Hearing voices is common and can be distressing. Virtual reality might help us meet and ‘treat’ them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever heard something that others cannot – such as your name being called? Hearing voices or other noises that aren’t there is very common. About 10% of people report experiencing auditory hallucinations at some point in their life.
The experience of hearing voices can be very different from person to person, and can change over time. They might be the voice of someone familiar or unknown. There might be many voices, or just one or two. They can be loud or quiet like a whisper.
For some people these experiences are positive. They might represent a spiritual or supernatural experience they welcome or a comforting presence. But for others these experiences are distressing. Voices can be intrusive, negative, critical or threatening. Difficult voices can make a person feel worried, frightened, embarrassed or frustrated. They can also make it hard to concentrate, be around other people and get in the way of day-to-day activities.
Although not everyone who hears voices has a mental health problem, these experiences are much more common in people who do. They have been considered a hallmark symptom of schizophrenia, which affects about 24 million people worldwide.
However, such experiences are also common in other mental health problems, particularly in mood- and trauma-related disorders (such as bipolar disorder or depression and post-traumatic stress disorder) where as many as half of people may experience them.

Why do people hear voices?
It is unclear exactly why people hear voices but exposure to prolonged stress, trauma or depression can increase the chances.
Some research suggests people who hear voices might have brains that are “wired” differently, particularly between the hearing and speaking parts of the brain. This may mean parts of our inner speech can be experienced as external voices. So, having the thought “you are useless” when something goes wrong might be experienced as an external person speaking the words.
Other research suggests it may relate to how our brains use past experiences as a template to make sense of and make predictions about the world. Sometimes those templates can be so strong they lead to errors in how we experience what is going on around us, including hearing things our brain is “expecting” rather than what is really happening.
What is clear is that when people tell us they are hearing voices, they really are! Their brain perceives voice experiences as if someone were talking in the room. We could think of this “mistake” as working a bit like being susceptible to common optical tricks or visual illusions.

Coping with hearing voices
When hearing voices is getting in the way of life, treatment guidelines recommend the use of medications. But roughly a third of people will experience ongoing distress. As such, treatment guidelines also recommend the use of psychological therapies such as cognitive behavioural therapy.
The next generation of psychological therapies are beginning to use digital technologies and virtual reality offers a promising new medium.
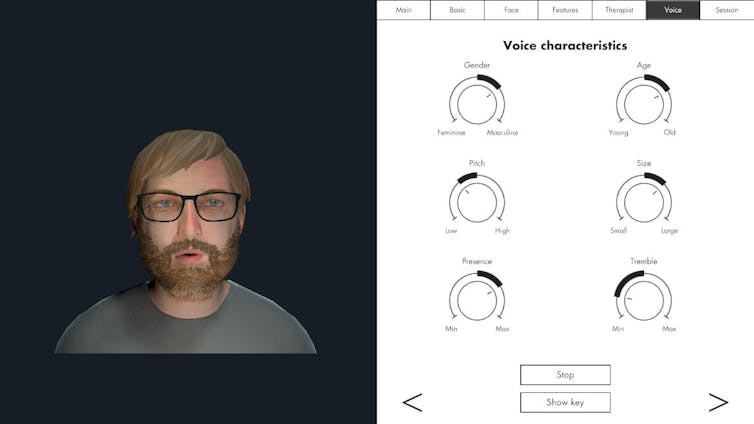
Avatar therapy allows a person to create a virtual representation of the voice or voices, which looks and sounds like what they are experiencing. This can help people regain power in the “relationship” as they interact with the voice character, supported by a therapist.
Jason’s experience
Aged 53, Jason (not his real name) had struggled with persistent voices since his early 20s. Antipsychotic medication had helped him to some extent over the years, but he was still living with distressing voices. Jason tried out avatar therapy as part of a research trial.
He was initially unable to stand up to the voices, but he slowly gained confidence and tested out different ways of responding to the avatar and voices with his therapist’s support.
Jason became more able to set boundaries, such as not listening to them for periods throughout the day. He also felt more able to challenge what they said and make his own choices.
Over a couple of months, Jason started to experience some breaks from the voices each day and his relationship with them started to change. They were no longer like bullies, but more like critical friends pointing out things he could consider or be aware of.
Gaining recognition
Following promising results overseas and its recommendation by the United Kingdom’s National Institute for Health and Care Excellence, our team has begun adapting the therapy for an Australian context.
We are trialling delivering avatar therapy from our specialist voices clinic via telehealth. We are also testing whether avatar therapy is more effective than the current standard therapy for hearing voices, based on cognitive behavioural therapy.
As only a minority of people with psychosis receive specialist psychological therapy for hearing voices, we hope our trial will support scaling up these new treatments to be available more routinely across the country.
We would like to acknowledge the advice and input of Dr Nadine Keen (consultant clinical psychologist at South London and Maudsley NHS Foundation Trust, UK) on this article.
Leila Jameel, Trial Co-ordinator and Research Therapist, Swinburne University of Technology; Imogen Bell, Senior Research Fellow and Psychologist, The University of Melbourne; Neil Thomas, Professor of Clinical Psychology, Swinburne University of Technology, and Rachel Brand, Senior Lecturer in Clinical Psychology, University of the Sunshine Coast
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Feeding You Lies – by Vani Hari
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to advertising, we know that companies will often be as misleading as they can get away with. But just how misleading is it?
Vani Hari, of “Food Babe” fame, is here to unravel it all.
The book covers many areas of food and drink advertising and marketing, and gives particular attention to:
- Sodas (with and without sugar), and how deleterious they are to the health—as well as not even helping people lose weight, but actively hindering
- Nutritionally fortified foods, and what we may or may not actually get from them by the time the processing is done
- Organic food, and what that may or may not mean
She also covers a lot of what happens outside of supermarkets, way back in universities and corporate boardrooms. In short, who is crossing whose palms with silver for a seal of approval… And what that means for us as consumers.
A strength of this book that sets it apart from many of its genre, by the way, is that while being deeply critical of certain institutions’ practices, it doesn‘t digress into tinfoil-hat pseudoscientific scaremongering, either. Here at 10almonds we love actual science, so that was good to see too.
Bottom line: is you’d like to know “can they say that and get away with it if it’s not true?” and make decisions based on the actual nutritional value of things, this is a great book for you.
Click here to check out “Feeding You Lies” on Amazon and make your shopping healthier!
Share This Post
-
The Immunostimulant Superfood –
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is not: a “detox cleanse” book of the kind that claims you can flush out the autism if you just eat enough celery.
What it rather is: an overview brain chemistry, gut microbiota, and the very many other bodily systems that interact with these “two brains”.
She also does some mythbusting of popular misconceptions (for example with regard to tryptophan), and explains with good science just what exactly such substances as gluten and casein can and can’t do.
The format is less of a textbook and more a multipart (i.e., chapter-by-chapter) lecture, in pop-science style though, making it very readable. There are a lot of practical advices too, and options to look up foods by effect, and what to eat for/against assorted mental states.
Bottom line: anyone who eats food is, effectively, drugging themselves in one fashion or another—so you might as well make a conscious choice about how to do so.
Click here to check out This Is Your Brain On Food, and choose what kind of day you have!
Share This Post
-
The Borderline Personality Disorder Workbook – by Dr. Daniel Fox
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Personality disorders in general get a bad rep. In part, because their names and descriptions often focus on how the disorders affect other people, rather than how they affect the actual sufferer:
- “This disorder gives you cripplingly low self-esteem; we call it Evil Not-Quite-Human Disorder”
- “This disorder makes you feel unloveable; we call it Abusive Bitch Disorder”
- …etc
Putting aside the labels and stigma, it turns out that humans sometimes benefit from help. In the case of BPD, characterized by such things as difficult moods and self-sabotage, the advice in this book can help anyone struggling with those (and related) issues.
The style of the book is both textbook, and course. It’s useful to proceed through it methodically, and doing the exercises is good too. We recommend getting the print edition, not the Kindle edition, so that you can check off boxes, write in it (pencil, if you like!), etc.
Bottom line: if you or a loved one suffers from BPD symptoms (whether or not you/they would meet criteria for diagnosis), this book can help a lot.
Click here to check out the BPD Workbook, and retake control of your life!
Share This Post
Related Posts
-
Eat To Avoid (Or Beat) PCOS
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Polycystic ovary syndrome, PCOS, affects very many people; around 1 in 5 women. It can show up unexpectedly, and usually the first-identified sign is irregular vaginal bleeding. We say “vaginal” rather than “menstrual” as it’s not technically menses, although it’ll look (and can feel) the same.
Like many “affects mostly women” conditions, science’s general position is “we don’t know what causes it or how to cure it”.
Quick book recommendation before we continue:
Unwell Women: Misdiagnosis and Myth in a Man-Made World – by Dr. Elinor Cleghorn
…is a top-tier book about medical misogyny. We’d say more here, but well, you can read our review there 🙂
What doesn’t work
Since PCOS is characterized by excessive androgen production, it is reasonable to expect that foods containing phytoestrogens (such as soy) may help. They won’t. The human body can’t use those as estrogen, and in fact, consuming unusually large quantities of phytoestrogens can actually get in the way of your own (or bioidentical) estrogen, by competing for the same receptors but not really doing the job.
But, you won’t get that problem from moderate consumption of soy; the warning is more for those tempted to self-medicate with megadoses, or are opting for dubious supplements such as Pueraria mirifica ← will have to do a research review on that one of these days, but suffice it to say meanwhile, it has some serious drawbacks
See also: What Does “Balance Your Hormones” Even Mean?
What can work
There are some supplement-based approaches that actually can help, and those are the ones that rather than trying to manufacture estrogen out of thin air, work to reduce testosterone and/or reduce the conversion of free testosterone to its more potent form, dihydrogen testosterone (DHT); here are two examples:
- Licorice, Digestion, & Hormones
- One Man’s Saw Palmetto Is Another Woman’s Serenoa Repens ← this one has the most evidence of the two
What will work
…or at least, barring additional confounding factors, what the evidence strongly supports working. Here’s where we get into diet properly, and there are three main dietary approaches:
Low-GI diet: focus on high-fiber, low-carb foods (e.g. whole grains, legumes, berries, leafy greens). Eating this way results in improved insulin sensitivity, lower fasting insulin, cholesterol, triglycerides, waist circumference, and (for women) yes, lower testosterone levels.
See: What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
High antioxidant diet: focus on foods rich in antioxidants (e.g. vitamin A, α-tocopherol specifically, vitamins C and D, and polyphenols) as these lower PCOS incidence.
See: 21 Most Beneficial Polyphenols & What Foods Have Them
Ketogenic diet: focus on high-fat, very low-carb foods (e.g. fatty fish, dairy, leafy greens). This significantly reduces androgen levels, improves insulin sensitivity, and regulates hormones. But… It’s recommended for short-term use only due to its negative health impacts from poor (i.e. narrow) nutritional coverage:
See: Ketogenic Diet: Burning Fat, Or Burning Out?
It is also reasonable to supplement, for example:
❝Omega-3 fatty acids and vitamin D have powerful anti-inflammatory and antioxidant properties that significantly improve insulin sensitivity and reduce androgen levels in metabolic syndromes like PCOS. A higher intake of omega-3 and vitamin E also alleviates mental health parameters and gene expression of PPAR-γ, IL-8, and TNF-α in women with PCOS.
Dietary supplements, such as antioxidants like N-acetylcysteine (NAC), vitamin D, inositol, and omega-3 fatty acids, and mineral supplements (zinc, magnesium selenium, and chromium) help in reducing insulin resistance. These supplements also enhance ovulatory function and decrease inflammation in PCOS patients.
Omega-3 fatty acid supplements improve biochemical parameters LH, LH/FSH, lipid profiles, and adiponectin levels and regularize the menstrual cycle in women with PCOS. A recent RCT also indicated that probiotic/symbiotic supplementation significantly improves triglyceride, insulin, and HDL levels in women with PCOS.❞
Source: The Role of Lifestyle Interventions in PCOS Management: A Systematic Review
Want to know more?
You might like this book that we reviewed a little while back:
PCOS Repair Protocol – by Tamika Woods
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tips For Avoiding/Managing Rheumatoid Arthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding/Managing Rheumatoid Arthritis
Arthritis is the umbrella term for a cluster of joint diseases involving inflammation of the joints, hence “arthr-” (joint) “-itis” (suffix used to denote inflammation). These are mostly, but not all, autoimmune diseases, in which the body’s immune system mistakenly attacks our own joints.
Inflammatory vs Non-Inflammatory Arthritis
Arthritis is broadly divided into inflammatory arthritis and non-inflammatory arthritis.
You may be wondering: how does one get non-inflammatory inflammation of the joints?
The answer is, in “non-inflammatory” arthritis, such as osteoarthritis, the damage comes first (by general wear-and-tear) and inflammation generally follows as part of the symptoms, rather than the cause. So the name can be a little confusing. In the case of osteo- and other “non-inflammatory” forms of arthritis, you definitely still want to keep your inflammation at bay as best you can, but it’s not as absolutely critical a deal as it is for “inflammatory” forms of arthritis.
We’ll tackle the beast that is osteoarthritis another day, however.
Today we’re going to focus on…
Rheumatoid Arthritis
This is the most common of the autoimmune forms of arthritis. Some quick facts:
- It affects a little under 1% of the global population, but the older we get, the more likely it becomes
- Early onset of rheumatoid arthritis is most likely to show up around the age of 50 (but it can show up at any age)
- However, incidence (not onset) of rheumatoid arthritis peaks in the 70s age bracket
- It is 2–4 times more common in women than in men
- Approximately one third of people stop work within two years of its onset, and this increases thereafter.
Well, that sounds gloomy.
Indeed it’s not fun. There’s a lot of stiffness and aching of joints (often with swelling too), loss of joint function can be common, and then there are knock-on effects like fatigue, weakness, and loss of appetite.
Beyond that it’s an autoimmune disorder, its cause is not known, and there is no known cure.
Is there any good news?
If you don’t have rheumatoid arthritis at the present time, you can reduce your risk factors in several ways:
- Having an anti-inflammatory diet. Get plenty of fiber, greens, and berries. Fatty fish is great too, as are oily nuts. On the other side of things, high consumption of salt, sugar, alcohol, and red meat are associated with a greater risk of developing rheumatoid arthritis.
- Not smoking. Smoking is bad for pretty much everything, including your chances of developing rheumatoid arthritis.
- Not being obese. This one may be more a matter of correlation than causation, because of the dietary factors (if one eats an anti-inflammatory diet, obesity is less likely), but the association is there.
There are other risk factors that are harder to control, such as genetics, age, sex, and having a mother who smoked.
See: Genetic and environmental risk factors for rheumatoid arthritis
What if I already have rheumatoid arthritis?
If you already have rheumatoid arthritis, it becomes a matter of symptom management.
First, reduce inflammation any (reasonable) way you can. We did a main feature on this before, so we’ll just drop that again here:
Next, consider the available medications. Your doctor may or may not have discussed all of the options with you, so be aware that there are more things available than just pain relief. To talk about them all would require a whole main feature, so instead, here’s a really well-compiled list, along with explanations about each of them, up to date as of this year:
Rheumatoid Arthritis Medication List (And What They Do, And How)
Finally, consider other lifestyle adjustments to manage your symptoms. These include:
- Exercise—gently, though! You do not want to provoke a flare-up, but you do want to maintain your mobility as best you can. There’s a use-it-or-lose-it factor here. Swimming and yoga are great options, as is tai chi. You may want to avoid exercises that involve repetitive impacts to your joints, like running.
- Rest—while keeping mobility going. Get good sleep at night (this is important), but don’t make your bed your new home, or your mobility will quickly deteriorate.
- Hot & cold—both can help, and alternating them can reduce inflammation and stiffness by improving your body’s ability to respond appropriately to these stimuli rather than getting stuck in an inappropriate-response state of inflammation.
- Mobility aids—if it helps, it helps. Maybe you only need something during a flare-up, but when that’s the case, you want to be as gentle on your body as possible while keeping moving, so if crutches, handrails etc help, then by all means get them and use them.
- Go easy on the use of braces, splints, etc—these can offer short-term relief, but at a long term cost of loss of mobility. Only you can decide where to draw the line when it comes to that trade-off.
You can also check out our previous article:
Managing Chronic Pain (Realistically!)
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Here’s Looking At Ya!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This Main Feature Should Take You Two Minutes (and 18 Seconds) To Read*
*Or at least, that’s what we’re told by our powerful software that checks things for readability!
Curious what that looks like? Try Out Hemingway App Online Here!
There’s a problem nobody wants to talk about when it comes to speed-reading
If you’re not very conscientious in your method, information does get lost. Especially, anything over 500 words per minute is almost certainly skimming and not true speed-reading.
One of the reasons information gets lost is because of a weird and wonderful feature of our eyes and brain: saccades.
Basically, our eyes can either collect visual information or they can move; they can’t do both at once. And as you may know, our eyes are almost always moving. So why aren’t we blind most of the time?
We actually are.
Did you know: your eyes take two upside-down 2D images and your brain presents you one 3D image the right way around instead? You probably did know that. So: it’s a bit like that.
Your brain takes a series of snapshots from whenever your eyes weren’t moving, and mentally fills in the blanks for you, just like a studio animation. We have a “frame rate” of about 60 frames per second, by the way—that’s why many computer monitors use that frequency. Lower frequencies can result in a noticeable flicker, and higher frequencies are wasted on us mere mortals!
Our eyes do some super-speedy movements called saccades (up to 500º per second! Happily no, our eyes don’t rotate 500º, but that’s the “per second” rate) and our brain fills in the gaps with its best guesses. The more you push it, the more it’ll guess wrong.
We’re not making this up, by the way! See for yourself:
Eye Movements In Reading And Information Processing: 20 Years Of Research
Fortunately, it is possible to use your eyes in a way that reduces the brain’s need to guess. That also means it has more processing power left over to guess correctly when it does need to.
Yes, There’s An App For That
Actually there are a few! But we’re going to recommend Spreeder as a top-tier option, with very rapid improvement right from day one.
It works by presenting the text with a single unmoving focal point. This is the opposite of traditional speed-reading methods that involve a rapidly moving pacer (such as your finger on the page, or a dot on the screen).
This unmoving focal point (while the words move instead) greatly reduces the number of saccades needed, and so a lot less information is lost to optical illusions and guesswork.
Try Spreeder (any platform) Here Now!
If you find that easy to use and would like something with a few more features, you might like another app that works on the same principle: Spritz.
It can take a bit more getting-used-to, but allows for greater integrations with all your favourite content in the long-run:
Check Out Spritz: Android App / iOS App / Free Chrome Extension
Lastly, if you don’t want any of those fancy apps and would just like to read more quickly and easily with less eye-strain, Beeline has you covered.
For free, unless you want to unlock some premium features!
How Beeline works is by adding a color gradient to text on websites and in documents. This makes it a lot easier for the eye to track without going off-piste, skipping a line, or re-reading the same bit again, etc.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: