Love Sense – by Dr. Sue Johnson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s quickly fact-check the subtitle:
- Is it revolutionary? It has a small element of controversy, but mostly no
- Is it new? No, it is based on science from the 70s that was expanded in the 80s and 90s and has been, at most, tweaked a little since.
- Is it science? Yes! It is so much science. This book comes with about a thousand references to scientific studies.
What’s the controversy, you ask? Dr. Johnson asserts, based on our (as a species) oxytocin responsiveness, that we are biologically hardwired for monogamy. This is in contrast to the prevailing scientific consensus that we are not.
Aside from that, though, the book is everything you could expect from an expert on attachment theory with more than 35 years of peer-reviewed clinical research, often specifically for Emotionally Focused Therapy (EFT), which is her thing.
The writing style is similar to that of her famous “Hold Me Tight: Seven Conversations For A Lifetime Of Love”, a very good book that we reviewed previously. It can be a little repetitive at times in its ideas, but this is largely because she revisits some of the same questions from many angles, with appropriate research to back up her advice.
Bottom line: if you are the sort of person who cares to keep working to improve your romantic relationship (no matter whether it is bad or acceptable or great right now), this book will arm you with a lot of deep science that can be applied reliably with good effect.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Too Much Salt May Lead To Organ Failure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Salt’s Health Risks… More Than Just Heart Disease!
It’s been well-established for a long time that too much salt is bad for cardiovascular health. It can lead to high blood pressure, which in turn can lead to many problems, including heart attacks.
A team of researchers has found that in addition to this, it may be damaging your organs themselves.
This is because high salt levels peel away the surfaces of blood vessels. How does this harm your organs? Because it’s through those walls that nutrients are selectively passed to where they need to be—mostly your organs. So, too much salt can indirectly starve your organs of the nutrients they need to survive. And you absolutely do not want your organs to fail!
❝We’ve identified new biomarkers for diagnosing blood vessel damage, identifying patients at risk of heart attack and stroke, and developing new drug targets for therapy for a range of blood vessel diseases, including heart, kidney and lung diseases as well as dementia❞
~ Newman Sze, Canada Research Chair in Mechanisms of Health and Disease, and lead researcher on this study.
See the evidence for yourself: Endothelial Damage Arising From High Salt Hypertension Is Elucidated by Vascular Bed Systematic Profiling
Diets high in salt are a huge problem in Canada, North America as a whole, and around the world. According to a World Health Organization (WHO) report released March 9, Canadians consume 9.1 grams of salt per day.
Read: WHO global report on sodium intake reduction
You may be wondering: who is eating over 9g of salt per day?
And the answer is: mostly, people who don’t notice how much salt is already in processed foods… don’t see it, and don’t think about it.
Meanwhile, the WHO recommends the average person to consume no more than five grams, or one teaspoon, of salt per day.
Read more: Massive efforts needed to reduce salt intake and protect lives
The American Heart Association, tasked with improving public health with respect to the #1 killer of Americans (it’s also the #1 killer worldwide—but that’s not the AHA’s problem), goes further! It recommends no more than 2.3g per day, and ideally, no more than 1.5g per day.
Some handy rules-of-thumb
Here are sodium-related terms you may see on food packages:
- Salt/Sodium-Free = Less than 5mg of sodium per serving
- Very Low Sodium = 35mg or less per serving
- Low Sodium = 140mg or less per serving
- Reduced Sodium = At least 25% less sodium per serving than the usual sodium level
- Light in Sodium or Lightly Salted = At least 50% less sodium than the regular product
Confused by milligrams? Instead of remembering how many places to move the decimal point (and potentially getting an “out by an order of magnitude error—we’ve all been there!), think of the 1.5g total allowance as being 1500mg.
See also: How much sodium should I eat per day? ← from the American Heart Association
Share This Post
-
Can you get sunburnt or UV skin damage through car or home windows?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When you’re in a car, train or bus, do you choose a seat to avoid being in the sun or do you like the sunny side?
You can definitely feel the sun’s heat through a window. But can you get sunburn or skin damage when in your car or inside with the windows closed?
Let’s look at how much UV (ultraviolet) radiation passes through different types of glass, how tinting can help block UV, and whether we need sunscreen when driving or indoors.
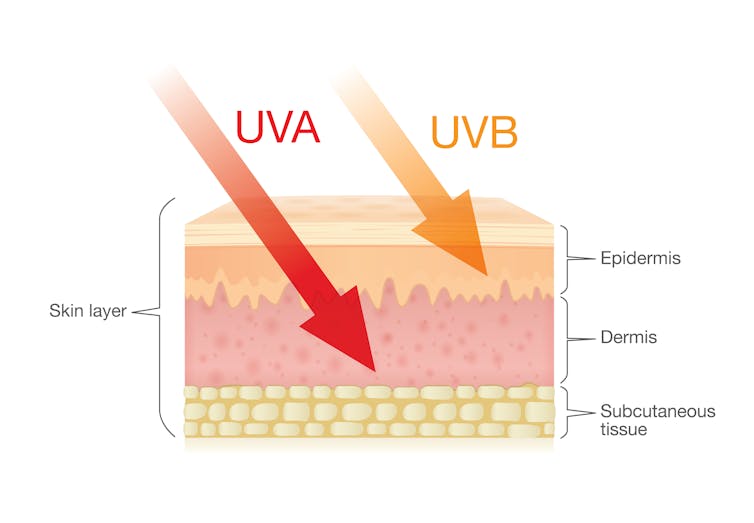
Zac Harris/Unsplash What’s the difference between UVA and UVB?
Of the total UV radiation that reaches Earth, about 95% is UVA and 5% is UVB.
UVB only reaches the upper layers of our skin but is the major cause of sunburn, cataracts and skin cancer.
UVA penetrates deeper into our skin and causes cell damage that leads to skin cancer.
UVA penetrates deeper than UVB. Shutterstock/solar22 Glass blocks UVA and UVB radiation differently
All glass used in house, office and car windows completely blocks UVB from passing through.
But only laminated glass can completely block UVA. UVA can pass through other glass used in car, house and office windows and cause skin damage, increasing the risk of cancer.
Car windscreens block UVA, but the side and rear windows don’t
A car’s front windscreen lets in lots of sunshine and light. Luckily it blocks 98% of UVA radiation because it is made of two layers of laminated glass.
But the side and rear car windows are made of tempered glass, which doesn’t completely block UVA. A study of 29 cars found a range from 4% to almost 56% of UVA passed through the side and rear windows.
The UVA protection was not related to the car’s age or cost, but to the type of glass, its colour and whether it has been tinted or coated in a protective film. Grey or bronze coloured glass, and window tinting, all increase UVA protection. Window tinting blocks around 95% of UVA radiation.
In a separate study from Saudi Arabia, researchers fitted drivers with a wearable radiation monitor. They found drivers were exposed to UV index ratings up to 3.5. (In Australia, sun protection is generally recommended when the UV index is 3 or above – at this level it takes pale skin about 20 minutes to burn.)
So if you have your windows tinted, you should not have to wear sunscreen in the car. But without tinted windows, you can accumulate skin damage.
UV exposure while driving increases skin cancer risk
Many people spend a lot of time in the car – for work, commuting, holiday travel and general transport. Repeated UVA radiation exposure through car side windows might go unnoticed, but it can affect our skin.
Indeed, skin cancer is more common on the driver’s side of the body. A study in the United States (where drivers sit on the left side) found more skin cancers on the left than the right side for the face, scalp, arm and leg, including 20 times more for the arm.
Another US study found this effect was higher in men. For melanoma in situ, an early form of melanoma, 74% of these cancers were on the on the left versus 26% on the right.
Earlier Australian studies reported more skin damage and more skin cancer on the right side.
Cataracts and other eye damage are also more common on the driver’s side of the body.
What about UV exposure through home or office windows?
We see UV damage from sunlight through our home windows in faded materials, furniture or plastics.
Most glass used in residential windows lets a lot of UVA pass through, between 45 and 75%.
Residential windows can let varied amounts of UVA through. Sherman Trotz/Pexels Single-pane glass lets through the most UVA, while thicker, tinted or coated glass blocks more UVA.
The best options are laminated glass, or double-glazed, tinted windows that allow less than 1% of UVA through.
Skylights are made from laminated glass, which completely stops UVA from passing through.
Most office and commercial window glass has better UVA protection than residential windows, allowing less than 25% of UVA transmission. These windows are usually double-glazed and tinted, with reflective properties or UV-absorbent chemicals.
Some smart windows that reduce heat using chemical treatments to darken the glass can also block UVA.
So when should you wear sunscreen and sunglasses?
The biggest risk with skin damage while driving is having the windows down or your arm out the window in direct sun. Even untinted windows will reduce UVA exposure to some extent, so it’s better to have the car window up.
For home windows, window films or tint can increase UVA protection of single pane glass. UVA blocking by glass is similar to protection by sunscreen.
When you need to use sunscreen depends on your skin type, latitude and time of the year. In a car without tinted windows, you could burn after one hour in the middle of the day in summer, and two hours in the middle of a winter’s day.
But in the middle of the day next to a home window that allows more UVA to pass through, it could take only 30 minutes to burn in summer and one hour in winter.
When the UV index is above three, it is recommended you wear protective sunglasses while driving or next to a sunny window to avoid eye damage.
Theresa Larkin, Associate Professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
3 Things Everyone Over 50 Must Do Daily for Healthy Feet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Will Harlow, the over-50s specialist physio, wants you to be on a good footing:
Daily steps in the right direction
The three daily exercises recommended in the video are:
Exercise 1: Towel Scrunch
The towel scrunch exercise strengthens the flexor muscles in the feet, improving balance and improving contact with the ground. To do this exercise, sit on a chair with a towel placed on the floor beneath your toes while keeping your heels on the ground. Use only your toes to pull the towel toward your heel, scrunching it up as much as possible. This movement strengthens the arch of the foot and can help alleviate symptoms of flat feet. For best results, practice this exercise for 2–3 minutes once or twice daily. Once you’ve got the hand of doing it sitting, do it while standing.
Exercise 2: Big Toe Extension
Big toe extension is an essential exercise for maintaining foot mobility and improving walking kinesthetics by preventing stiffness in the big toe. To do this exercise, keep your foot flat on the floor and try to lift only your big toe while keeping the four other toes firmly pressed down. To be clear, we mean under its own power; not using your hands to help. Many people find this difficult initially, but it’s due to a loss of neural connection rather than muscle strength, so with practice, the ability to isolate the movement improves quite quickly. Perform 10 repetitions in a row, three times per day, for optimal benefits. Once you’ve got the hand of doing it sitting, do it while standing.
Exercise 3: Calf Stretch
The calf stretch is an important exercise for maintaining foot health by preventing tight calves, which can contribute to issues like plantar fasciitis and Morton’s neuroma. To do this stretch, place your hands against a wall for support and extend one leg straight behind you while keeping your other heel firmly on the floor. The front knee should be bent while the back leg remains straight, creating a stretch in the calf. Hold this position for 30 seconds (building up to that, if necessary). Since the effectiveness of stretching comes from frequency rather than duration, this stretch should be performed three to four times per day for the best results.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation ← this one’s about general habits, not exercises
Take care!
Share This Post
Related Posts
-
Sunflower Seeds vs Sesame Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sunflower seeds to sesame seeds, we picked the sunflower.
Why?
In moderation, both are very healthy. We say “in moderation” because they’re both about 50% fat and such fats, while vital for life, are generally best enjoyed in small portions. Of that fat, sunflower has the slightly better fat profile; they’re both mostly poly- and monounsaturated fats, but sunflower has 10% saturated fat while sesame has 15%. Aside from fats, sunflower has slightly more protein and sesame has slightly more carbs. While sesame has slightly more fiber, because of the carb profile sunflower still has the lower glycemic index. All in all, a moderate win for sunflower in the macros category.
You may be wondering, with all that discussion of fats, what they’re like for omega-3, and sesame seeds have more omega-3, though sunflower seeds contain it too. Still, a point in sesame’s favor here.
When it comes to vitamins, sunflower has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, and choline, while sesame is not higher in any vitamins.
In the category of minerals, sunflower has more phosphorus, potassium, and selenium, while sesame has more calcium, copper, iron, and zinc. This is nominally a marginal win for sesame, but it should be noted that sunflower is still very rich in copper, iron, and zinc too (but not calcium).
Adding up the categories makes for a moderate win for sunflower seeds, but as ever, enjoy both; diversity is best!
Want to learn more?
You might like to read:
Sunflower Seeds vs Pumpkin Seeds – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Black Beans vs Pinto Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing black beans to pinto beans, we picked the pinto beans.
Why?
Both of these beans have won all their previous comparisons, so it’s no surprise that this one was very close. Despite their different appearance, taste, and texture, their nutritional profiles are almost identical:
In terms of macros, pinto beans have a tiny bit more protein, carbs, and fiber. So, a nominal win for pinto beans, but again, the difference is very slight.
When it comes to vitamins, black beans have more of vitamins A, B1, B3, and B5, while pinto beans have more of vitamins B2, B6, B9, C, E, K and choline. Superficially, again this is nominally a win for pinto beans, but in most cases the differences are so slight as to be potentially the product of decimal place rounding.
In the category of minerals, black beans have more calcium, copper, iron, and phosphorus, while pinto beans have more magnesium, manganese, selenium, and zinc. That’s a 4:4 tie, but the only one with a meaningful margin of difference is selenium (of which pinto beans have 4x more), so we’re calling this one a very modest win for pinto beans.
All in all, adding these up makes for a “if we really are pressed to choose” win for pinto beans, but honestly, enjoy either in accordance with your preference (this writer prefers black beans!), or better yet, both.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lobster vs Crab – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lobster to crab, we picked the crab.
Why?
Generally speaking, most seafood is healthy in moderation (assuming it’s well-prepared, not poisonous, and you don’t have an allergy), and for most people, these two sea creatures are indeed considered a reasonable part of a healthy balanced diet.
In terms of macros, they’re comparable in protein, and technically crab has about 2x the fat, but in both cases it’s next to nothing, so 2x almost nothing is still almost nothing. And, if we break down the lipids profiles, crab has a sufficiently smaller percentage of saturated fat (compared to monounsaturated and polyunsaturated), that crab actually has less saturated fat than lobster. In balance, the category of macros is either a tie or a slight win for crab, depending on your personal priorities.
When it comes to vitamins, crab wins easily with more of vitamins A, B1, B2, B6, B9, B12, and C, in most cases by considerable margins (we’re talking multiples of what lobster has). Lobster, meanwhile, has more of vitamin B3 (tiny margin) and vitamin B5 (pantothenic acid, as in, the vitamin that’s in basically everything edible, and thus almost impossible to be deficient in unless literally starving).
The minerals scene is more balanced; lobster has more calcium, copper, manganese, and selenium, while crab has more iron, magnesium, phosphorus, potassium, and zinc. The margins are comparable from one creature to another, so all in all the 4:5 score means a modest win for crab.
Both of these creatures are good sources of omega-3 fatty acids, but crab is better.
Lobster and crab are both somewhat high in cholesterol, but crab is the relatively lower of the two.
In short: for most people most of the time, both are fine to enjoy in moderation, but if picking one, crab is the healthier by most metrics.
Want to learn more?
You might like to read:
Shrimp vs Caviar – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: