Feel Better In 5 – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve featured Dr. Rangan Chatterjee before, and here’s a great book of his.
The premise is a realistic twist on a classic, the classic being “such-and-such, in just 5 minutes per day!”
In this case, Dr. Chatterjee offers many lifestyle interventions that each take just 5 minutes, with the idea that you implement 3 of them per day (your choice which and when), and thus gradually build up healthy habits. Of course, once things take as habits, you’ll start adding in more, and before you know it, half your lifestyle has changed for the better.
Which, you may be thinking “my lifestyle’s not that bad”, but if you improve the health outcomes of, say, 20 areas of your life by just a few percent each, you know much better health that adds up to? We’ll give you a clue: it doesn’t add up, it compounds, because each improves the other too, for no part of the body works entirely in isolation.
And Dr. Chatterjee does tackle the body systematically, by the way; interventions for the gut, heart, brain, and so on.
As for what these interventions look like; it is very varied. One might be a physical exercise; another, a mental exercise; another, a “make this health 5-minute thing in the kitchen”, etc, etc.
Bottom line: this is the most supremely easy of easy-ins to healthier living, whatever your starting point—because even if you’re doing half of these interventions, chances are you aren’t doing the other half, and the idea is to pick and choose how and when you adopt them in any case, just picking three 5-minute interventions each day with no restrictions. In short, a lot of value to had here when it comes to real changes to one’s serious measurable health.
Click here to check out Feel Better In 5, and indeed feel better in 5!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blood and Water
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q&A with the 10almonds Team
Q: I really loved the information about macular degeneration! I was wondering if you have any other advice about looking after eye health?
A: We may well do a full feature on it sometime! Meanwhile, some top tips include:
- Eat your greens (as you know from this last Tuesday’s edition of 10almonds)!
- Exercise! Generally. We’re not talking about eye exercises here, we’re talking about exercises that will support:
- Healthy heart rate
- Healthy blood pressure
- Healthy blood oxygenation
- Healthy blood sugar levels
- Healthy blood flow in general (so keep hydrated too! There’s a reason phlebotomists ask you to be well-hydrated before they take blood)
Eye health is a good indicator for a lot of other things, and that’s because whether or not the eyes are the window to your soul, they’re definitely the window to what your blood’s like, and that affects (and is affected by) so many other things.
- On that note, don’t smoke!
- Protect your eyes physically, too. This means:
- UV-blocking sunglasses when appropriate
- Protective eye-wear when appropriate
You think safety glasses are for laboratories and construction sites, then you go and do comparable tasks in your home? Your eyes are just as damageable in your kitchen or garden as they would be in a lab or workshop.
Some bits and bobs that can help:
- Safety sunglasses! Because a thing can do two jobs (useful in the garden now the days are brightening up!)
- Pulse oximeter! Check your own heart rate, pulse strength, and blood oxygenation at home!
- Blood pressure monitor! Because it’s so important for a lot of things and you really should have one.
Share This Post
-
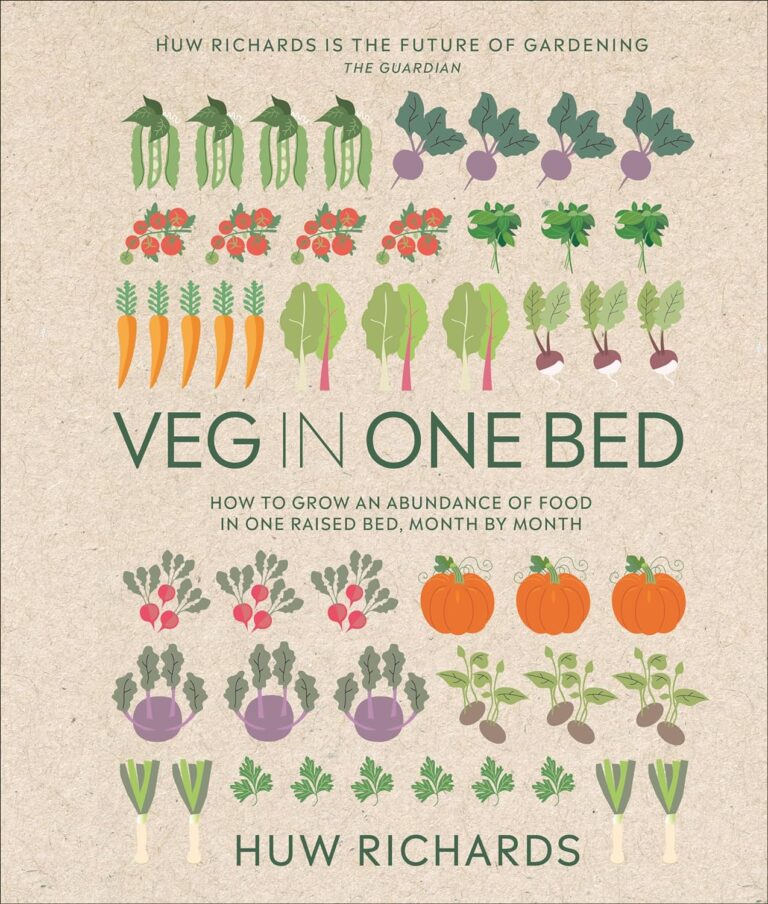
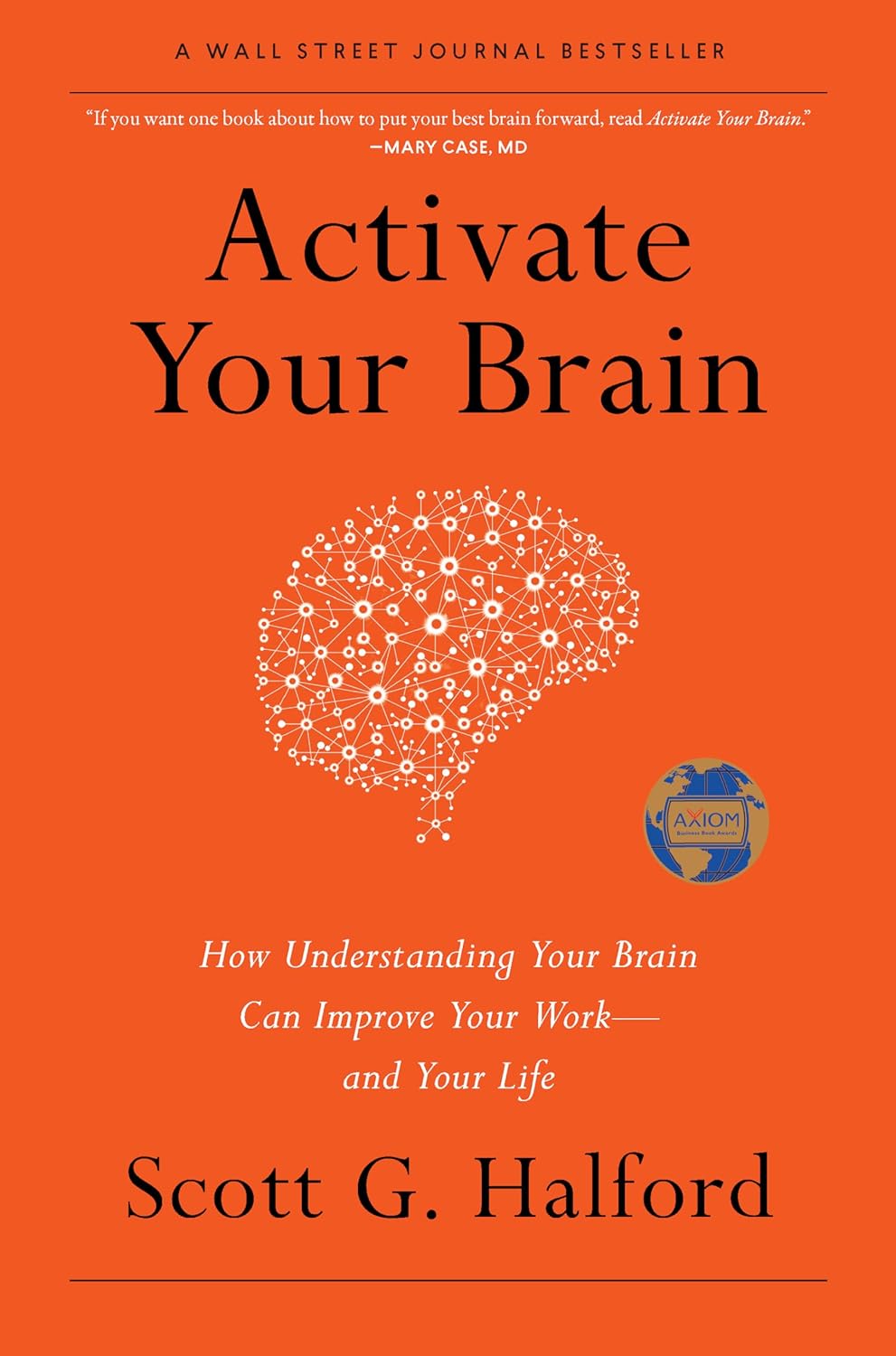
Activate Your Brain – by Scott G. Halford
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed a number of “improve your brain health” books over time, and this one’s quite different. How?
Most of the books we’ve reviewed have been focused on optimizing diet and exercise for brain health with a nod to other factors… This one focuses more on those other factors.
While this book does reference a fair bit of hard science, much of it is written more like a pop psychology book. As a result, most of the actionable advices, of which there are many, pertain to cognitive and behavioral adjustments.
And no, this is not a book of Cognitive Behavioral Therapy. It just happened to also address those two aspects.
We learn, for example, how our neurochemistry influences us—but also how we can influence our neurochemistry.
We also learn the oft-neglected (in other books!) social factors that influence brain health. Not just for our happiness, but for our productivity and peak cognitive performance too. Halford talks us through optimizing these such that we and those around us all get to enjoy the best brain benefits available to each of us.
The format of the book is that each chapter explains what you need to know for a given “activation” as the author calls it, and then an exercise to try out. With fifteen such chapters, every reader is bound to find at least something new.
Bottom line: if you want to grease those synapses in more ways than just eating some nuts and berries and getting good sleep and exercise, this book is a great resource.
Click here to check out “Activate Your Brain” and find your next level of cognitive performance!
Share This Post
-
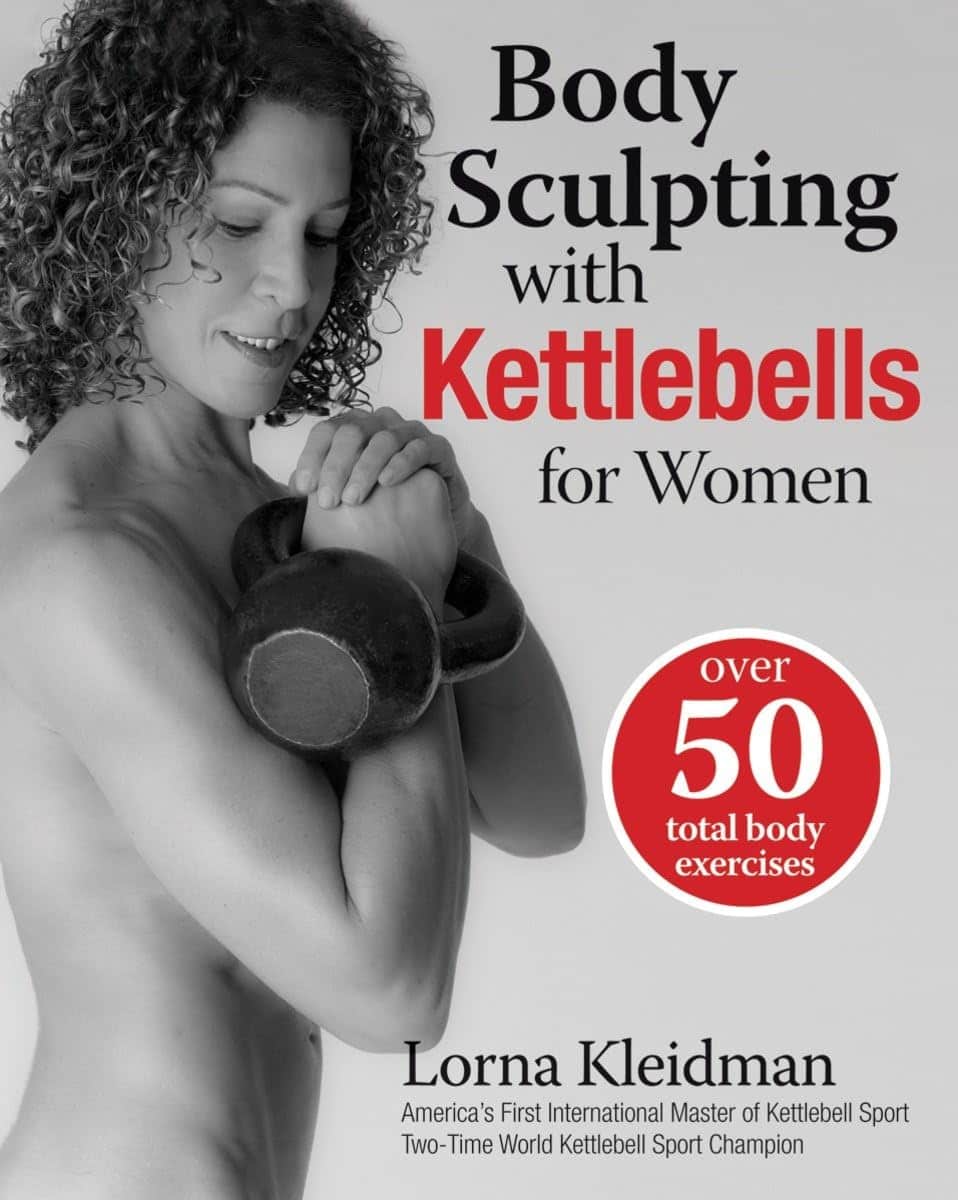
Body Sculpting with Kettlebells for Women – by Lorna Kleidman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those of us who are more often lifting groceries or pots and pans than bodybuilding trophies, kettlebells provide a way of training functional strength. This book does (as per the title) offer both sides of things—the body sculpting, and thebody maintenance free from pain and injury.
Kleidman first explains the basics of kettlebell training, and how to get the most from one’s workouts, before discussing what kinds of exercises are best for which benefits, and finally moving on to provide full exercise programs.
The exercise programs themselves are fairly comprehensive without being unduly detailed, and give a week-by-week plan for getting your body to where you want it to be.
The style is fairly personal and relaxed, while keeping things quite clear—the photographs are also clear, though if there’s a weakness here, it’s that we don’t get to see which muscles are being worked in the same as we do when there’s an illustration with a different-colored part to show that.
Bottom line: if you’re looking for an introductory course for kettlebell training that’ll take you from beginner through to the “I now know what I’m doing and can take it from here, thanks” stage.
Click here to check out Body Sculpting With Kettlebells For Women, and get sculpting!
Share This Post
Related Posts
-
America Worries About Health Costs — And Voters Want to Hear From Biden and Republicans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
President Joe Biden is counting on outrage over abortion restrictions to help drive turnout for his reelection. Former President Donald Trump is promising to take another swing at repealing Obamacare.
But around America’s kitchen tables, those are hardly the only health topics voters want to hear about in the 2024 campaigns. A new KFF tracking poll shows that health care tops the list of basic expenses Americans worry about — more than gas, food, and rent. Nearly 3 in 4 adults — and majorities of both parties — say they’re concerned about paying for unexpected medical bills and other health costs.
“Absolutely health care is something on my mind,” Rob Werner, 64, of Concord, New Hampshire, said in an interview at a local coffee shop in January. He’s a Biden supporter and said he wants to make sure the Affordable Care Act, also known as Obamacare, is retained and that there’s more of an effort to control health care costs.
The presidential election is likely to turn on the simple question of whether Americans want Trump back in the White House. (Nikki Haley, the former South Carolina governor and U.S. ambassador to the United Nations, remained in the race for the Republican nomination ahead of Super Tuesday, though she had lost the first four primary contests.) And neither major party is basing their campaigns on health care promises.
But in the KFF poll, 80% of adults said they think it’s “very important” to hear presidential candidates talk about what they’d do to address health care costs — a subject congressional and state-level candidates can also expect to address.
“People are most concerned about out-of-pocket expenses for health care, and rightly so,” said Andrea Ducas, vice president of health policy at the Center for American Progress, a Washington, D.C.-based progressive think tank.
Here’s a look at the major health care issues that could help determine who wins in November.
Abortion
Less than two years after the Supreme Court overturned the constitutional right to an abortion, it is shaping up to be the biggest health issue in this election.
That was also the case in the 2022 midterm elections, when many voters rallied behind candidates who supported abortion rights and bolstered Democrats to an unexpectedly strong showing. Since the Supreme Court’s decision, voters in six states — including Kansas, Kentucky, and Ohio, where Republicans control the legislatures — have approved state constitutional amendments protecting abortion access.
Polls show that abortion is a key issue to some voters, said Robert Blendon, a public opinion researcher and professor emeritus at the Harvard T.H. Chan School of Public Health. He said up to 30% across the board see it as a “personal” issue, rather than policy — and most of those support abortion rights.
“That’s a lot of voters, if they show up and vote,” Blendon said.
Proposals to further protect — or restrict — abortion access could drive voter turnout. Advocates are working to put abortion-related measures on the ballot in such states as Arizona, Florida, Missouri, and South Dakota this November. A push in Washington toward a nationwide abortion policy could also draw more voters to the polls, Blendon said.
A surprise ruling by the Alabama Supreme Court in February that frozen embryos are children could also shake up the election. It’s an issue that divides even the anti-abortion community, with some who believe that a fertilized egg is a unique new person deserving of full legal rights and protections, and others believing that discarding unused embryos as part of the in vitro fertilization process is a morally acceptable way for couples to have children.
Pricey Prescriptions
Drug costs regularly rank high among voters’ concerns.
In the latest tracking poll, more than half — 55% — said they were very worried about being able to afford prescription drugs.
Biden has tried to address the price of drugs, though his efforts haven’t registered with many voters. While its name doesn’t suggest landmark health policy, the Inflation Reduction Act, or IRA, which the president signed in August 2022, included a provision allowing Medicare to negotiate prices for some of the most expensive drugs. It also capped total out-of-pocket spending for prescription drugs for all Medicare patients, while capping the price of insulin for those with diabetes at $35 a month — a limit some drugmakers have extended to patients with other kinds of insurance.
Drugmakers are fighting the Medicare price negotiation provision in court. Republicans have promised to repeal the IRA, arguing that forcing drugmakers to negotiate lower prices on drugs for Medicare beneficiaries would amount to price controls and stifle innovation. The party has offered no specific alternative, with the GOP-led House focused primarily on targeting pharmacy benefit managers, the arbitrators who control most Americans’ insurance coverage for medicines.
Costs of Coverage
Health care costs continue to rise for many Americans. The cost of employer-sponsored health plans have hit new highs in the past few months, raising costs for employers and workers alike. Experts have attributed the increase to high demand and expensive prices for certain drugs and treatments, notably weight loss drugs, as well as to medical inflation.
Meanwhile, the ACA is popular. The KFF poll found that more adults want to see the program expanded than scaled back. And a record 21.3 million people signed up for coverage in 2024, about 5 million of them new customers.
Enrollment in Republican-dominated states has grown fastest, with year-over-year increases of 80% in West Virginia, nearly 76% in Louisiana, and 62% in Ohio, according to the Centers for Medicare & Medicaid Services.
Public support for Obamacare and record enrollment in its coverage have made it politically perilous for Republicans to pursue the law’s repeal, especially without a robust alternative. That hasn’t stopped Trump from raising that prospect on the campaign trail, though it’s hard to find any other Republican candidate willing to step out on the same limb.
“The more he talks about it, the more other candidates have to start answering for it,” said Jarrett Lewis, a partner at Public Opinion Strategies, a GOP polling firm.
“Will a conversation about repeal-and-replace resonate with suburban women in Maricopa County?” he said, referring to the populous county in Arizona known for being a political bellwether. “I would steer clear of that if I was a candidate.”
Biden and his campaign have pounced on Trump’s talk of repeal. The president has said he wants to make permanent the enhanced premium subsidies he signed into law during the pandemic that are credited with helping to increase enrollment.
Republican advisers generally recommend that their candidates promote “a market-based system that has the consumer much more engaged,” said Lewis, citing short-term insurance plans as an example. “In the minds of Republicans, there is a pool of people that this would benefit. It may not be beneficial for everyone, but attractive to some.”
Biden and his allies have criticized short-term insurance plans — which Trump made more widely available — as “junk insurance” that doesn’t cover care for serious conditions or illnesses.
Entitlements Are Off-Limits
Both Medicaid and Medicare, the government health insurance programs that cover tens of millions of low-income, disabled, and older people, remain broadly popular with voters, said the Democratic pollster Celinda Lake. That makes it unlikely either party would pursue a platform that includes outright cuts to entitlements. But accusing an opponent of wanting to slash Medicare is a common, and often effective, campaign move.
Although Trump has said he wouldn’t cut Medicare spending, Democrats will likely seek to associate him with other Republicans who support constraining the program’s costs. Polls show that most voters oppose reducing any Medicare benefits, including by raising Medicare’s eligibility age from 65. However, raising taxes on people making more than $400,000 a year to shore up Medicare’s finances is one idea that won strong backing in a recent poll by The Associated Press and NORC Center for Public Affairs Research.
Brian Blase, a former Trump health adviser and the president of Paragon Health Institute, said Republicans, if they win more control of the federal government, should seek to lower spending on Medicare Advantage — through which commercial insurers provide benefits — to build on the program’s efficiencies and ensure it costs taxpayers less than the traditional program.
So far, though, Republicans, including Trump, have expressed little interest in such a plan. Some of them are clear-eyed about the perils of running on changing Medicare, which cost $829 billion in 2021 and is projected to consume nearly 18% of the federal budget by 2032.
“It’s difficult to have a frank conversation with voters about the future of the Medicare program,” said Lewis, the GOP pollster. “More often than not, it backfires. That conversation will have to happen right after a major election.”
Addiction Crisis
Many Americans have been touched by the growing opioid epidemic, which killed more than 112,000 people in the United States in 2023 — more than gun deaths and road fatalities combined. Rural residents and white adults are among the hardest hit.
Federal health officials have cited drug overdose deaths as a primary cause of the recent drop in U.S. life expectancy.
Republicans cast addiction as largely a criminal matter, associating it closely with the migration crisis at the U.S. southern border that they blame on Biden. Democrats have sought more funding for treatment and prevention of substance use disorders.
“This affects the family, the neighborhood,” said Blendon, the public opinion researcher.
Billions of dollars have begun to flow to states and local governments from legal settlements with opioid manufacturers and retailers, raising questions about how to best spend that money. But it isn’t clear that the crisis, outside the context of immigration, will emerge as a campaign issue.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tuna Steak with Protein Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Yes, it’s protein on protein today, and it’s all healthy.
You will need (per person)
- 1 tuna steak
- 1 400g/12oz can mixed beans, drained & rinsed
- 1 tsp capers
- 2 tsp black pepper, coarse ground
- 1 red chili, chopped
- 1 lime, cut into wedges
- ½ tsp white wine vinegar
- Extra virgin olive oil, for cooking
- Garnish: chopped parsley
Method
(we suggest you read everything at least once before doing anything)
1) Put the beans in a bowl, mixing in the capers, vinegar, and 1 tsp of the black pepper
2) Gently rub a little olive oil onto each side of the tuna steak, and season with the remainder of the black pepper (as in, the other tsp, not the rest of what you have in the house).
3) Heat a ridged grill pan until hot, and then cook the tuna for around 3 minutes on each side. Do not jiggle it! Do not slide it, and definitely do not stir it. Just gently turn it over when necessary. The edges should be cooked, and the inside should still be pink (it’s easy to forget when it comes from a can, but remember tuna is usually eaten raw)
4) Serve, sprinkling with the chopped chili and garnishing with the parsley. The lime wedges go on the side for squeezing at the table.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Protein: How Much Do We Need, Really?
- Salmon vs Tuna – Which is Healthier?
- Cilantro vs Parsley – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vibration Plate, Review After 6 Months: Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is it push-button exercise, or an expensive fad, or something else entirely? Robin, from “The Science of Self-Care”, has insights:
Science & Experience
According to the science (studies cited in the video and linked-to in the video description, underneath it on YouTube), vibration therapy does have some clear benefits, namely:
- Bone health (helps with bone density, particularly beneficial for postmenopausal women)
- Muscle recovery (reduces lactate levels, aiding faster recovery)
- Joint health (reduces pain and improves function in osteoarthritis patients)
- Muscle stimulation (helps older adults maintain muscle mass)
- Cognitive function (due to increased blood flow to the brain)
And from her personal experience, the benefits included:
- Improved recovery after exercise, reducing muscle soreness and stiffness
- Reduced back pain and improved posture (not surprising, given the need for stabilizing muscles when using one of these)
- Better circulation and (likely resulting from same) skin clarity
She did not, however, notice:
- Any reduction in cellulite
- Any change in body composition (fat loss or muscle gain)
For a deeper look into these things and more, plus a demonstration of how the machine actually operates, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: