Getting antivirals for COVID too often depends on where you live and how wealthy you are
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medical experts recommend antivirals for people aged 70 and older who get COVID, and for other groups at risk of severe illness and hospitalisation from COVID.
But many older Australians have missed out on antivirals after getting sick with COVID. It is yet another way the health system is failing the most vulnerable.

Who missed out?
We analysed COVID antiviral uptake between March 2022 and September 2023. We found some groups were more likely to miss out on antivirals including Indigenous people, people from disadvantaged areas, and people from culturally and linguistically diverse backgrounds.
Some of the differences will be due to different rates of infection. But across this 18-month period, many older Australians were infected at least once, and rates of infection were higher in some disadvantaged communities.
How stark are the differences?
Compared to the national average, Indigenous Australians were nearly 25% less likely to get antivirals, older people living in disadvantaged areas were 20% less likely to get them, and people with a culturally or linguistically diverse background were 13% less likely to get a script.
People in remote areas were 37% less likely to get antivirals than people living in major cities. People in outer regional areas were 25% less likely.
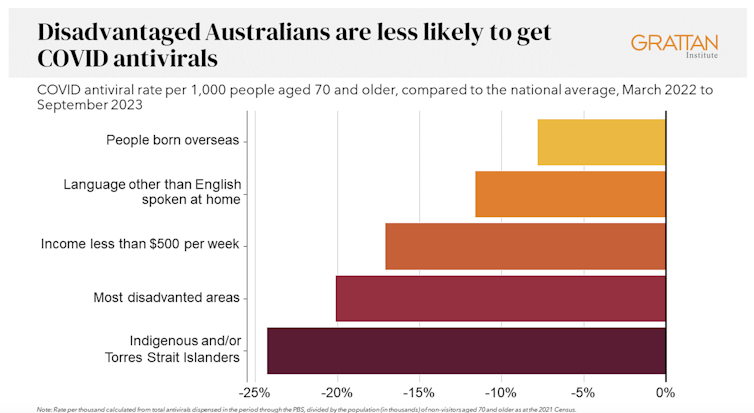
Even within the same city, the differences are stark. In Sydney, people older than 70 in the affluent eastern suburbs (including Vaucluse, Point Piper and Bondi) were nearly twice as likely to have had an antiviral as those in Fairfield, in Sydney’s south-west.
Older people in leafy inner-eastern Melbourne (including Canterbury, Hawthorn and Kew) were 1.8 times more likely to have had an antiviral as those in Brimbank (which includes Sunshine) in the city’s west.
Why are people missing out?
COVID antivirals should be taken when symptoms first appear. While awareness of COVID antivirals is generally strong, people often don’t realise they would benefit from the medication. They wait until symptoms get worse and it is too late.
Frequent GP visits make a big difference. Our analysis found people 70 and older who see a GP more frequently were much more likely to be dispensed a COVID antiviral.
Regular visits give an opportunity for preventive care and patient education. For example, GPs can provide high-risk patients with “COVID treatment plans” as a reminder to get tested and seek treatment as soon as they are unwell.
Difficulty seeing a GP could help explain low antiviral use in rural areas. Compared to people in major cities, people in small rural towns have about 35% fewer GPs, see their GP about half as often, and are 30% more likely to report waiting too long for an appointment.
Just like for vaccination, a GP’s focus on antivirals probably matters, as does providing care that is accessible to people from different cultural backgrounds.
Care should go those who need it
Since the period we looked at, evidence has emerged that raises doubts about how effective antivirals are, particularly for people at lower risk of severe illness. That means getting vaccinated is more important than getting antivirals.
But all Australians who are eligible for antivirals should have the same chance of getting them.
These drugs have cost more than A$1.7 billion, with the vast majority of that money coming from the federal government. While dispensing rates have fallen, more than 30,000 packs of COVID antivirals were dispensed in August, costing about $35 million.
Such a huge investment shouldn’t be leaving so many people behind. Getting treatment shouldn’t depend on your income, cultural background or where you live. Instead, care should go to those who need it the most.

People born overseas have been 40% more likely to die from COVID than those born here. Indigenous Australians have been 60% more likely to die from COVID than non-Indigenous people. And the most disadvantaged people have been 2.8 times more likely to die from COVID than those in the wealthiest areas.
All those at-risk groups have been more likely to miss out on antivirals.
It’s not just a problem with antivirals. The same groups are also disproportionately missing out on COVID vaccination, compounding their risk of severe illness. The pattern is repeated for other important preventive health care, such as cancer screening.
A 3-step plan to meet patients’ needs
The federal government should do three things to close these gaps in preventive care.
First, the government should make Primary Health Networks (PHNs) responsible for reducing them. PHNs, the regional bodies responsible for improving primary care, should share data with GPs and step in to boost uptake in communities that are missing out.
Second, the government should extend its MyMedicare reforms. MyMedicare gives general practices flexible funding to care for patients who live in residential aged care or who visit hospital frequently. That approach should be expanded to all patients, with more funding for poorer and sicker patients. That will give GP clinics time to advise patients about preventive health, including COVID vaccines and antivirals, before they get sick.
Third, team-based pharmacist prescribing should be introduced. Then pharmacists could quickly dispense antivirals for patients if they have a prior agreement with the patient’s GP. It’s an approach that would also work for medications for chronic diseases, such as cardiovascular disease.
COVID antivirals, unlike vaccines, have been keeping up with new variants without the need for updates. If a new and more harmful variant emerges, or when a new pandemic hits, governments should have these systems in place to make sure everyone who needs treatment can get it fast.
In the meantime, fairer access to care will help close the big and persistent gaps in health between different groups of Australians.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Relieve GERD and Acid Reflux with Stretches and Exercises
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Looking for relief from GERD or acid reflux? Today we’re featuring an amazing video by Dr. Jo, packed with stretches and exercises designed to ease those symptoms.
Here’s a quick rundown, in case you don’t have time to watch the whole video.
If you’re not familiar with GERD, you can find our simple explanation of GERD here. Or, if you’re on the other end of the spectrum and want to do a deeper dive on the topic, we reviewed a great book on the topic).
1. Mobilize Your SEM Muscle
The sternocleidomastoid (SEM) muscle, if tight, can aggravate acid reflux. Dr. Jo shows how to gently mobilize this muscle by turning your head while holding the SEM in place. It’s simple but effective.
2. Portrait Pose Stretch
Stretch out that SEM with the Portrait Pose. Place your hand on your collarbone, turn your head away, side bend, and look up. Hold for 30 seconds. You’ll feel the tension melting away.
3. Seated Cat-Cow Motion
Open up your stomach area with this easy exercise. Sit down, roll your body forward, arch your back (Cow), then curl your spine and tuck your chin (Cat). Alternate for 30 seconds and feel the difference.
4. Quadruped Cat-Cow with Breathing
Similar to the seated cat-cow, the quadruped cat-cow focuses on flexing the lower spine whilst on all fours. Bonus tip: focus on deep belly breathing during the exercise. This helps improve digestion and ease reflux symptoms.
5. Exaggerated Pelvic Tilt
Lie on your back and tilt your pelvis back and forth. This loosens up the abdominal area and helps everything flow better.
6. Trunk Rotation
Lie down, bend your knees, and rotate them to one side. Hold for 30 seconds, then switch sides. It’s a great way to relax and stretch your abdominal muscles.
We know this is a quick overview (sorry if it seems rushed!), but if you have a few more minutes on your hand you can watch the whole video below.
Feel better soon! And if you have any favorite tips or videos to share, email us at 10almonds.
Share This Post
-
How Are You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Answering The Most Difficult Question: How Are You?
Today’s feature is aimed at helping mainly two kinds of people:
- “I have so many emotions that I don’t always know what to do with them”
- “What is an emotion, really? I think I felt one some time ago”
So, if either those describe you and/or a loved one, read on…
Alexithymia
Alexi who? Alexithymia is an umbrella term for various kinds of problems with feeling emotions.
That could be “problems feeling emotions” as in “I am unable to feel emotions” or “problems feeling emotions” as in “feeling these emotions is a problem for me”.
It is most commonly used to refer to “having difficulty identifying and expressing emotions”.
There are a lot of very poor quality pop-science articles out there about it, but here’s a decent one with good examples and minimal sensationalist pathologization:
Alexithymia Might Be the Reason It’s Hard to Label Your Emotions
A somatic start
Because a good level of self-awareness is critical for healthy emotional regulation, let’s start there. We’ll write this in the first person, but you can use it to help a loved one too, just switching to second person:
Simplest level first:
Are my most basic needs met right now? Is this room a good temperature? Am I comfortable dressed the way I am? Am I in good physical health? Am I well-rested? Have I been fed and watered recently? Does my body feel clean? Have I taken any meds I should be taking?
Note: If the answer is “no”, then maybe there’s something you can do to fix that first. If the answer is “no” and also you can’t fix the thing for some reason, then that’s unfortunate, but just recognize it anyway for now. It doesn’t mean the thing in question is necessarily responsible for how you feel, but it’s good to check off this list as a matter of good practice.
Bonus question: it’s cliché, but if applicable… What time of the month is it? Because while hormonal mood swings won’t create moods out of nothing, they sure aren’t irrelevant either and should be listened to too.
Bodyscanning next
What do you feel in each part of your body? Are you clenching your jaw? Are your shoulders tense? Do you have a knot in your stomach? What are your hands doing? How’s your posture? What’s your breathing like? How about your heart? What are your eyes doing?
Your observations at this point should be neutral, by the way. Not “my posture is terrible”, but “my posture is stooped”, etc. Much like in mindfulness meditation, this is a time for observing, not for judging.
Narrowing it down
Now, like a good scientist, you have assembled data. But what does the data mean for your emotions? You may have to conduct some experiments to find out.
Thought experiments: what calls to you? What do you feel like doing? Do you feel like curling up in a ball? Breaking something? Taking a bath? Crying?
Maybe what calls to you, or what you feel like doing, isn’t something that’s possible for you to do. This is often the case with anxiety, for example, and perhaps also guilt. But whatever calls to you, notice it, reflect on it, and if it’s something that your conscious mind considers reasonable and safe for you to do, you can even try doing it.
Your body is trying to help you here, by the way! It will try (and usually succeed) to give you a little dopamine spike when you anticipate doing the thing it wants you to do. Warning: it won’t always be right about what’s best for you, so do still make your own decisions about whether it is a good idea to safely do it.
Practical experiments: whether you have a theory or just a hypothesis (if you have neither make up a hypothesis; that is also what scientists do), you can also test it:
If in the previous step you identified something you’d like to do and are able to safely do it, now is the time to try it. If not…
- Find something that is likely to (safely) tip you into emotional expression, ideally, in a cathartic way. But, whatever you can get is good.
- Music is great for this. What songs (or even non-lyrical musical works) make you sad, happy, angry, energized? Try them.
- Literature and film can be good too, albeit they take more time. Grab that tear-jerker or angsty rage-fest, and see if it feels right.
- Other media, again, can be completely unrelated to the situation at hand, but if it evokes the same emotion, it’ll help you figure out “yes, this is it”.
- It could be a love letter or a tax letter, it could be an outrage-provoking news piece or some nostalgic thing you own.
Ride it out, wherever it takes you (safely)
Feelings feel better felt. It doesn’t always seem that way! But, really, they are.
Emotions, just like physical sensations, are messengers. And when a feeling/sensation is troublesome, one of the best ways to get past it is to first fully listen to it and respond accordingly.
- If your body tells you something, then it’s good to acknowledge that and give it some reassurance by taking some action to appease it.
- If your emotions are telling you something, then it’s good to acknowledge that and similarly take some action to appease it.
There is a reason people feel better after “having a good cry”, or “pounding it out” against a punchbag. Even stress can be dealt with by physically deliberately tensing up and then relaxing that tension, so the body thinks that you had a fight and won and can relax now.
And when someone is in a certain (not happy) mood and takes (sometimes baffling!) actions to stay in that mood rather than “snap out of it”, it’s probably because there’s more feeling to be done before the body feels heard. Hence the “ride it out if you safely can” idea.
How much feeling is too much?
While this is in large part a subjective matter, clinically speaking the key question is generally: is it adversely affecting daily life to the point of being a problem?
For example, if you have to spend half an hour every day actively managing a certain emotion, that’s probably indicative of something unusual, but “unusual” is not inherently pathological. If you’re managing it safely and in a way that doesn’t negatively affect the rest of your life, then that is generally considered fine, unless you feel otherwise about it.
If you do think “I would like to not think/feel this anymore”, then there are tools at your disposal too:
- How To Manage Chronic Stress
- How To Set Anxiety Aside
- How To Stop Revisiting Those Memories
- How To Stay Alive (When You Really Don’t Want To)
Take care!
Share This Post
-
5 Self-Care Trends That Are Actually Ruining Your Mental Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ok, some of these are trends; some are more perennial to human nature. For example, while asceticism is not a new idea, the “dopamine detox” is, and “bed rotting” is not a trend that this writer has seen recommended anywhere, but on the other hand, there are medieval illustrations of it—there was no Netflix in sight in the medieval illustrations, but perhaps a label diagnosing it as “melancholy”, for example.
So without further ado, here are five things to not do…
Don’t fall into these traps
The 5 things to watch out for are:
- Toxic positivity: constantly promoting positivity regardless of the reality of a situation can shame or invalidate genuine emotions, preventing people from processing their real feelings and leading to negative mental health outcomes—especially if it involves a “head in sand” approach to external problems as well as internal ones (because then those problems will never actually get dealt with).
- Self-indulgence: excessive focus on personal desires can make you more self-centered, less disciplined, and ultimately dissatisfied, which hinders personal growth and mental wellness.
- Bed rotting: spending prolonged time in bed for relaxation or entertainment can decrease motivation, productivity, and lead to (or worsen) depression rather than promoting genuine rest and rejuvenation.
- Dopamine detox: abstaining from pleasurable activities to “reset” the brain simply does not work and can lead to loneliness, boredom, and worsen mental health, especially when done excessively.
- Over-reliance on self-help: consuming too much self-help content or relying on material possessions for well-being can lead to information overload, unrealistic expectations, and the constant need for self-fixing, rather than fostering self-acceptance and authentic growth. Useful self-help can be like taking your car in for maintenance—counterproductive self-help is more like having your car always in for maintenance and never actually on the road.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read, and yes these are pretty much one-for-one with the 5 items above, doing a deeper dive into each in turn,
- How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
- Self-Care That’s Not Just Self-Indulgence
- The Mental Health First-Aid That You’ll Hopefully Never Need
- The Dopamine Myth
- Behavioral Activation Against Depression & Anxiety
Take care!
Share This Post
Related Posts
-
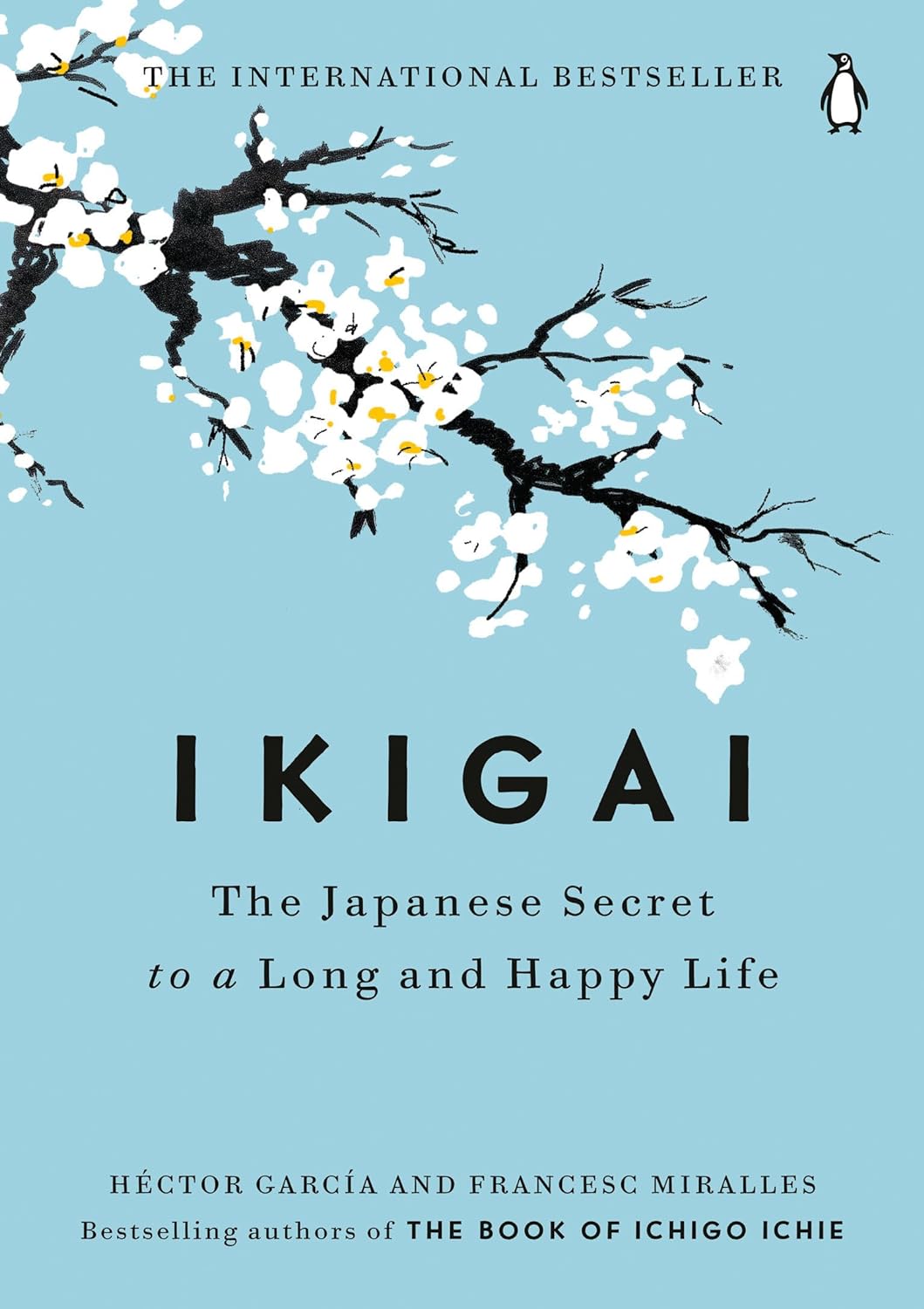
Ikigai – by Héctor García and Francesc Miralles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ikigai is the Japanese term for what in English we often call “raison d’être”… in French, because English is like that.
But in other words: ikigai is one’s purpose in life, one’s reason for living.
The authors of this work spend some chapters extolling the virtues of finding one’s ikigai, and the health benefits that doing so can convey. It is, quite clearly, an important and relevant factor.
The rest of the book goes beyond that, though, and takes a holistic look at why (and how) healthy longevity is enjoyed by:
- Japanese people in general,
- Okinawans in particular,
- Residents of Okinawa’s “blue zone” village with the highest percentage of supercentenarians, most of all.
Covering considerations from ikigai to diet to small daily habits to attitudes to life, we’re essentially looking at a blueprint for healthy longevity.
For a book whose title and cover suggests a philosophy-heavy content, there’s a lot of science in here too, by the way! From microbiology to psychiatry to nutrition science to cancer research, this book covers all bases.
In short: this book gives a lot of good science-based suggestions for adjustments we can make to our lives, without moving to an Okinawan village!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Ways To Make Your Smoothie Blood Sugar Friendly (Avoid the Spike!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds, we are often saying “eat whole fruit; don’t drink your calories”. Whole fruit is great for blood sugars; fruit juices and many smoothies on the other hand, not so much. Especially juices, being near-completely or perhaps even completely stripped of fiber, but even smoothies have had a lot of the fiber broken down and are still a liquid, meaning they are very quickly and easily digestible, and thus their sugars (whatever carbs are in there) can just zip straight into your veins.
However, there are ways to mitigate this…
Slow it down
The theme here is “give the digestive process something else to do”; some things are more quickly and easily digestible than others, and if it’s working on breaking down some of the slower things, it’s not waving sugars straight on through; they have to wait their turn.
To that end, recommendations include:
- Full-fat Greek yogurt which provides both protein and fat, helping to slow down the absorption of sugar. Always choose unsweetened versions to avoid added sugars, though!
- Coconut milk (canned) which is low in sugar and carbs, high in fat. This helps reduce blood sugar spikes, as she found through personal experimentation too.
- Avocado which is rich in healthy fats that help stabilize blood sugar. As a bonus, it blends well into smoothies without affecting the taste much.
- Coconut oil which contains medium-chain triglycerides (MCTs) that are quickly absorbed for energy without involving glucose, promoting fat-burning and reducing blood sugar spikes.
- Collagen powder which is a protein that helps lower blood sugar spikes while also supporting muscle growth, skin, and joints.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reduce Your Stroke Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❝Each year in the U.S., over half a million people have a first stroke; however, up to 80% of strokes may be preventable.❞
~ American Stroke Association
Source: New guideline: Preventing a first stroke may be possible with screening, lifestyle changes
So, what should we do?
Some of the risk factors are unavoidable or not usefully avoidable, like genetic predispositions and old age, respectively (i.e. it is possible to avoid old age—by dying young, which is not a good approach).
Some of the risk factors are avoidable. Let’s look at the most obvious first:
You cannot drink to your good health
While overall, the World Health Organization has declared that “the only safe amount of alcohol is zero”, when it comes to stroke risk specifically, it seems that low consumption is not associated with stroke, while moderate to high consumption is associated with a commensurately increased risk of stroke:
Alcohol Intake as a Risk Factor for Acute Stroke
Note: there are some studies out there that say that a low to moderate consumption may decrease the risk compared to zero consumption. However, any such study that this writer has seen has had the methodological flaw of not addressing why those who do not drink alcohol, do not drink it. In many cases, someone who drinks no alcohol at all does so because either a) it would cause problems with some medication(s) they are taking, or b) they used to drink heavily, and quit. In either case, their reasons for not drinking alcohol may themselves be reasons for an increased stroke risk—not the lack of alcohol itself.
Smoke now = stroke later
This one is straightforward; smoking is bad for pretty much everything, and that includes stroke risk, as it’s bad for your heart and brain both, increasing stroke risk by 200–400%:
Smoking and stroke: the more you smoke the more you stroke
So, the advice here of course is: don’t smoke
Diet matters
The American Stroke Association’s guidelines recommend, just for a change, the Mediterranean Diet. This does not mean just whatever is eaten in the Mediterranean region though, and there are specifically foods that are included and excluded, and the ratios matter, so here’s a run-down of what the Mediterranean Diet does and doesn’t include:
The Mediterranean Diet: What Is It Good For? ← what isn’t it good for?!
You can outrun stroke
Or out-walk it; that’s fine too. Most important here is frequency of exercise, more than intensity. So basically, getting those 150 minutes moderate exercise per week as a minimum.
See also: The Doctor Who Wants Us To Exercise Less & Move More
Which is good, because it means we can get a lot of exercise in that doesn’t feel like “having to do” exercise, for example:
Do You Love To Go To The Gym? No? Enjoy These “No-Exercise Exercises”!
Your brain needs downtime too
Your brain (and your heart) both need you to get good regular sleep:
Sleep Disorders in Stroke: An Update on Management
We sometimes say that “what’s good for your heart is good for your brain” (because the heart feeds the brain, and also ultimately clears away detritus), and that’s true here too, so we might also want to prioritize sleep regularity over other factors, even over duration:
How Regularity Of Sleep Can Be Even More Important Than Duration ← this is about adverse cardiovascular events, including ischemic stroke
Keep on top of your blood pressure
High blood pressure is a very modifiable risk factor for stroke. Taking care of the above things will generally take care of this, especially the DASH variation of the Mediterranean diet:
Hypertension: Factors Far More Relevant Than Salt
However, it’s still important to actually check your blood pressure regularly, because sometimes an unexpected extra factor can pop up for no obvious reason. As a bonus, you can do this improved version of the usual blood pressure test, still using just a blood pressure cuff:
Try This At Home: ABI Test For Clogged Arteries
Consider GLP-1 receptor agonists (or…)
GLP-1 receptor agonists (like Ozempic et al.) seem to have cardioprotective and neuroprotective (thus: anti-stroke) activity independent of their weight loss benefits:
Of course, GLP-1 RAs aren’t everyone’s cup of tea, and they do have their downsides (including availability, cost, and the fact benefits reverse themselves if you stop taking them), so if you want a similar effect from a natural approach, there are some foods that work on the body’s incretin responses in the same way as GLP-1 RAs do:
5 Foods That Naturally Mimic The “Ozempic Effect”
Better to know sooner rather than too late
Rather than waiting until one half of our face is drooping to know that there was a stroke risk, here are things to watch out for to know about it before it’s too late:
6 Signs Of Stroke (One Month In Advance)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: