Prostate Health: What You Should Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Prostate Health: What You Should Know
We’re aware that very many of our readers are women, who do not have a prostate.
However, dear reader: if you do have one, and/or love someone who has one, this is a good thing to know about.
The prostate gland is a (hopefully) walnut-sized gland (it actually looks a bit like a walnut too), that usually sits just under the bladder.
See also: How to Locate Your Prostate*
*The scale is not great in these diagrams, but they’ll get the job done. Besides, everyone is different on the inside, anyway. Not in a “special unique snowflake” way, but in a “you’d be surprised how much people’s insides move around” way.
Fun fact: did you ever feel like your intestines are squirming? That’s because they are.
You can’t feel it most of the time due to the paucity of that kind of nervous sensation down there, but the peristaltic motion that they use to move food along them on the inside, also causes them push against the rest of your guts, on the outside of them. This is the exact same way that many snakes move about.
If someone has to perform an operation in that region, sometimes it will be necessary to hang the intestines on a special rack, to keep them in one place for the surgery.
What can go wrong?
There are two very common things that can go wrong with the prostate:
- Benign Prostate Hyperplasia (BPH), otherwise known as an enlarged prostate
- Prostate cancer
For most men, the prostate gland continues to grow with age, which is how the former comes about so frequently.
For everyone, due to the nature of the mathematics involved in cellular mutation and replication, we will eventually get cancer if something else doesn’t kill us first.
- Prostate cancer affects 12% of men overall, and 60% of men aged 60+, with that percentage climbing each year thereafter.
- Prostate cancer can look like BPH in the early stages (and/or, an enlarged prostate can turn cancerous) so it’s important to not shrug off the symptoms of BPH.
How can BPH be avoided/managed?
There are prescription medications that can help reduce the size of the prostate, including testosterone blockers (such as spironolactone and bicalutamide) and 5α-reductase inhibitors, such as finasteride. Each have their pros and cons:
- Testosterone-blockers are the heavy-hitters, and work very well… but have more potential adverse side effects (your body is used to running on testosterone, after all)
- 5α-reductase inhibitors aren’t as powerful, but they block the conversion of free testosterone to dihydrogen testosterone (DHT), and it’s primarily DHT that causes the problems. By blocking the conversion of T to DHT, you may actually end up with higher serum testosterone levels, but fewer ill-effects. Exact results will vary depending on your personal physiology, and what else you are taking, though.
There are also supplements that can help, including saw palmetto and pumpkin seed oil. Here’s a good paper that covers both:
We have recommended saw palmetto before for a variety of uses, including against BPH:
Too much or too little testosterone? This one supplement may fix that
You might want to avoid certain medications that can worsen BPH symptoms (but not actually the size of the prostate itself). They include:
- Antihistamines
- Decongestants
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Tricyclic antidepressants (most modern antidepressants aren’t this kind; ask your pharmacist/doctor if unsure)
You also might want to reduce/skip:
- Alcohol
- Caffeine
In all the above cases, it’s because of how they affect the bladder, not the prostate, but given their neighborliness, each thing affects the other.
What if it’s cancer? How do I know and what do I do?
The creator of the Prostate Specific Antigen (PSA) test has since decried it as “a profit-driven health disaster” that is “no better than a coin toss”, but it remains the first go-to of many medical services.
However, there’s a newer, much more accurate test, called the Prostate Screening Episwitch (PSE) test, which is 94% accurate, so you might consider asking your healthcare provider whether that’s an option:
The new prostate cancer blood test with 94 per cent accuracy
As for where to go from there, we’re out of space for today, but we previously reviewed a very good book about this, Dr. Patrick Walsh’s Guide to Surviving Prostate Cancer, and we highly recommend it—it could easily be a literal lifesaver.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Break the Cycle – by Dr. Mariel Buqué
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Intergenerational trauma comes in two main varieties: epigenetic, and behavioral.
This book covers both. There’s a lot more we can do about the behavioral side than the epigenetic, but that’s not to say that Dr. Buqué doesn’t have useful input in the latter kind too.
If you’ve read other books on epigenetic trauma, then there’s nothing new here—though the refresher is always welcome.
On the behavioral side, Dr. Buqué gives a strong focus on practical techniques, such as specific methods of journaling to isolate trauma-generated beliefs and resultant behaviors, with a view to creating one’s own trauma-informed care, cutting through the cycle, and stopping it there.
Which, of course, will not only be better for you, but also for anyone who will be affected by how you are (e.g. now/soon, hopefully better).
As a bonus, if you see the mistakes your parents made and are pretty sure you didn’t pass them on, this book can help you troubleshoot for things you missed, and also to improve your relationship with your own childhood.
Bottom line: if you lament how things were, and do wish/hope to do better in terms of mental health for yourself now and generations down the line, this book is a great starting point.
Share This Post
-
What Happens To Your Body When You Plank 1 Minute Every Day
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Planks improve strength, flexibility, balance, posture, reduce chronic back pain, lower blood pressure, and enhance physique. But can we really get benefits from just 1 minute per day?
To the core
The benefits that can be expected, according to the science cited in this video, include:
- Within 2–3 weeks, daily planking of just 1 minute per day activates deep core muscles, enhancing balance, which helps in everyday tasks and prevents muscle imbalances.
- Strengthening core muscles through planks also helps alleviate lower back pain, with research supporting its effectiveness within 3 weeks.
- Posture is important for good health, and planks align the spine and hips, improving posture naturally, which also helps alleviate back issues. So, there’s a good kind of synergy to this exercise.
- Of course, many people exercising have the goal of a more toned body; regular planking leads to a toned core, sculpted shoulders, and leaner legs.
- For those who care more about mobility, though, planking enhances flexibility in hamstrings, feet, and toes within 4–6 weeks.
- Anything else? Yes, isometric exercises like planks are highly effective at reducing blood pressure, and, counterintuitively, more so than aerobic exercises.
The video also looks at a study in which participants did 20 minutes per day instead of 1, which predictably also significantly improved strength, endurance, flexibility, and reduced body fat.
However, another study cited gives the stats for just 1 minute daily, and that was not even a whole minute, so much as 30 seconds hold, 1 minute rest, 30 seconds hold—and still showed very good improvements.
For more on all this, plus links to three studies mentioned in the video, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Isometric Exercises That Are Good If You Have Osteoporosis (or if you don’t, but the point is, they are safe and beneficial for people with osteoporosis)
Take care!
Share This Post
-
Apricot vs Banana – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apricot to banana, we picked the banana.
Why?
Both are great, and it was close!
In terms of macros, apricot has more protein, while banana has more carbs and fiber; both are low glycemic index foods, and we’ll call this category a tie.
In the category of vitamins, apricot has more of vitamins A, C, E, and K, while banana has more of vitamins B1, B2, B3, B5, B6, B7, B9, and choline, giving banana the win by strength of numbers. It’s worth noting though that apricots are one of the best fruits for vitamin A in particular.
When it comes to minerals, apricot has slightly more calcium, iron, and zinc, while banana has a lot more magnesium, manganese, potassium, and selenium, meaning a moderate win for banana here.
Adding up the sections makes for an overall win for banana—but of course, by all means enjoy either or both!
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← we argue for apricots as bonus number 9 on the list
Take care!
Share This Post
Related Posts
-
Carbonated Water: For Weight Loss, Satiety, Or Just Gas?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are two main mechanisms of action by which sparkling water is considered to help satiety and/or weight loss; they are:
- It “fills us up” such that we feel fuller sooner, and thus eat less, and thus (all other things being equal) perhaps lose weight
- The carbon dioxide is absorbed into the bloodstream, where (as a matter of chemistry) it improves glucose metabolism, thus lowering blood sugars and indirectly leading (potentially) to weight loss, but even if not, lowered blood sugars are good for most people most of the time, right?
However, there are just a few problems:
Full of gas?
Many people self-report enjoying sparkling water as a way to feel fuller while fasting (or even while eating). However, the plural of “anecdote” is not “data”, so, here be data… Ish:
❝In order to determine whether such satiating effects occur through oral carbonic stimulation alone, we conducted modified sham-feeding (SF) tests (carbonated water ingestion (CW), water ingestion (W), carbonated water sham-feeding (CW-SF), and water sham-feeding (W-SF)), employing an equivalent volume and standardized temperature of carbonated and plain water, in a randomized crossover design.
Thirteen young women began fasting at 10 p.m. on the previous night and were loaded with each sample (15ºC, 250 mL) at 9 a.m. on separate days. Electrogastrography (EGG) recordings were obtained from 20 min before to 45 min after the loading to determine the power and frequency of the gastric myoelectrical activity. Appetite was assessed using visual analog scales. After ingestion, significantly increased fullness and decreased hunger ratings were observed in the CW group. After the load, transiently but significantly increased fullness as well as decreased hunger ratings were observed in the CW-SF group. The powers of normogastria (2-4 cpm) and tachygastria (4-9 cpm) showed significant increases in the CW and W groups, but not in the CW-SF and W-SF groups. The peak frequency of normogastria tended to shift toward a higher band in the CW group, whereas it shifted toward a lower band in the CW-SF group, indicating a different EGG rhythm.
Our results suggest that CO2-induced oral stimulation is solely responsible for the feeling of satiety.❞
~ Dr. Maki Suzuki et al.
Now, that’s self-reported, and a sample size of 13, so it’s not the most airtight science ever, but it is at least science. Here’s the paper, by the way:
Oral Carbonation Attenuates Feeling of Hunger and Gastric Myoelectrical Activity in Young Women
Here’s another small study with 8 people, which found that still and sparkling water had the exact same effect:
Effect of carbonated water on gastric emptying and intragastric meal distribution
However, drinking water (still or sparkling) with a meal will not have anywhere near the same effect for satiety as consuming food that has a high water-content.
See also: Some Surprising Truths About Hunger And Satiety ← our main feature in which we examine the science of volumetrics, including a study that shows how water incorporated into a food (but not served with a food) decreases caloric intake.
As an aside, one difference that carbonation can make is to increase ghrelin levels—that’s the hunger hormone (the satiety hormone is leptin, by the way). This one’s a rat study, but it seems reasonable that the same will be true of humans:
…which is worth bearing in mind even if you yourself are not, in fact, a male rat.
The glucose guzzler?
This one has simply been the case of a study being misrepresented, for example here:
Fizzy water might aid weight loss by providing a small boost to glucose uptake and metabolism
The idea is that higher levels of carbon dioxide in the blood mean faster glucose metabolism, which is technically true. Now, often “technically true” is the best kind of true, but not here, because it’s simply not useful.
In short, we produce so much carbon dioxide as part of our normal respiratory processes, that any carbon dioxide we might consume in a carbonated water is barely a blip in the graph.
Oh, and that article we just linked? Even within the article, despite running with that headline, the actual scientists quoted are saying such things as:
❝While there is a hypothetical link between carbonated water and glucose metabolism, this has yet to be tested in well-designed human intervention studies❞
~ Professor Sumantra Ray
Note: the word “hypothetical” means “one level lower than theoretical”. This is very far from being a conclusion.
And the study itself? Wasn’t even about carbonated water, it was about kidney dialysis and how the carbon dioxide content can result in hypoglycemia:
The mechanism of hypoglycemia caused by hemodialysis
…which got referenced in this paper (not a study):
Can carbonated water support weight loss?
…and even that concluded:
❝CO2 in carbonated water may promote weight loss by enhancing glucose uptake and metabolism in red blood cells.
However, the amount is so small that it is difficult to expect weight loss effects solely from the CO2 in carbonated water.
Drinking carbonated water may also affect blood glucose measurements.❞
Note: the word “may”, when used by a scientist and in the absence of any stronger claims, means “we haven’t ruled out the possibility”.
What breaking news that is.
Stop the press! No, really, stop it!
So… What does work?
There are various ways of going about actually hacking hunger (and they stack; i.e. you can use multiple methods and get cumulative results), and we wrote about them here:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Should You Go Light Or Heavy On Carbs?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Carb-Strong or Carb-Wrong?
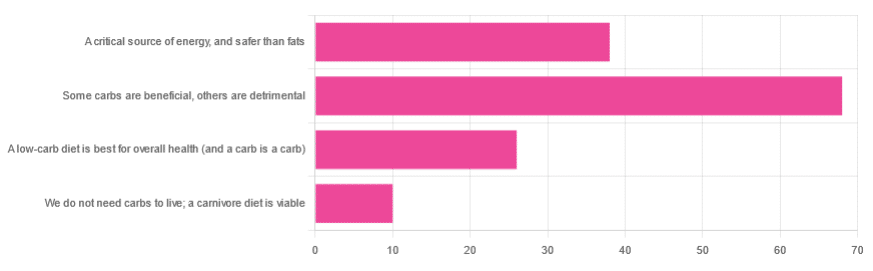
We asked you for your health-related view of carbs, and got the above-depicted, below-described, set of responses
- About 48% said “Some carbs are beneficial; others are detrimental”
- About 27% said “Carbs are a critical source of energy, and safer than fats”
- About 18% said “A low-carb diet is best for overall health (and a carb is a carb)”
- About 7% said “We do not need carbs to live; a carnivore diet is viable”
But what does the science say?
Carbs are a critical source of energy, and safer than fats: True or False?
True and False, respectively! That is: they are a critical source of energy, and carbs and fats both have an important place in our diet.
❝Diets that focus too heavily on a single macronutrient, whether extreme protein, carbohydrate, or fat intake, may adversely impact health.❞
Source: Low carb or high carb? Everything in moderation … until further notice
(the aforementioned lead author Dr. de Souza, by the way, served as an external advisor to the World Health Organization’s Nutrition Guidelines Advisory Committee)
Some carbs are beneficial; others are detrimental: True or False?
True! Glycemic index is important here. There’s a big difference between eating a raw carrot and drinking high-fructose corn syrup:
Which Sugars Are Healthier, And Which Are Just The Same?
While some say grains and/or starchy vegetables are bad, best current science recommends:
- Eat some whole grains regularly, but they should not be the main bulk of your meal (non-wheat grains are generally better)
- Starchy vegetables are not a critical food group, but in moderation they are fine.
To this end, the Mediterranean Diet is the current gold standard of healthful eating, per general scientific consensus:
A low-carb diet is best for overall health (and a carb is a carb): True or False?
True-ish and False, respectively. We covered the “a carb is a carb” falsehood earlier, so we’ll look at “a low-carb diet is best”.
Simply put: it can be. One of the biggest problems facing the low-carb diet though is that adherence tends to be poor—that is to say, people crave their carby comfort foods and eat more carbs again. As for the efficacy of a low-carb diet in the context of goals such as weight loss and glycemic control, the evidence is mixed:
❝There is probably little to no difference in weight reduction and changes in cardiovascular risk factors up to two years’ follow-up, when overweight and obese participants without and with T2DM are randomised to either low-carbohydrate or balanced-carbohydrate weight-reducing diets❞
Source: Low-carbohydrate versus balanced-carbohydrate diets for reducing weight and cardiovascular risk
❝On the basis of moderate to low certainty evidence, patients adhering to an LCD for six months may experience remission of diabetes without adverse consequences.
Limitations include continued debate around what constitutes remission of diabetes, as well as the efficacy, safety, and dietary satisfaction of longer term LCDs❞
~ Dr. Joshua Goldenberg et al.
Source: Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission
❝There should be no “one-size-fits-all” eating pattern for different patient´s profiles with diabetes.
It is clinically complex to suggest an ideal percentage of calories from carbohydrates, protein and lipids recommended for all patients with diabetes.❞
Source: Current Evidence Regarding Low-carb Diets for The Metabolic Control of Type-2 Diabetes
We do not need carbs to live; a carnivore diet is viable: True or False?
False. For a simple explanation:
The Carnivore Diet: Can You Have Too Much Meat?
There isn’t a lot of science studying the effects of consuming no plant products, largely because such a study, if anything other than observational population studies, would be unethical. Observational population studies, meanwhile, are not practical because there are so few people who try this, and those who do, do not persist after their first few hospitalizations.
Putting aside the “Carnivore Diet” as a dangerous unscientific fad, if you are inclined to meat-eating, there is some merit to the Paleo Diet, at least for short-term weight loss even if not necessarily long-term health:
What’s The Real Deal With The Paleo Diet?
For longer-term health, we refer you back up to the aforementioned Mediterranean Diet.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting Your Messy Life In Order
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Getting Your Messy Life In Order
We’ve touched on this before by recommending the book, but today we’re going to give an overview of the absolute most core essentials of the “Getting Things Done” method. If you’re unfamiliar, this will be enough to get you going. If you’re already familiar, this may be a handy reminder!
First, you’ll need:
- A big table
- A block of small memo paper squares—post-it note sized, but no need to be sticky.
- A block of A4 printer paper
- A big trash bag
Gathering everything
Gather up not just all your to-dos, but: all sources of to-dos, too, and anything else that otherwise needs “sorting”.
Put them all in one physical place—a dining room table may have enough room. You’ll need a lot of room because you’re going to empty our drawers of papers, unopened (or opened and set aside) mail. Little notes you made for yourself, things stuck on the fridge or memo boards. Think across all areas of your life, and anything you’re “supposed” to do, write it down on a piece of paper. No matter what area of your life, no matter how big or small.
Whether it’s “learn Chinese” or “take the trash out”, write it down, one item per piece of paper (hence the block of little memo squares).
Sorting everything
Everything you’ve gathered needs one of three things to happen:
- You need to take some action (put it in a “to do” pile)
- You may need it later sometime (put it in a “to file” pile)
- You don’t need it (put it in the big trash bag for disposal)
What happens next will soothe you
- Dispose of the things you put for disposal
- File the things for filing in a single alphabetical filing system. If you don’t have one, you’ll need to get one, so write that down and add it to the “to do” pile.
- You will now process your “to dos”
Processing the “to dos”
The pile you have left is now your “inbox”. It’s probably huge; later it’ll be smaller, maybe just a letter-tray on your desk.
Many of your “to dos” are actually not single action items, they’re projects. If something requires more than one step, it’s a project.
Take each item one-by-one. Do this in any order; you’re going to do this as quickly as possible! Now, ask yourself: is this a single-action item that I could do next, without having to do something else first?
- If yes: put it in a pile marked “next action”
- If no: put it in a pile marked “projects”.
Take a sheet of A4 paper and fold it in half. Write “Next Action” on it, and put your pile of next actions inside it.
Take a sheet of A4 paper per project and write the name of the project on it, for example “Learn Chinese”, or “Do taxes”. Put any actions relating to that project inside it.
Likely you don’t know yet what the first action will be, or else it’d be in your “Next Action” pile, so add an item to each project that says “Brainstorm project”.
Processing the “Next Action” pile
Again you want to do this as quickly as possible, in any order.
For each item, ask yourself “Do I care about this?” If the answer is no, ditch that item, and throw it out. That’s ok. Things change and maybe we no longer want or need to do something. No point in hanging onto it.
For each remaining item, ask yourself “can this be done in under 2 minutes?”.
- If yes, do it, now. Throw away the piece of paper for it when you’re done.
- If no, ask yourself:”could I usefully delegate this to someone else?” If the answer is yes, do so.
If you can’t delegate it, ask yourself: “When will be a good time to do this?” and schedule time for it. A specific, written-down, clock time on a specific calendar date. Input that into whatever you use for scheduling things. If you don’t already use something, just use the calendar app on whatever device you use most.
The mnemonic for the above process is “Do/Defer/Delegate/Ditch”
Processing projects:
If you don’t know where to start with a project, then figuring out where to start is your “Next Action” for that project. Brainstorm it, write down everything you’ll need to do, and anything that needs doing first.
The end result of this is:
- You will always, at any given time, have a complete (and accessible) view of everything you are “supposed” to do.
- You will always, at any given time, know what action you need to take next for a given project.
- You will always, when you designate “work time”, be able to get straight into a very efficient process of getting through your to-dos.
Keeping on top of things
- Whenever stuff “to do something with/about” comes to you, put it in your physical “inbox” place—as mentioned, a letter-tray on a desk should suffice.
- At the start of each working day, quickly process things as described above. This should be a small daily task.
- Once a week, do a weekly review to make sure you didn’t lose sight of something.
- Monthly, quarterly, and annual reviews can be a good practice too.
How to do those reviews? Topic for another day, perhaps.
Or:
Check out the website / Check out GTD apps / Check out the book
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: