death
A persistent myth that may relate to the legends of vampires is that hair and nails continue to grow after we die.
In reality, they only appear to do so. As the body dehydrates after death, the skin shrinks, making hair and nails seem longer.
Morticians are well aware of this phenomenon and some inject tissue filler into the deceased’s fingertips to minimise this effect.
So, it seems that living or dead, there is no escape from the never-ending task of caring for our hair and nails.
Michelle Moscova, Adjunct Associate Professor, Anatomy, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ozempic vs Five Natural Supplements
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (GLP-1 agonist) drugs Ozempic and Wegovy really do work for losing weight, provided one then remains on these expensive drugs for life. Dr. Jin Sung recommends a supplements-based approach, instead.
Natural Alternatives
Dr. Sung recommends:
- Berberine, which increases production and secretion of GLP-1.
- Probiotics, which increase GLP-1 secretion. In particular he recommends Akkermansia municiphila which secretes P9, and this protein stimulates GLP-1 production and secretion.
- Psyllium, a soluble dietary fiber which will increase short-chain fatty acids which then help with increasing GLP-1.
- Curcumin, which enhances L-cell numbers, in turn promoting and increasing GLP-1 secretion. Also, curcumin may prolong gastric emptying, and increase insulin sensitivity.
- Ginseng, of which the bioactive compound stimulates secretion of GLP-1, and also has anti-diabetic effects.
Dr. Sung explains more about each of these in his video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might enjoy our previous main feature looking at some of the pros and cons:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: