Lost for words? Research shows art therapy brings benefits for mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Creating art for healing purposes dates back tens of thousands of years, to the practices of First Nations people around the world. Art therapy uses creative processes, primarily visual art such as painting, drawing or sculpture, with a view to improving physical health and emotional wellbeing.
When people face significant physical or mental ill-health, it can be challenging to put their experiences into words. Art therapists support people to explore and process overwhelming thoughts, feelings and experiences through a reflective art-making process. This is distinct from art classes, which often focus on technical aspects of the artwork, or the aesthetics of the final product.
Art therapy can be used to support treatment for a wide range of physical and mental health conditions. It has been linked to benefits including improved self-awareness, social connection and emotional regulation, while lowering levels of distress, anxiety and even pain scores.
In a study published this week in the Journal of Mental Health, we found art therapy was associated with positive outcomes for children and adolescents in a hospital-based mental health unit.
An option for those who can’t find the words
While a person’s engagement in talk therapies may sometimes be affected by the nature of their illness, verbal reflection is optional in art therapy.
Where possible, after finishing an artwork, a person can explore the meaning of their work with the art therapist, translating unspoken symbolic material into verbal reflection.
However, as the talking component is less central to the therapeutic process, art therapy is an accessible option for people who may not be able to find the words to describe their experiences.
Art therapy has supported improved mental health outcomes for people who have experienced trauma, people with eating disorders, schizophrenia and dementia, as well as children with autism.
Art therapy has also been linked to improved outcomes for people with a range of physical health conditions. These include lower levels of anxiety, depression and fatigue among people with cancer, enhanced psychological stability for patients with heart disease, and improved social connection among people who have experienced a traumatic brain injury.
Art therapy has been associated with improved mood and anxiety levels for patients in hospital, and lower pain, tiredness and depression among palliative care patients.

Our research
Mental ill-health, including among children and young people, presents a major challenge for our society. While most care takes place in the community, a small proportion of young people require care in hospital to ensure their safety.
In this environment, practices that place even greater restriction, such as seclusion or physical restraint, may be used briefly as a last resort to ensure immediate physical safety. However, these “restrictive practices” are associated with negative effects such as post-traumatic stress for patients and health professionals.
Worryingly, staff report a lack of alternatives to keep patients safe. However, the elimination of restrictive practices is a major aim of mental health services in Australia and internationally.
Our research looked at more than six years of data from a child and adolescent mental health hospital ward in Australia. We sought to determine whether there was a reduction in restrictive practices during the periods when art therapy was offered on the unit, compared to times when it was absent.
We found a clear association between the provision of art therapy and reduced frequency of seclusion, physical restraint and injection of sedatives on the unit.
We don’t know the precise reason for this. However, art therapy may have lessened levels of severe distress among patients, thereby reducing the risk they would harm themselves or others, and the likelihood of staff using restrictive practices to prevent this.

That said, hospital admission involves multiple therapeutic interventions including talk-based therapies and medications. Confirming the effect of a therapeutic intervention requires controlled clinical trials where people are randomly assigned one treatment or another.
Although ours was an observational study, randomised controlled trials support the benefits of art therapy in youth mental health services. For instance, a 2011 hospital-based study showed reduced symptoms of post-traumatic stress disorder among adolescents randomised to trauma-focussed art therapy compared to a “control” arts and crafts group.

What do young people think?
In previous research we found art therapy was considered by adolescents in hospital-based mental health care to be the most helpful group therapy intervention compared to other talk-based therapy groups and creative activities.
In research not yet published, we’re speaking with young people to better understand their experiences of art therapy, and why it might reduce distress. One young person accessing art therapy in an acute mental health service shared:
[Art therapy] is a way of sort of letting out your emotions in a way that doesn’t involve being judged […] It let me release a lot of stuff that was bottling up and stuff that I couldn’t explain through words.
A promising area
The burgeoning research showing the benefits of art therapy for both physical and especially mental health highlights the value of creative and innovative approaches to treatment in health care.
There are opportunities to expand art therapy services in a range of health-care settings. Doing so would enable greater access to art therapy for people with a variety of physical and mental health conditions.
Sarah Versitano, Academic, Master of Art Therapy Program, Western Sydney University and Iain Perkes, Senior Lecturer, Child and Adolescent Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are your Kidneys Ok? Detect Early To Protect Kidney Health (Here’s How)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tomorrow (at time of publication) will be World Kidney Day (WKD). Perhaps not the most well-known initiative, but it celebrates its 21st year this year!
For those of us who celebrated our own 21st year quite some time ago now, it’s as good a reason as any to check in on our kidney health.
Here are some things they’d like us to know about Chronic Kidney Disease (CKD):
❝CKD is a silent disease, people with CKD have no signs or symptoms until the late stage of the disease.
CKD usually does not go away, instead, it progresses, unless early treatment to slow or halt the disease is ensured.
CKD can progress to kidney failure – a condition when kidneys cannot maintain their function anymore, posing a life-threatening risk.
CKD ranks number 7 in the top ten causes of death among noncommunicable diseases worldwide.
CKD increases the risk of premature death from associated cardiovascular disease.
CKD is more common among certain ethnic groups due in part to high rates of diabetes and high blood pressure.
CKD is more common among women, here is why.❞Source: World Kidney Day: Your Amazing Kidneys
How can we check our kidney health?
There are clinical tests that can be done (they’ll just need a urine sample from you; ask your doctor about it), but there’s some screening that can be done at home already:
Are Your Kidneys Healthy? Take This One-Minute Quiz To Find out
👆 this is about medical indicators; there are also non-medical factors that affect risk, including:
- Where someone lives
- Where they work
- The foods they eat
- How much exercise they do
- If they are able to get the medical care they need
For more information on this, see: Keeping Your Kidneys Healthy (Especially After 60) ← there’s a lot more to it than just hydration!
What can we do for our kidney health, besides the obvious “hydrate”?
Some top things to do include:
Hydrate, yes. See also: Things Many People Forget When It Comes To Hydration
Don’t smoke. It’s bad for everything, including your kidneys. So, just don’t. See also: Addiction Myths That Are Hard To Quit
Look after your blood. Not just “try to keep it inside your body”, but also:
- Keep your blood sugar levels healthy (hyperglycemia can cause kidney damage)
- Keep your blood pressure healthy (hypertension can cause kidney damage)
Basically, your kidneys’ primary job of filtering blood will go much more smoothly if that blood is less problematic on the way in.
Watch your over-the-counter pill intake. A lot of PRN OTC NSAIDs (PRN = pro re nata, i.e. you take them as and when symptoms arise) (NSAIDs = Non-Steroidal Anti-Inflammatory Drugs, such as ibuprofen for example) can cause kidney damage if taken regularly.
Keep an eye on your urine. Hydration is only one side of the story, and our urine can say quite a bit about our health. Indeed, we have written about this before:
12 Things Your Urine Says About Your Health (Test At Home) ← no special equipment required!
On which note, see also: To Pee Or Not To Pee ← spoiler: there’s a flood of reasons to not hold your pee
Want to know more?
Check out the WKD website’s…
8 Golden Rules Of Kidney Disease Prevention
Take care!
Share This Post
-
What Menopause Does To The Heart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
World Menopause Day: Menopause & Cardiovascular Disease Risk
Today, the 18th of October, is World Menopause Day.
The theme for this year is cardiovascular disease (CVD), and if your first reaction is to wonder what that has to do with the menopause, then this is the reason why it’s being featured. Much of the menopause and its effects are shrouded in mystery; not because of a lack of science (though sometimes a bit of that too), but rather, because it is popularly considered an unimportant, semi-taboo topic.
So, let’s be the change we want to see, and try to fix that!
What does CVD have to do with the menopause?
To quote Dr. Anjana Nair:
❝The metabolic and clinical factors secondary to menopause, such as dyslipidemia, insulin resistance, fat redistribution and systemic hypertension, contribute to the accelerated risk for cardiovascular aging and disease.
Atherosclerosis appears to be the end result of the interaction between cardiovascular risk factors and their accentuation during the perimenopausal period.
The increased cardiovascular risk in menopause stems from the exaggerated effects of changing physiology on the cardiovascular system.❞
Source: Cardiovascular Changes in Menopause
See also: Menopause-associated risk of cardiovascular disease
Can we do anything about it?
Yes, we can! Here be science:
- Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association
- Cardiovascular risk in menopausal women and our evolving understanding of menopausal hormone therapy: risks, benefits, and current guidelines for use
This (in few words: get your hormone levels checked, and consider HRT if appropriate) is consistent with the advice from gynecologist Dr. Jen Gunter, whom we featured back in August:
What You Should Have Been Told About The Menopause Beforehand
What about lifestyle changes?
We definitely can do some good things; here’s what the science has to say:
- Mediterranean diet: yes, evidence-based
- High soy consumption: mixed evidence, unclear. So, eat it if you want, don’t if you don’t.
- Supplements e.g. vitamins and minerals: yes, evidence-based.
- Supplements e.g. herbal preparations: many may help, but watch out for adverse interactions with meds. Check with your pharmacist or doctor.
- Supplements; specifically CBD: not enough evidence yet
- Exercise: yes, evidence-based—especially low-impact high-resistance training, for bone strength, as well as regular moderate-intensity exercise and/or High-Intensity Interval Training, to guard against CVD.
For a full low-down on all of these:
Revealing the evidence-based lifestyle solutions to managing your menopause symptoms
Want to know more?
You can get the International Menopause Society’s free downloadable booklet here:
Menopause & Cardiovascular Disease: What Women Need To Know
You may also like our previous main feature:
What Does “Balance Your Hormones” Even Mean?
Take care!
Share This Post
-
Butter vs Margarine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Butter vs Margarine
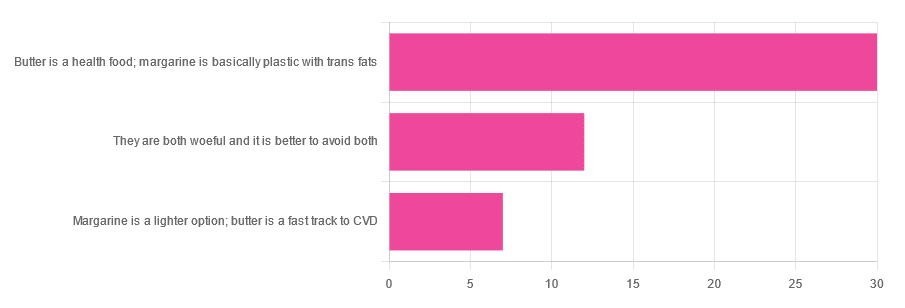
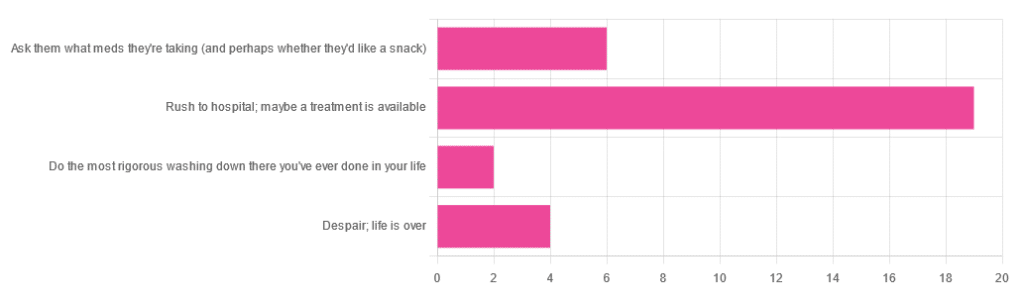
Yesterday, we asked you for your (health-related) opinion on butter vs margarine, and got the above-depicted, below-described, set of responses:
- A little over 60% said butter is a health food and margarine is basically plastic with trans fats
- A little over 20% said that both are woeful and it’s better to avoid both
- A little over 10% said that margarine is a lighter option, and butter is a fast track to cardiovascular disease.
Comments included (we will summarize/paraphrase, for space):
- “…in moderation, though”
- “I’m vegan so I use vegan butter but I know it’s not great, so I use it sparingly”
- “butter is healthy if and only if it’s grass-fed”
- “margarine has unpronounceable ingredients”
To address those quickly:
- “…in moderation” is a stipulation with which one can rarely go too far wrong
- Same! Speaking for myself (your writer here, hi) and not for the company
- Grass-fed is indeed better; alas that so little of it is grass-fed, in the US!
- Butter contains eicosatrienoic acid, linolelaidic acid, and more*. Sometimes big words don’t mean that something is worse for the health, though!
So, what does the science say?
Butter is a health food: True or False?
True or False, depending on amount! Moderation is definitely key, but we’ll return to that (and why not to have more than a small amount of butter) later. But it is a rich source of many nutrients, iff it’s grass-fed, anyway.
The nutritional profile of something isn’t a thing that’s too contentious, so rather than take too much time on it, in this case we’ll point you back up to the scientific paper we linked above, or if you prefer a pop-science rendering, here’s a nice quick rundown:
7 Reasons to Switch to Grass-Fed Butter
Margarine is basically plastic with trans fats: True or False?
False and usually False now, respectively, contingently.
On the first part: chemically, it’s simply not “basically plastic” and everything in it is digestible
On the second part: it depends on the margarine, and here’s where it pays to read labels. Historically, margarines all used to be high in trans fats (which are indeed woeful for the health). Nowadays, since trans fats have such a (well-earned) bad press, there are increasingly many margarines with low (or no) trans fats, and depending on your country, it may be that all margarines no longer have such:
❝It’s a public health success story. Consumers no longer have to worry about reading product nutritional labels to see if they contain hydrogenated oils and trans fats. They can just know that they no longer do❞
Source: Margarines now nutritionally better than butter after hydrogenated oil ban
So this is one where the science is clear (trans fats are unequivocally bad), but the consumer information is not always (it may be necessary to read labels, to know whether a margarine is conforming to the new guidelines).
Butter is a fast track to cardiovascular disease: True or False?
True or False depending on amount. In moderation, predictably it’s not a big deal.
But for example, the World Health Organization recommends that saturated fats (of which butter is a generous source) make up no more than 10% of our calorie intake:
Source: Saturated fatty acid and trans-fatty acid intake for adults and children: WHO guideline
So if you have a 2000 kcal daily intake, that would mean consuming not more than 200 kcal from butter, which is approximately two tablespoons.
If you’d like a deeper look into the complexities of saturated fats (for and against), you might like our previous main feature specifically about such:
Can Saturated Fats Be Healthy?
Enjoy!
Share This Post
Related Posts
-
What Most People Don’t Know About HIV
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What To Know About HIV This World AIDS Day
Yesterday, we asked 10almonds readers to engage in a hypothetical thought experiment with us, and putting aside for a moment any reason you might feel the scenario wouldn’t apply for you, asked:
❝You have unprotected sex with someone who, afterwards, conversationally mentions their HIV+ status. Do you…❞
…and got the above-depicted, below-described, set of responses. Of those who responded…
- Just over 60% said “rush to hospital; maybe a treatment is available”
- Just under 20% said “ask them what meds they’re taking (and perhaps whether they’d like a snack)”
- Just over 10% said “despair; life is over”
- Two people said “do the most rigorous washing down there you’ve ever done in your life”
So, what does science say about it?
First, a quick note on terms
- HIV is the Human Immunodeficiency Virus. It does what it says on the tin; it gives humans immunodeficiency. Like many viruses that have become epidemic in humans, it started off in animals (called SIV, because there was no “H” involved yet), which were then eaten by humans, passing the virus to us when it one day mutated to allow that.
- It’s technically two viruses, but that’s beyond the scope of today’s article; for our purposes they are the same. HIV-1 is more virulent and infectious than HIV-2, and is the kind more commonly found in most of the world.
- AIDS is Acquired Immunodeficiency Syndrome, and again, is what it sounds like. When a person is infected with HIV, then without treatment, they will often develop AIDS.
- Technically AIDS itself doesn’t kill people; it just renders people near-defenseless to opportunistic infections (and immune-related diseases such as cancer), since one no longer has a properly working immune system. Common causes of death in AIDS patients include cancer, influenza, pneumonia, and tuberculosis.
People who contract HIV will usually develop AIDS if untreated. Untreated life expectancy is about 11 years.
HIV/AIDS are only a problem for gay people: True or False?
False, unequivocally. Anyone can get HIV and develop AIDS.
The reason it’s more associated with gay men, aside from homophobia, is that since penetrative sex is more likely to pass it on, then if we go with the statistically most likely arrangements here:
- If a man penetrates a woman and passes on HIV, that woman will probably not go on to penetrate someone else
- If a man penetrates a man and passes on HIV, that man could go on to penetrate someone else—and so on
- This means that without any difference in safety practices or promiscuity, it’s going to spread more between men on average, by simple mathematics.
- This is why “men who have sex with men” is the generally-designated higher-risk category.
There is medication to cure HIV/AIDS: True or False?
False so far (though there have been individual case studies of gene treatments that may have cured people—time will tell).
But! There are medications that can prevent HIV from being a life-threatening problem:
- PrEP (Pre-Exposure Prophylaxis) is a medication that one can take in advance of potential exposure to HIV, to guard against it.
- This is a common choice for people aren’t sure about their partners’ statuses, or people working in risky environments.
- PEP (Post-Exposure Prophylaxis) is a medication that one can take after potential exposure to HIV, to “nip it in the bud”.
- Those of you who were rushing to hospital in our poll, this is what you’re rushing there for.
- ARVs (Anti-RetroVirals) are a class of medications (there are different options; we don’t have room to distinguish them) that reduce an HIV+ person’s viral load to undetectable levels.
- Those of you who were asking what meds your partner was taking, these will be those meds. Also, most of them are to be taken in the morning with food, so that’s what the snack was for.
If someone is HIV+, the risk of transmission in unprotected sex is high: True or False?
True or False, with false being the far more likely. It depends on their medications, and this is why you were asking. If someone is on ARVs and their viral load is undetectable (as is usual once someone has been on ARVs for 6 months), they cannot transmit HIV to you.
U=U is not a fancy new emoticon, it means “undetectable = untransmittable”, which is a mathematically true statement in the case of HIV viral loads.
See: NIH | HIV Undetectable=Untransmittable (U=U)
If you’re thinking “still sounds risky to me”, then consider this:
You are safer having unprotected sex with someone who is HIV+ and on ARVs with an undetectable viral load, than you are with someone you are merely assuming is HIV- (perhaps you assume it because “surely this polite blushing young virgin of a straight man won’t give me cooties” etc)
Note that even your monogamous partner of many decades could accidentally contract HIV due to blood contamination in a hospital or an accident at work etc, so it’s good practice to also get tested after things that involve getting stabbed with needles, cut in a risky environment, etc.
If you’re concerned about potential stigma associated with HIV testing, you can get kits online:
CDC | How do I find an HIV self-test?
(these are usually fingerprick blood tests, and you can either see the results yourself at home immediately, or send it in for analysis, depending on the kit)
If I get HIV, I will get AIDS and die: True or False?
False, assuming you get treatment promptly and keep taking it. So those of you who were at “despair; life is over” can breathe a sigh of relief now.
However, if you get HIV, it does currently mean you will have to take those meds every day for the rest of your (no reason it shouldn’t be long and happy) life.
So, HIV is definitely still something to avoid, because it’s not great to have to take a life-saving medication every day. For a little insight as to what that might be like:
HIV.gov | Taking HIV Medication Every Day: Tips & Challenges
(as you’ll see there, there are also longer-lasting injections available instead of daily pulls, but those are much less widely available)
Summary
Some quick take-away notes-in-a-nutshell:
- Getting HIV may have been a death sentence in the 1980s, but nowadays it’s been relegated to the level of “serious inconvenience”.
- Happily, it is very preventable, with PrEP, PEP, and viral loads so low that they can’t transmit HIV, thanks to ARVs.
- Washing will not help, by the way. Safe sex will, though!
- As will celibacy and/or sexual exclusivity in seroconcordant relationships, e.g. you have the same (known! That means actually tested recently! Not just assumed!) HIV status as each other.
- If you do get it, it is very manageable with ARVs, but prevention is better than treatment
- There is no certain cure—yet. Some people (small number of case studies) may have been cured already with gene therapy, but we can’t know for sure yet.
Want to know more? Check out:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How extreme heat can affect you—and how you can protect yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Because of climate change, last summer was the hottest in the Northern Hemisphere in 2,000 years—and this summer is expected to be even hotter. The record may continue to be broken: Extreme heat is expected to become even more frequent.
The scorching heat has led to an increase in heat-related deaths in the United States, according to the Department of Health and Human Services, with approximately 2,300 deaths in the summer of 2023. Extreme heat, defined as a period of two to three days with high heat and humidity with temperatures above 90 degrees Fahrenheit, can have serious health consequences, including symptoms like headache, dizziness, loss of consciousness, nausea, and confusion.
As we face more extreme heat, you may be wondering how you can protect yourself and your loved ones. Read on to learn about heat-related illness, who’s most at risk, and more.
What happens when our bodies are exposed to extreme heat?
As our body temperature rises, our bodies attempt to cool down by opening up more blood vessels near the skin to begin sweating. The evaporation of our sweat regulates our body temperature, but it also leads to losing fluids and minerals.
When it’s too humid, sweating alone doesn’t do the trick. The heart must work harder to bring blood around the body. It starts beating faster, which can cause light-headedness, nausea, and headache.
This process can affect our health in different ways, including increasing our risk of hospitalization for heart disease, worsening asthma, and injuring kidneys due to dehydration. It can also result in heat-related illness. Below are some effects of heat on our bodies:
- Heat cramps: Occur when a person loses salt through sweating, which causes painful cramps. Symptoms begin as painful spasms after heavy sweating, usually in the legs or the stomach. Heat cramps can lead to heat exhaustion or heat stroke.
- Heat exhaustion: This occurs when the body loses an excessive amount of water and salt, usually during intense physical activity. Symptoms include irritability, heavy sweating, and weakness, including muscle cramps. Heat exhaustion can lead to heat stroke.
- Heat stroke: This is the most severe heat-related illness. It happens when the body can’t cool down and reaches a temperature of 106 Fahrenheit or higher within 10 to 15 minutes. If the person doesn’t receive emergency treatment, it can cause permanent disability or death. Symptoms include confusion, loss of consciousness, and seizures.
What should I do if someone experiences a heat-related illness?
If you or someone you’re with begins to show signs of heat illness, the Centers for Disease Control and Prevention recommends the following:
- Heat cramps: Stop all physical activity, drink water or a sports drink, move to a cool place, and wait for cramps to go away before resuming activity. If the cramps last more than an hour, you’re on a low-sodium diet, or you have heart problems, get medical help.
- Heat exhaustion: Move the person to a cool place, loosen their clothes, use a cool bath or cloths to try to lower their body temperature, and give them a sip of water. If the person throws up, or if their symptoms last longer than an hour or worsen, get medical help.
- Heat stroke: Call 911 immediately. Then, move the person to a cooler place, use cool cloths or a cool bath to help lower their temperature, and don’t give them anything to drink.
Read more about heat-related illness and what to do in each case.
Who’s more vulnerable to extreme heat?
While everyone can be affected by extreme heat, some people are more at risk, including people of color.
A 2023 KFF report outlined that because of historical residential segregation in the U.S. (known as “redlining”), people of color are more likely to live in areas that experience higher temperatures from rooftops, asphalt, and sidewalks that retain the sun’s heat (known as the “urban heat island effect”). Additionally, communities of color are more likely to live in areas with fewer trees, which act as a canopy and provide shade, making the heat worse and more direct.
Children under 5, adults 65 or over, and pregnant people are also more vulnerable to extreme heat. If you have a chronic health condition like diabetes, heart problems, or a mental health condition, you’re also at higher risk. (Some psychiatric medications, like antidepressants, can also make people more susceptible to heat).
Lastly, anyone exposed to the sun and extreme heat for long periods is also at higher risk. This includes athletes, people who work outdoors, and unhoused people.
What can I do to prevent heat-related illness during a heat wave?
During a heat wave, follow these tips to stay cool and protect yourself from heat-related illness:
- Never leave your pets or children inside a car.
- Wear loose, light-colored clothing (dark colors absorb more heat).
- Find shade if you’re outside.
- If you don’t have air conditioning in your home, go to a place where you can cool down, such as a local library, community center, local pool or splash pad, or mall. Check to see if your city has designated cooling centers. (Cities like New York have a list of places.)
- Wear a hat.
- Drink (non-alcoholic) fluids often to stay hydrated—and if you have pets, give them water frequently as well.
- Check on your family members or older neighbors who may be more sensitive to extreme heat.
- Avoid using your stove or oven too often or during the hottest parts of the day.
- Cover your windows with shades to keep the heat out.
What are some resources to prevent heat-related illness?
If you need financial assistance to cool down your home, such as to purchase an air conditioner, apply to the federal government’s Low Income Home Energy Assistance Program.
Before you head outside during a heat wave, use the CDC’s HeatRisk tool: Enter your zip code to find the current heat risk in your area and get tips on what to do to stay safe with each risk level.
During a heat wave, also look for a cooling center in your state using the National Center for Healthy Housing’s list.
Check out the National Weather Service’s for more tips and resources.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ouch. That ‘Free’ Annual Checkup Might Cost You. Here’s Why.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Kristy Uddin, 49, went in for her annual mammogram in Washington state last year, she assumed she would not incur a bill because the test is one of the many preventive measures guaranteed to be free to patients under the 2010 Affordable Care Act. The ACA’s provision made medical and economic sense, encouraging Americans to use screening tools that could nip medical problems in the bud and keep patients healthy.
So when a bill for $236 arrived, Uddin — an occupational therapist familiar with the health care industry’s workings — complained to her insurer and the hospital. She even requested an independent review.
“I’m like, ‘Tell me why am I getting this bill?’” Uddin recalled in an interview. The unsatisfying explanation: The mammogram itself was covered, per the ACA’s rules, but the fee for the equipment and the facility was not.
That answer was particularly galling, she said, because, a year earlier, her “free” mammogram at the same health system had generated a bill of about $1,000 for the radiologist’s reading. Though she fought that charge (and won), this time she threw in the towel and wrote the $236 check. But then she dashed off a submission to the KFF Health News-NPR “Bill of the Month” project:
“I was really mad — it’s ridiculous,” she later recalled. “This is not how the law is supposed to work.”
The ACA’s designers might have assumed that they had spelled out with sufficient clarity that millions of Americans would no longer have to pay for certain types of preventive care, including mammograms, colonoscopies, and recommended vaccines, in addition to doctor visits to screen for disease. But the law’s authors didn’t reckon with America’s ever-creative medical billing juggernaut.
Over the past several years, the medical industry has eroded the ACA’s guarantees, finding ways to bill patients in gray zones of the law. Patients going in for preventive care, expecting that it will be fully covered by insurance, are being blindsided by bills, big and small.
The problem comes down to deciding exactly what components of a medical encounter are covered by the ACA guarantee. For example, when do conversations between doctor and patient during an annual visit for preventive services veer into the treatment sphere? What screenings are needed for a patient’s annual visit?
A healthy 30-year-old visiting a primary care provider might get a few basic blood tests, while a 50-year-old who is overweight would merit additional screening for Type 2 diabetes.
Making matters more confusing, the annual checkup itself is guaranteed to be “no cost” for women and people age 65 and older, but the guarantee doesn’t apply for men in the 18-64 age range — though many preventive services that require a medical visit (such as checks of blood pressure or cholesterol and screens for substance abuse) are covered.
No wonder what’s covered under the umbrella of prevention can look very different to medical providers (trying to be thorough) and billers (intent on squeezing more dollars out of every medical encounter) than it does to insurers (who profit from narrower definitions).
For patients, the gray zone has become a billing minefield. Here are a few more examples, gleaned from the Bill of the Month project in just the past six months:
Peter Opaskar, 46, of Texas, went to his primary care doctor last year for his preventive care visit — as he’d done before, at no cost. This time, his insurer paid $130.81 for the visit, but he also received a perplexing bill for $111.81. Opaskar learned that he had incurred the additional charge because when his doctor asked if he had any health concerns, he mentioned that he was having digestive problems but had already made an appointment with his gastroenterologist. So, the office explained, his visit was billed as both a preventive physical and a consultation. “Next year,” Opasker said in an interview, if he’s asked about health concerns, “I’ll say ‘no,’ even if I have a gunshot wound.”
Kevin Lin, a technology specialist in Virginia in his 30s, went to a new primary care provider to take advantage of the preventive care benefit when he got insurance; he had no physical complaints. He said he was assured at check-in that he wouldn’t be charged. His insurer paid $174 for the checkup, but he was billed an additional $132.29 for a “new patient visit.” He said he has made many calls to fight the bill, so far with no luck.
Finally, there’s Yoori Lee, 46, of Minnesota, herself a colorectal surgeon, who was shocked when her first screening colonoscopy yielded a bill for $450 for a biopsy of a polyp — a bill she knew was illegal. Federal regulations issued in 2022 to clarify the matter are very clear that biopsies during screening colonoscopies are included in the no-cost promise. “I mean, the whole point of screening is to find things,” she said, stating, perhaps, the obvious.
Though these patient bills defy common sense, room for creative exploitation has been provided by the complex regulatory language surrounding the ACA. Consider this from Ellen Montz, deputy administrator and director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare & Medicaid Services, in an emailed response to queries and an interview request on this subject: “If a preventive service is not billed separately or is not tracked as individual encounter data separately from an office visit and the primary purpose of the office visit is not the delivery of the preventive item or service, then the plan issuer may impose cost sharing for the office visit.”
So, if the doctor decides that a patient’s mention of stomach pain does not fall under the umbrella of preventive care, then that aspect of the visit can be billed separately, and the patient must pay?
And then there’s this, also from Montz: “Whether a facility fee is permitted to be charged to a consumer would depend on whether the facility usage is an integral part of performing the mammogram or an integral part of any other preventive service that is required to be covered without cost sharing under federal law.”
But wait, how can you do a mammogram or colonoscopy without a facility?
Unfortunately, there is no federal enforcement mechanism to catch individual billing abuses. And agencies’ remedies are weak — simply directing insurers to reprocess claims or notifying patients they can resubmit them.
In the absence of stronger enforcement or remedies, CMS could likely curtail these practices and give patients the tools to fight back by offering the sort of clarity the agency provided a few years ago regarding polyp biopsies — spelling out more clearly what comes under the rubric of preventive care, what can be billed, and what cannot.
The stories KFF Health News and NPR receive are likely just the tip of an iceberg. And while each bill might be relatively small compared with the stunning $10,000 hospital bills that have become all too familiar in the United States, the sorry consequences are manifold. Patients pay bills they do not owe, depriving them of cash they could use elsewhere. If they can’t pay, those bills might end up with debt-collection agencies and, ultimately, harm their credit score.
Perhaps most disturbing: These unexpected bills might discourage people from seeking preventive screenings that could be lifesaving, which is why the ACA deemed them “essential health benefits” that should be free.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: