Woman Petitions Health Insurer After Company Approves — Then Rejects — Her Infusions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When KFF Health News published an article in August about the “prior authorization hell” Sally Nix said she went through to secure approval from her insurance company for the expensive monthly infusions she needs, we thought her story had a happy ending.
That’s because, after KFF Health News sent questions to Nix’s insurance company, Blue Cross Blue Shield of Illinois, it retroactively approved $36,000 worth of treatments she thought she owed. Even better, she also learned she would qualify for the infusions moving forward.
Good news all around — except it didn’t last for long. After all, this is the U.S. health care system, where even patients with good insurance aren’t guaranteed affordable care.
To recap: For more than a decade, Nix, of Statesville, North Carolina, has suffered from autoimmune diseases, chronic pain, and fatigue, as well as a condition called trigeminal neuralgia, which is marked by bouts of electric shock-like pain that’s so intense it’s commonly known as the “suicide disease.”
“It is a pain that sends me to my knees,” Nix said in October. “My entire family’s life is controlled by the betrayal of my body. We haven’t lived normally in 10 years.”
Late in 2022, Nix started receiving intravenous immunoglobulin infusions to treat her diseases. She started walking two miles a day with her service dog. She could picture herself celebrating, free from pain, at her daughter’s summer 2024 wedding.
“I was so hopeful,” she said.
But a few months after starting those infusions, she found out that her insurance company wouldn’t cover their cost anymore. That’s when she started “raising Cain about it” on Instagram and Facebook.
You probably know someone like Sally Nix — someone with a chronic or life-threatening illness whose doctor says they need a drug, procedure, or scan, and whose insurance company has replied: No.
Prior authorization was conceived decades ago to rein in health care costs by eliminating duplicative and ineffective treatment. Not only does overtreatment waste billions of dollars every year, but doctors acknowledge it also potentially harms patients.
However, critics worry that prior authorization has now become a way for health insurance companies to save money, sometimes at the expense of patients’ lives. KFF Health News has heard from hundreds of people in the past year relating their prior authorization horror stories.
When we first met Nix, she was battling her insurance company to regain authorization for her infusions. She’d been forced to pause her treatments, unable to afford $13,000 out-of-pocket for each infusion.
Finally, it seemed like months of her hard work had paid off. In July, Nix was told by staff at both her doctor’s office and her hospital that Blue Cross Blue Shield of Illinois would allow her to restart treatment. Her balance was marked “paid” and disappeared from the insurer’s online portal.
But the day after the KFF Health News story was published, Nix said, she learned the message had changed. After restarting treatment, she received a letter from the insurer saying her diagnoses didn’t actually qualify her for the infusions. It felt like health insurance whiplash.
“They’re robbing me of my life,” she said. “They’re robbing me of so much, all because of profit.”
Dave Van de Walle, a spokesperson for Blue Cross Blue Shield of Illinois, said the company would not discuss individual patients’ cases.
“Prior authorization is often a requirement for certain treatments,” Van de Walle said in a written statement, “and BCBSIL administers benefits according to medical policy and the employer’s benefit.”
But Nix is a Southern woman of the “Steel Magnolia” variety. In other words, she’s not going down without a fight.
In September, she called out her insurance company’s tactics in a http://change.org/ campaign that has garnered more than 21,000 signatures. She has also filed complaints against her insurance company with the U.S. Department of Health and Human Services, U.S. Department of Labor, Illinois Department of Insurance, and Illinois attorney general.
Even so, Nix said, she feels defeated.
Not only is she still waiting for prior authorization to restart her immunoglobulin infusions, but her insurance company recently required Nix to secure preapproval for another treatment — routine numbing injections she has received for nearly 10 years to treat the nerve pain caused by trigeminal neuralgia.
“It is reprehensible what they’re doing. But they’re not only doing it to me,” said Nix, who is now reluctantly taking prescription opioids to ease her pain. “They’re doing it to other patients. And it’s got to stop.”
Do you have an experience with prior authorization you’d like to share? Click here to tell your story.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 7 Approaches To Pain Management
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More Than One Way To Kill Pain
This is Dr. Deepak Ravindran (MD, FRCA. FFPMRCA, EDRA. FIPP, DMSMed). He has decades of experience and is a specialist in acute and chronic pain management, anesthesia, musculoskeletal medicine, and lifestyle medicine.
A quick catch-up, first:
We’ve written about chronic pain management before:
Managing Chronic Pain (Realistically!)
As well as:
Science-Based Alternative Pain Relief
Dr. Ravindran’s approach
Dr. Ravindran takes a “trauma-informed care” approach to his professional practice, and recommends the same for others.
In a nutshell, this means starting from a position of not “what’s wrong with you?”, but rather “what happened to you?”.
This seemingly subtle shift is important, because it means actually dealing with a person’s issues, instead of “take one of these and call my secretary next month”. Read more:
Pain itself can be something of a many-headed hydra. Dr. Ravindran’s approach is equally many-headed; specifically, he has a 7-point plan:
Medications
Dr. Ravindran sees painkillers (and a collection of other drugs, like antidepressants and muscle relaxants) as a potential means to an end worth exploring, but he doesn’t expect them to be the best choice for everyone, and nor does he expect them to be a cure-all. Neither should we. He also advises being mindful of the drawbacks and potential complications of these drugs, too.
Interventions
Sometimes, surgery is the right choice. Sometimes it isn’t. Often, it will change a life—one way or the other. Similar to with medications, Dr. Ravindran is very averse to a “one size fits all” approach here. See also:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Neuroscience and stress management
Often a lot of the distress of pain is not just the pain itself, but the fear associated with it. Will it get worse if I move wrong or eat the wrong thing? How long will it last? Will it ever get better? Will it get worse if I do nothing?. Dr. Ravindran advises tackling this, with the same level of importance as the pain itself. Here’s a good start:
Stress, And Building Psychological Resilience
Diet and the microbiome
Many chronic illnesses are heavily influenced by this, and Dr. Ravindran’s respect for lifestyle medicine comes into play here. While diet might not fix all our ills, it certainly can stop things from being a lot worse. Beyond the obvious “eat healthily” (Mediterranean diet being a good starting point for most people), he also advises doing elimination tests where appropriate, to screen out potential flare-up triggers. You also might consider:
Four Ways To Upgrade The Mediterranean Diet
Sleep
“Get good sleep” is easy advice for those who are not in agonizing pain that sometimes gets worse from staying in the same position for too long. Nevertheless, it is important, and foundational to good health. So it’s important to explore—whatever limitations one might realistically have—what can be done to improve it.
If you can only sleep for a short while at a time, you may get benefit from this previous main feature of ours:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Exercise and movement
The trick here is to move little and often; without overdoing it, but without permitting loss of mobility either. See also:
The Doctor Who Wants Us To Exercise Less, And Move More
Therapies of the mind and body
This is about taking a holistic approach to one’s wellness. In Dr. Ravindran’s words:
❝Mind-body therapies are often an extremely sensitive topic about which people hold very strong opinions and sometimes irrational beliefs.
Some, like reiki and spiritual therapy and homeopathy, have hardly any scientific evidence to back them up, while others like yoga, hypnosis, and meditation/mindfulness are mainstream techniques with many studies showing the benefits, but they all work for certain patients.❞
In other words: evidence-based is surely the best starting point, but if you feel inclined to try something else and it works for you, then it works for you. And that’s a win.
Want to know more?
You might like his book…
The Pain-Free Mindset: 7 Steps to Taking Control and Overcoming Chronic Pain
He also has a blog and a podcast.
Take care!
Share This Post
-
Six Ways To Eat For Healthier Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sadia Badiei, the nutritionist-chef of “Pick Up Limes” fame, has advice:
More than skin-deep:
We’ll not keep them a mystery; here are the six points of focus:
1. Collagen and skin elasticity
Collagen is the structural protein that provides firmness and elasticity to the skin, but its production decreases with age, resulting in about a 1% annual loss starting at age 20. To support collagen, a diet rich in protein is essential, including foods like beans, lentils, tofu, tempeh, nuts, and seeds. They can’t do their work alone though; vitamins C and E play a critical role in collagen production and repair, protecting against damage from sun exposure, pollution, and free radicals. Vitamin E can be found in almonds, sunflower seeds, leafy greens, peanuts, and avocados, while vitamin C is abundant in citrus fruits, bell peppers, and broccoli.
2. Skin healing and zinc
Zinc is critical for wound healing and reducing inflammation, making it particularly helpful in managing skin conditions such as acne, eczema, psoriasis, and rosacea. Great dietary sources of zinc include nutritional yeast, pumpkin, sesame, and hemp seeds, as well as legumes and whole grains. However, zinc absorption can be hindered by phytate levels in some foods. Soaking, sprouting, or fermenting foods where possible can correct for that and improve zinc absorption.
3. Dry skin and hydration
Dry skin can result from many things, including dry air, hot water, abrasive soaps, and certain medications. While moisturizers provide external hydration, dietary omega-3 fats are essential for improving the skin’s barrier function, helping it retain moisture. Plant-based sources of omega-3s include walnuts, hemp seeds, chia seeds, flax seeds, and algae-based supplements. Staying adequately hydrated also supports overall health of course (everything runs on water in one way or another, after all), which indirectly benefits skin hydration, although drinking additional water only helps if dehydration is present.
4. Sebum regulation
Sebum, an oily substance that lubricates the skin, can cause issues like acne and blackheads when overproduced. Hormonal fluctuations and diet both influence sebum levels (in either direction). High glycemic index foods, such as sweetened beverages, refined grains, and sugary snacks, can lead to spikes in insulin, which in turn stimulates excess sebum production. In contrast, low glycemic index foods like vegetables, whole grains, tofu, nuts, and seeds regulate blood sugar and help manage sebum production, promoting clearer skin without an excess or a shortage of sebum.
5. Gut health and skin
The gut-skin connection means that imbalances in gut bacteria can contribute to skin issues like acne, eczema, and psoriasis. Supporting gut health involves increasing the diversity of beneficial bacteria through probiotic-rich foods. Fermented options like plant-based yogurts, kimchi, miso, sauerkraut, and kombucha not only improve gut microbiome health but also positively impact skin health by reducing inflammation and improving overall skin conditions.
6. Inflammation and skin health
Chronic inflammation is associated with so many health issues, and when it comes to skin, that includes acne, rosacea, and even wrinkles. Anti-inflammatory foods, especially those rich in antioxidants, can mitigate these effects and improve skin elasticity, smoothness, and color. Diets centered around fruits, vegetables, and other plant-based foods provide the necessary nutrients to combat inflammation, showcasing the significant role of nutrition in promoting radiant, healthy skin.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Undo The Sun’s Damage To Your Skin
Take care!
Share This Post
-
Keep Cellulite At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Does anything actually get rid of cellulite? Nothing seems to❞
Let’s get the bad news over with in one go:
Nothing (that the scientific world currently knows of) can get rid of cellulite permanently, nor completely guard against it proactively. Which, given that it affects up to 98% of women to some degree, and often shows up not long after puberty (though it can appear at any time and often increases later in life), any pre-emptive health regime would need to be started as a child in any case.
As with many things that predominantly affect women, the world of medicine isn’t entirely sure what causes it, let alone how to effectively treat it.
Obviously hormones are implicated, namely estrogen.
Obviously adiposity is implicated, because one can’t have dimples in one’s fat if one doesn’t have enough fat to dimple.
Other hypothesized contributory factors include genetics, poor diet, inactivity, unhealthy lifestyle (in ways not previously mentioned, e.g. use of alcohol, tobacco, etc), accumulated toxins, and pregnancy.
Here’s an old paper (from 2004); today’s reviews say pretty much the same thing, but we love how succinctly (albeit, somewhat depressingly) this abstract states how little we know and how little we can do:
Cellulite: a review of its physiology and treatment
However, all is not lost!
There are some things that can affect how much cellulite we get, and there are some things that can reduce it, and even some things that can get rid of it completely—albeit temporarily.
First, a quick refresher on what it actually is, physiologically speaking: cellulite occurs when connective tissue bands pull the skin down in places, where fat tissue has been able to squeeze through. One of the reasons it is hypothesized women get this more than men is because our fat is not merely different in distribution and overall percentage, but also in how the fat cells stack up; we generally have have of a vertical stacking structure going on, while men generally have a more horizontal structure. This means that it can be easier for ours to get moved about differently, causing the connective tissue to pull on the skin unevenly in places.
With that in mind…
Prevention is, as we say, probably impossible if your body is running on estrogen. However, those contributory factors we mentioned above? Most of those are modifiable, including these things that it is hypothesized can reduce it:
Diet: as it seems to be worsened by inflammation (what isn’t?), an anti-inflammatory diet is recommended.
Exercise: there are three things here: 1) exercises to improve circulation and thus the body’s ability to sort things out by itself 2) HIIT exercise to reduce body fat percentage, if one has a high enough starting body fat percentage for that to be a healthy goal 3) mobility exercises, to ensure our connective tissues are the right amount of mobile.
Creams and lotions
These reduce the superficial appearance of cellulite, without actually treating the thing itself. Mostly they are caffeine-based, which when used topically increases blood flow and works as a local diuretic, reducing the water content of the fat cells, diminishing the appearance of the cellulite by making each fat cell physically smaller (while still containing the same amount of fat, and it’ll bounce back in size as soon as the body can restore osmotic balance).
Medical procedures
There are too many of these to discuss them all separately, but they all work on the principle of breaking up the tough bands of connective tissue to eliminate the dimpling of cellulite.
The methods they use vary from ultrasound to cryolipolysis to lasers to “vacuum-assisted precise tissue release”, which involves a suction pump and a multipronged robotic assembly with needles to administer anaesthetic as it goes and small blades to cut the connective tissues under the skin:
Tissue Stabilized–Guided Subcision for the Treatment of Cellulite
That last one definitely sounds like the least fun, but it’s also the only one that doesn’t take months to maybe see results.
Cellulite can and almost certainly will come back after all of these.
Home remedies
Aside from at-home versions of the above (not the robots with vacuum pumps and needles and microblades, hopefully, but for example homemade caffeine creams), and of course diet and exercise which can be considered “home remedies”, there are two more things worth mentioning:
Dry brushing: using a body brush to, as the name suggests, simply brush one’s skin. The “dry” aspect here is simply that it’s not done in the bath or shower; it’s done while dry. It can improve local circulation of blood and lymph, allowing for better detoxification and redistribution of needed bodily resources.
Here’s an example dry brushing body brush on Amazon; this writer has one and hates it, but I’ve also tried with other kinds of brush and hate them too, so it seems to be a me thing rather than a brush thing, and I have desisted in trying, now. Maybe you will like it better; many people do.
Self-massage: or massage by someone else, if that’s an option for you and you prefer. In this case, it works by a different mechanism than dry brushing; this time it’s working by the same principle as the medical techniques described in the previous section; it’s physically breaking down the toughened bits of connective tissue.
Here’s an example wooden massage roller on Amazon; this writer has one and loves it; it’s sooooooo good. I got it as a matter of general maintenance for my fascia, but it’s also very good if I get a muscular pain now and again. As for cellulite, I personally get just a little cellulite sometimes (in the backs of my thighs), and whenever I use this regularly, it goes away for at least a while.
A quick note in closing
Cellulite is normal for women and is not unhealthy. Much like gray hair for example, it’s something that can be increased by poor health, but the thing itself isn’t intrinsically unhealthy, and most of us get it to some degree at some point.
Nevertheless, aesthetic factors can also have a role to play in mental health, and we tend to feel best when we like the way our body looks. If for you that means wanting less/no cellulite, then the above are some ways towards that.
As a bonus, most of the nonmedical options are directly good for the physical health anyway, so doing them is of course good.
In particular that last one (the wooden massage roller), because that connective tissue we talked about? It matters for a lot more than just cellulite, and is heavily implicated in a lot of kinds of chronic pain, so it pays to keep it in good health:
Fascia: Why (And How) You Should Take Care Of Yours
(that article, also written by this same writer by the way, suggests a vibrating foam roller—those are very popular; I just really love my wooden one, and find it more effective)
Take care!
Share This Post
Related Posts
-
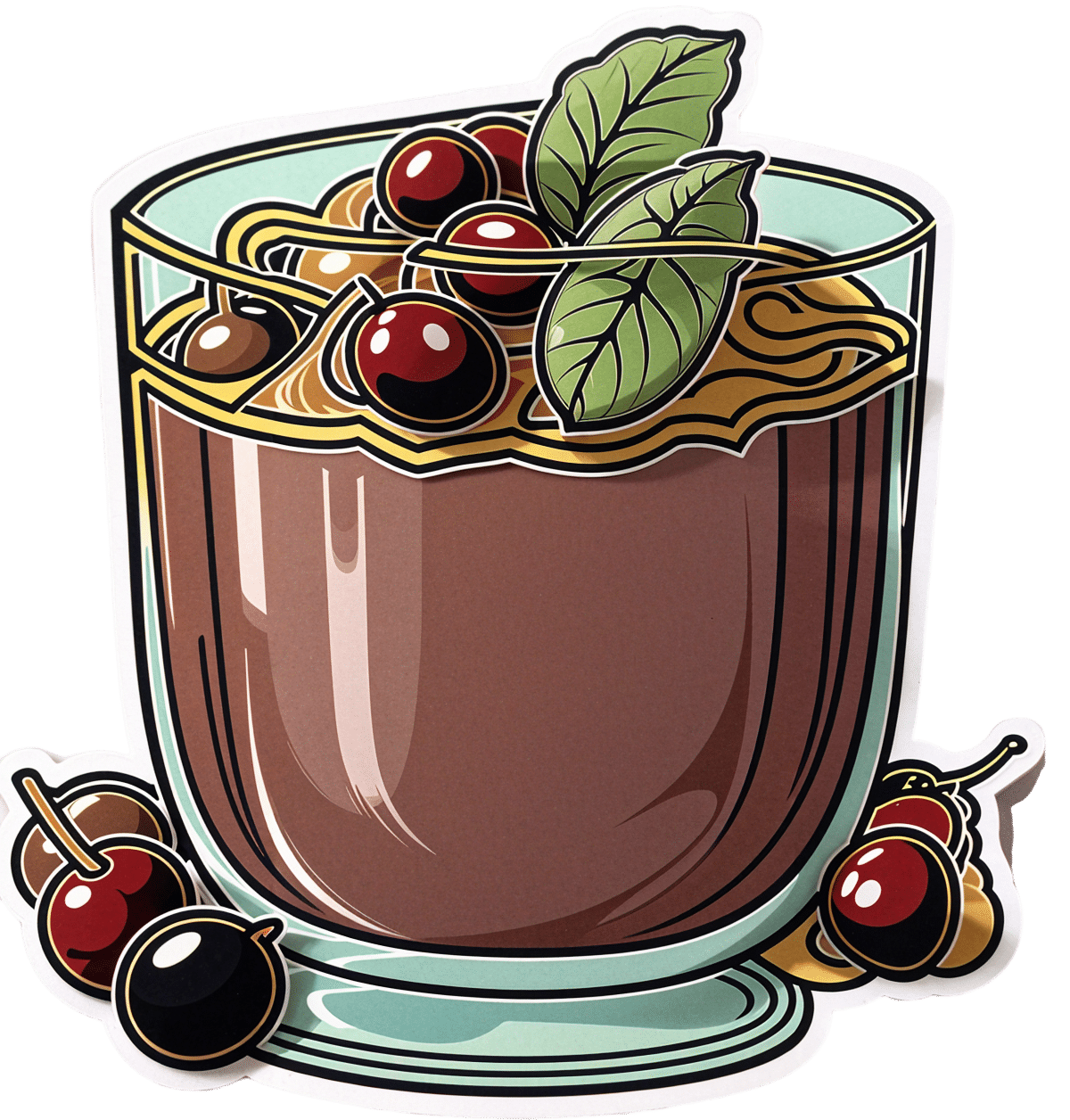
Black Forest Chia Pudding
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This pudding tastes so decadent, it’s hard to believe it’s so healthy, but it is! Not only is it delicious, it’s also packed with nutrients including protein, carbohydrates, healthy fats (including omega-3s), fiber, vitamins, minerals, and assorted antioxidant polyphenols. Perfect dessert or breakfast!
You will need
- 1½ cups pitted fresh or thawed-from-frozen cherries
- ½ cup mashed banana
- 3 tbsp unsweetened cocoa powder
- 2 tbsp chia seeds, ground
- Optional: 2 pitted dates, soaked in hot water for 10 minutes and then drained (include these if you prefer a sweeter pudding)
- Garnish: a few almonds, and/or berries, and/or cherries and/or cacao nibs
Method
(we suggest you read everything at least once before doing anything)
1) Blend the ingredients except for the chia seeds and the garnish, with ½ cup of water, until completely smooth
2) Divide into two small bowls or glass jars
3) Add 1 tbsp ground chia seeds to each, and stir until evenly distributed
4) Add the garnish and refrigerate overnight or at least for some hours. There’s plenty of wiggle-room here, so make it at your convenience and serve at your leisure.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Cherries’ Very Healthy Wealth Of Benefits!
- If You’re Not Taking Chia, You’re Missing Out
- Cacao vs Carob – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The FDA Just Redefined “Healthy”—But How?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the ongoing war of labelling regulations (usually with advertisers on one side and regulators on the other), the FDA has updated what’s required in order to label a food as “healthy”.
Here’s what they’re now* requiring:
To bear the “healthy” claim, a food product needs to:
- Contain a certain amount of food (food group equivalent) from at least one of the food groups or subgroups (such as fruits, vegetables, fat-free and low-fat dairy etc.) recommended by the Dietary Guidelines.
- Adhere to specified limits for the following nutrients: saturated fat, sodium, and added sugars.
Source: FDA | Press Releases | FDA Finalizes Updated “Healthy” Nutrient Content Claim
*however, manufacturers have 3 years to conform, which if we’re being cynical about it, looks suspiciously like just short of a US presidential election cycle so that actual enforcement will be someone else’s problem.
Will it help?
Maybe! It’s not too dissimilar to the “traffic light system” already in use in Europe, although that currently emphasizes the absence/presence of “bad things” e.g. saturated fat, sodium, and added sugars.
It has its faults, because for example…
- not all saturated fat is bad, and a jar of coconut oil is now definitely going to get labelled as very unhealthy
- low-sodium salt is, ironically, going to to get flagged as being very high in sodium and therefore unhealthy
This latter is because on a g/100g basis, a product that’s ⅓ sodium chloride is going to have a lot of sodium, even if it’s approaching ⅔ less sodium than the product it’s (healthily!) replacing.
However, on a large scale, these kinds of problems are surely going to be small next to (hopefully) manufacturers scrambling to find ways to cut down on the saturated fats, sodium, and added sugars.
You may be wondering…
What will they replace them with?
Sometimes, companies trying to make something healthier will mess up, like when the health risks of smoking hit public consciousness, one cigarette company had the bright idea of putting asbestos in their filter tips, to market them as healthier. So, could something similar happen here?
- Saturated fat: definitely could; because the health benefits/risks of different kinds of fats and their constituent fatty acids are a lot more nuanced than just “saturated” vs “mono-/polyunsaturated”, it is definitely possible that companies may replace healthier saturated-heavy fats with less healthy unsaturated fats, depending on what is cheaper.
- See also: Can Saturated Fats Be Healthy?
- Sodium: probably not; likely go-to replacements for sodium chloride will be potassium chloride (healthier than sodium chloride) and MSG (has an unearned bad reputation in the US, but is healthier than sodium chloride).
- Added sugars: probably—things get very complicated very quickly when it comes to artificial sweeteners, and also the crux will definitely lie in what gets defined as an “added sugar”; watch out for a rise in the use of things that slide by the definition of added sugar while still being chemically (and, which is important, metabolically) the same thing.
Well that doesn’t sound great
It doesn’t, but on the flipside, the positive inclusions will probably be mostly good.
For example, the only way to get a “healthy” labelling in including fiber is to include more fiber, same with vitamins and minerals.
The low-fat dairy thing could possibly get abused (much like with the general “low-fat” trend of the 80s).
The “portion of fruit” thing will need to be carefully defined to avoid running straight back into the “this is just added sugar by another name” problem; mostly that it’ll need to still include the same amount of fiber as was in the whole fruit, gram for gram.
See also: What Matters Most For Your Heart? ← it’s about fiber, not salt or saturated fats!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bridging The Generation Gap Over The Holidays
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Often seen as a time for family connection, this same holiday period is often experienced as a time of family tension. But it doesn’t have to be that way!
Hopefully this will be of benefit to readers of all ages, but we’re going to write with the largest age-group of our readership, which is people who are most likely to have Gen-Z grandkids.
why are we writing about this?
Not only are health and happiness closely linked, and not only is mental health also just health, but… In terms of the healthy longevity secrets of the “Blue Zones”, strong intergenerational connections are usually a feature.
First, the obvious:
Any holiday tensions, of course, don’t usually start with grandkids, and are more likely amongst the adults, but some points of friction can be the same:
- Differences of opinion on political/social/economic issues
- Difference of opinion on parenting/dating choices
- Differences of opinion on life priorities
And yes, by the way, that includes even young teens (and perhaps younger) having opinions on these things—we are living in an information age, and this does mean a lot of information is a lot more accessible than it used to be, including for kids. Problems (at all ages) may occur when someone is only really exposed to views from within a certain “bias bubble”, but for better or worse, most people will have an opinion on most well-known things.
As a general rule of thumb, all of these differences of opinion can be shelved if (and only if) those involved seek to avoid conflict. And while age is no guarantee of maturity, often it’ll be the older person(s) in the strongest position to redirect things. So, have a stack of “safe” topics up your sleeve.
Bonus: you can also have non-conversational distractions up your sleeve! These may be kitchen-related, for example (time to produce something distracting, or if the nascent conflict was only between you and one other person, time to go check on something, thus removing yourself from the situation).
Next, about “family time” and technology
It can be tempting to try to have a “phones away” rule, but this will tend to only exacerbate a younger person’s withdrawal.
Better: ask (with a tone of cheerful curiosity, not accusation) about what captures their attention so. Ask about their favorite YouTubers or TikTokers or whatever it is that it is for them. Learn about that Subreddit.
Or maybe (more likely for Millennials) they were following what is going on in the world via social media, which takes on an intermediary role for the delivery of world news. Hopefully this won’t run into the differences of opinion that we mentioned up top, but it could also be a perfectly good avenue of conversation, and maybe there’s more common ground than you might expect.
Meanwhile, if you’re the older generation present, chances are your own social media use is more about the human element. That’s great, but watch out:
A common faux pas is taking pictures without asking, let alone posting them online without asking. For many people this may seem an odd thing to object to, but generationally speaking, the younger someone is (down to the upper single digits, anyway) the more likely they might feel strongly about this. So, ask first.
The reason, by the way, is that in this age of digital hypervisibility, what we choose to share online can be a deeply personal thing. And, say what you will about the pros or cons of someone carefully curating an image of how they wish to be seen, shortcutting through that for them with a candid photo posted on Facebook will not endear you to them, even if you can’t see anything wrong with the photo in question, for example.
See also: Make Social Media Work For Your Mental Health
Show an interest, but don’t interrogate
This one doesn’t take too much explanation. If people want to share about their lives, they’ll need only the smallest nudge to do so. If someone passes up an opportunity to talk about something you showed an interest in, chances are they have their own reasons for not wanting to talk about it. This might be hurtful if you feel like they’re keeping you out of their life, but the best way to get them to talk to you is just to be a good listener—not an interrogator that they have to dodge.
For some powerful tools on this, see: Listening, Better
Lastly, if things aren’t so good…
43% of people are currently experiencing some sort of familial estrangement, so if that’s you, you’re not on your own.
Sometimes, it really is too late to fix things, but sometimes it isn’t; we put together a guide that might help:
Family Estrangement & How To Fix It
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: