Non-Sleep Deep Rest: A Neurobiologist’s Take
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to get many benefits of sleep, while awake!
Today we’re talking about Dr. Andrew Huberman, a neuroscientist and professor in the department of neurobiology at Stanford School of Medicine.
He’s also a popular podcaster, and as his Wikipedia page notes:
❝In episodes lasting several hours, Huberman talks about the state of research in a specific topic, both within and outside his specialty❞
Today, we won’t be taking hours, and we will be taking notes from within his field of specialty (neurobiology). Specifically, in this case:
Non-Sleep Deep Rest (NSDR)
What is it? To quote from his own dedicated site on the topic:
❝What is NSDR (Yoga Nidra)? Non-Sleep Deep Rest, also known as NSDR, is a method of deep relaxation developed by Dr. Andrew Huberman, a neuroscientist at Stanford University School of Medicine.
It’s a process that combines controlled breathing and detailed body scanning to bring you into a state of heightened awareness and profound relaxation. The main purpose of NSDR is to reduce stress, enhance focus, and improve overall well-being.❞
While it seems a bit bold of Dr. Huberman to claim that he developed yoga nidra, it is nevertheless reassuring to get a neurobiologist’s view on this:
How it works, by science
Dr. Huberman says that by monitoring EEG readings during NSDR, we can see how the brain slows down. Measurably!
- It goes from an active beta range of 13–30 Hz (normal waking) to a conscious meditation state of an alpha range of 8–13 Hz.
- However, with practice, it can drop further, into a theta range of 4–8 Hz.
- Ultimately, sustained SSDR practice can get us to 0.5–3 Hz.
This means that the brain is functioning in the delta range, something that typically only occurs during our deepest sleep.
You may be wondering: why is delta lower than theta? That’s not how I remember the Greek alphabet being ordered!
Indeed, while the Greek alphabet goes alpha beta gamma delta epsilon zeta eta theta (and so on), the brainwave frequency bands are:
- Gamma = concentrated focus, >30 Hz
- Beta = normal waking, 13–30 Hz
- Alpha = relaxed state, 8–13 Hz
- Theta = light sleep, 4–8 Hz
- Delta = deep sleep, 1–4 Hz
Source: Sleep Foundation ← with a nice infographic there too
NSDR uses somatic cues to engage our parasympathetic nervous system, which in turn enables us to reach those states. The steps are simple:
- Pick a time and place when you won’t be disturbed
- Lie on your back and make yourself comfortable
- Close your eyes as soon as you wish, and now that you’ve closed them, imagine closing them again. And again.
- Slowly bring your attention to each part of your body in turn, from head to toe. As your attention goes to each part, allow it to relax more.
- If you wish, you can repeat this process for another wave, or even a third.
- Find yourself well-rested!
Note: this engagement of the parasympathetic nervous system and slowing down of brain activity accesses restorative states not normally available while waking, but 10 minutes of NSDR will not replace 7–9 hours of sleep; nor will it give you the vital benefits of REM sleep specifically.
So: it’s an adjunct, not a replacement
Want to try it, but not sure where/how to start?
When you’re ready, let Dr. Huberman himself guide you through it in this shortish (10:49) soundtrack:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to try it, but not right now? Bookmark it for later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are you over 75? Here’s what you need to know about vitamin D
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Vitamin D is essential for bone health, immune function and overall wellbeing. And it becomes even more crucial as we age.
New guidelines from the international Endocrine Society recommend people aged 75 and over should consider taking vitamin D supplements.
But why is vitamin D so important for older adults? And how much should they take?
OPPO Find X5 Pro/Unsplash Young people get most vitamin D from the sun
In Australia, it is possible for most people under 75 to get enough vitamin D from the sun throughout the year. For those who live in the top half of Australia – and for all of us during summer – we only need to have skin exposed to the sun for a few minutes on most days.
The body can only produce a certain amount of vitamin D at a time. So staying in the sun any longer than needed is not going to help increase your vitamin D levels, while it will increase your risk of skin cancer.
But it’s difficult for people aged over 75 to get enough vitamin D from a few minutes of sunshine, so the Endocrine Society recommends people get 800 IU (international units) of vitamin D a day from food or supplements.
Why you need more as you age
This is higher than the recommendation for younger adults, reflecting the increased needs and reduced ability of older bodies to produce and absorb vitamin D.
Overall, older adults also tend to have less exposure to sunlight, which is the primary source of natural vitamin D production. Older adults may spend more time indoors and wear more clothing when outdoors.
As we age, our skin also becomes less efficient at synthesising vitamin D from sunlight.
The kidneys and the liver, which help convert vitamin D into its active form, also lose some of their efficiency with age. This makes it harder for the body to maintain adequate levels of the vitamin.
All of this combined means older adults need more vitamin D.
Deficiency is common in older adults
Despite their higher needs for vitamin D, people over 75 may not get enough of it.
Studies have shown one in five older adults in Australia have vitamin D deficiency.
In higher-latitude parts of the world, such as the United Kingdom, almost half don’t reach sufficient levels.
This increased risk of deficiency is partly due to lifestyle factors, such as spending less time outdoors and insufficient dietary intakes of vitamin D.
It’s difficult to get enough vitamin D from food alone. Oily fish, eggs and some mushrooms are good sources of vitamin D, but few other foods contain much of the vitamin. While foods can be fortified with the vitamin D (margarine, some milk and cereals), these may not be readily available or be consumed in sufficient amounts to make a difference.
In some countries such as the United States, most of the dietary vitamin D comes from fortified products. However, in Australia, dietary intakes of vitamin D are typically very low because only a few foods are fortified with it.
Why vitamin D is so important as we age
Vitamin D helps the body absorb calcium, which is essential for maintaining bone density and strength. As we age, our bones become more fragile, increasing the risk of fractures and conditions like osteoporosis.
Keeping bones healthy is crucial. Studies have shown older people hospitalised with hip fractures are 3.5 times more likely to die in the next 12 months compared to people who aren’t injured.
People over 75 often have less exposure to sunlight. Aila Images/Shutterstock Vitamin D may also help lower the risk of respiratory infections, which can be more serious in this age group.
There is also emerging evidence for other potential benefits, including better brain health. However, this requires more research.
According to the society’s systematic review, which summarises evidence from randomised controlled trials of vitamin D supplementation in humans, there is moderate evidence to suggest vitamin D supplementation can lower the risk of premature death.
The society estimates supplements can prevent six deaths per 1,000 people. When considering the uncertainty in the available evidence, the actual number could range from as many as 11 fewer deaths to no benefit at all.
Should we get our vitamin D levels tested?
The Endocrine Society’s guidelines suggest routine blood tests to measure vitamin D levels are not necessary for most healthy people over 75.
There is no clear evidence that regular testing provides significant benefits, unless the person has a specific medical condition that affects vitamin D metabolism, such as kidney disease or certain bone disorders.
Routine testing can also be expensive and inconvenient.
In most cases, the recommended approach to over-75s is to consider a daily supplement, without the need for testing.
You can also try to boost your vitamin D by adding fortified foods to your diet, which might lower the dose you need from supplementation.
Even if you’re getting a few minutes of sunlight a day, a daily vitamin D is still recommended.
Elina Hypponen, Professor of Nutritional and Genetic Epidemiology, University of South Australia and Joshua Sutherland, PhD Candidate – Nutrition and Genetic Epidemiology, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Gift Of Aging − by Dr. Elizabeth Eckstrom & Marcy Houle
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is, as you may gather from the title, a book about getting the most out of growing older, and doing it well.
Not all of it is positive though; some of it really is about avoiding, mitigating, or coping with the negatives that tend to come with aging.
The book is full of many (38) small self-contained chapters, so it’s well-suited to reading bit-by-bit, if so inclined. Essentially, it’s a collection of essays by the two authors, arranged into categories:
- Caring for your mind
- Caring for your body
- Caring for yourself and your family
- Caring for your soul
The first two sections are mostly self-explanatory; the third is largely about estate-planning of various kinds. The fourth is highly subjective, and/but not particularly religious, by the way. It’s largely an add-on to the “caring for your mind” mental health section, but now more specifically dealing with heavy topics such as the emotional side of mortality (as opposed to the previous section’s practical considerations of same), loss, and grief.
The style is the very low end of pop-science; facts (probably true ones; nothing seemed very contentious objectively) are stated with no sources, and there is no medical jargon that’s anything more complicated than you might find on a leaflet in a doctor’s waiting room.
Bottom line: this is a very opinion-filled book, so it’s worth reading with that in mind (i.e. their opinions may differ wildly from yours in some cases), but it’s largely informed opinions, so worth at least considering even in those cases. If nothing else, this book is certainly thought-provoking.
Click here to check out The Gift Of Aging, and enjoy the gift of aging!
Share This Post
-
What should I do if I can’t see a psychiatrist?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People presenting at emergency with mental health concerns are experiencing the longest wait times in Australia for admission to a ward, according to a new report from the Australasian College of Emergency Medicine.
But with half of New South Wales’ public psychiatrists set to resign next week after ongoing pay disputes – and amid national shortages in the mental health workforce – Australians who rely on psychiatry support may be wondering where else to go.
If you can’t get in to see a psychiatrist and you need help, there are some other options. However in an emergency, you should call 000.
Why do people see a psychiatrist?
Psychiatrists are doctors who specialise in mental health and can prescribe medication.
People seek or require psychiatry support for many reasons. These may include:
- severe depression, including suicidal thoughts or behaviours
- severe anxiety, panic attacks or phobias
- post-traumatic stress disorder (PTSD)
- eating disorders, such as anorexia or bulimia
- attention deficit hyperactivity disorder (ADHD).
Psychiatrists complement other mental health clinicians by prescribing certain medications and making decisions about hospital admission. But when psychiatry support is not available a range of team members can contribute to a person’s mental health care.
Can my GP help?
Depending on your mental health concerns, your GP may be able to offer alternatives while you await formal psychiatry care.
GPs provide support for a range of mental health concerns, regardless of formal diagnosis. They can help address the causes and impact of issues including mental distress, changes in sleep, thinking, mood or behaviour.
The GP Psychiatry Support Line also provides doctors advice on care, prescription medication and how support can work.
It’s a good idea to book a long consult and consider taking a trusted person. Be explicit about how you’ve been feeling and what previous supports or medication you’ve accessed.
What about psychologists, counsellors or community services?
Your GP should also be aware of supports available locally and online.
For example, Head to Health is a government initiative, including information, a nationwide phone line, and in-person clinics in Victoria. It aims to improve mental health advice, assessment and access to treatment.
Medicare Mental Health Centres provide in-person care and are expanding across Australia.
There are also virtual care services in some areas. This includes advice on individualised assessment including whether to go to hospital.
Some community groups are led by peers rather than clinicians, such as Alternatives to Suicide.
How about if I’m rural or regional?
Accessing support in rural or regional areas is particularly tough.
Beyond helplines and formal supports, other options include local Suicide Prevention Networks and community initiatives such as ifarmwell and Men’s sheds.
Should I go to emergency?
As the new report shows, people who present at hospital emergency departments for mental health should expect long wait times before being admitted to a ward.
But going to a hospital emergency department will be essential for some who are experiencing a physical or mental health crisis.
Managing suicide-related distress
With the mass resignation of NSW psychiatrists looming, and amid shortages and blown-out emergency waiting times, people in suicide-related distress must receive the best available care and support.
Roughly nine Australians die by suicide each day. One in six have had thoughts of suicide at some point in their lives.
Suicidal thoughts can pass. There are evidence-based strategies people can immediately turn to when distressed and in need of ongoing care.
Safety planning is a popular suicide prevention strategy to help you stay safe.
What is a safety plan?
This is a personalised, step-by-step plan to remain safe during the onset or worsening of suicidal urges.
You can develop a safety plan collaboratively with a clinician and/or peer worker, or with loved ones. You can also make one on your own – many people like to use the Beyond Now app.
Safety plans usually include:
- recognising personal warning signs of a crisis (for example, feeling like a burden)
- identifying and using internal coping strategies (such as distracting yourself by listening to favourite music)
- seeking social supports for distraction (for example, visiting your local library)
- letting trusted family or friends know how you’re feeling – ideally, they should know they’re in your safety plan
- knowing contact details of specific mental health services (your GP, mental health supports, local hospital)
- making the environment safer by removing or limiting access to lethal means
- identifying specific and personalised reasons for living.
Our research shows safety planning is linked to reduced suicidal thoughts and behaviour, as well as feelings of depression and hopelessness, among adults.
Evidence from people with lived experience shows safety planning helps people to understand their warning signs and practice coping strategies.
Sharing your safety plan with loved ones may help understand warning signs of a crisis. Dragana Gordic/Shutterstock Are there helplines I can call?
There are people ready to listen, by phone or online chat, Australia-wide. You can try any of the following (most are available 24 hours a day, seven days a week):
Suicide helplines:
- Lifeline 13 11 14
- Suicide Call Back Service 1300 659 467
There is also specialised support:
- for men: MensLine Australia 1300 78 99 78
- children and young people: Kids’ Helpline 1800 55 1800
- Aboriginal and Torres Strait Islander people: 13YARN 13 92 76
- veterans and their families: Open Arms 1800 011 046
- LGBTQIA+ community: QLife 1300 184 527
- new and expecting parents: PANDA 1300 726 306
- people experiencing eating disorders: Butterfly Foundation 1800 33 4673.
Additionally, each state and territory will have its own list of mental health resources.
With uncertain access to services, it’s helpful to remember that there are people who care. You don’t have to go it alone.
Monika Ferguson, Senior Lecturer in Mental Health, University of South Australia and Nicholas Procter, Professor and Chair: Mental Health Nursing, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Natto vs Tofu – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
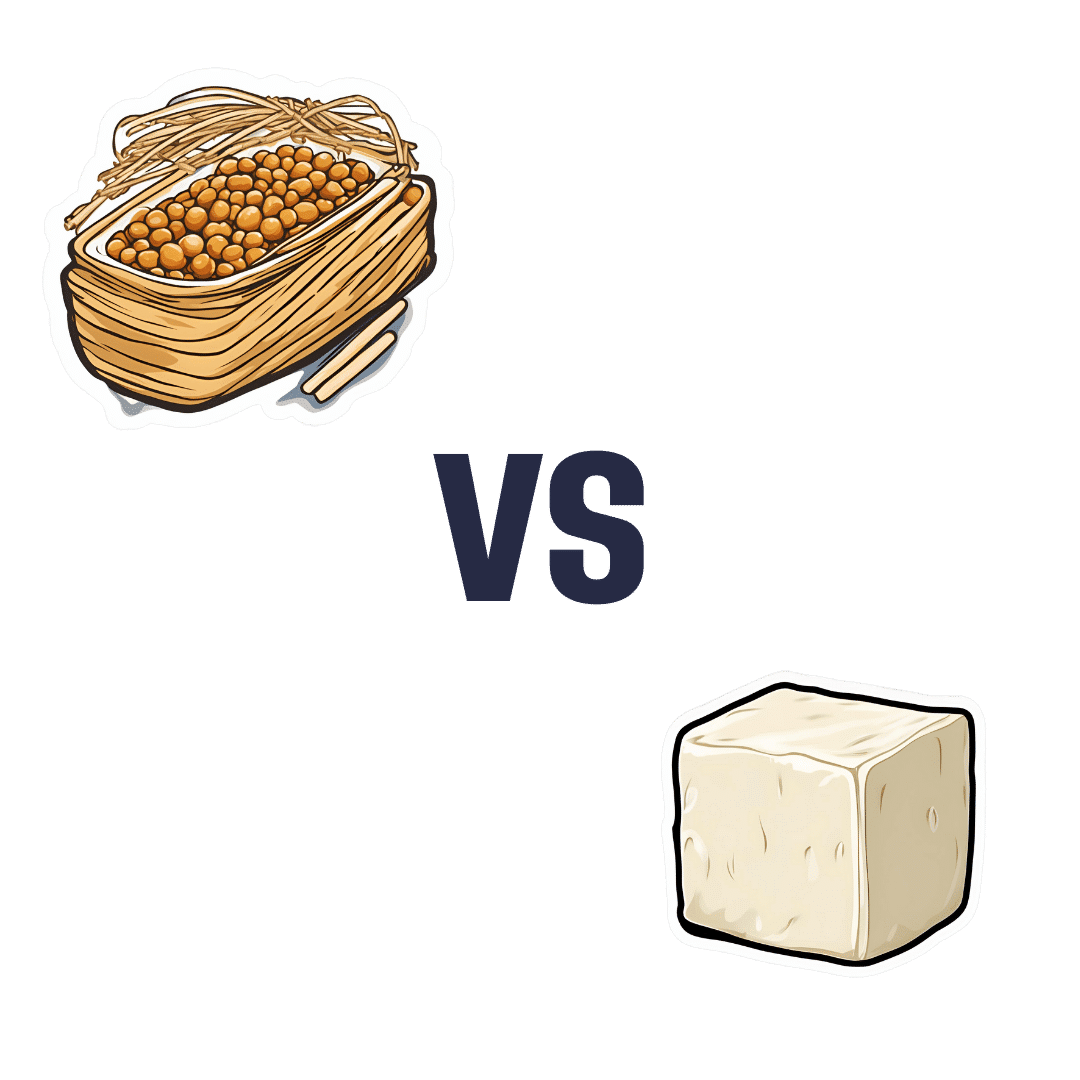
When comparing nattō to tofu, we picked the nattō.
Why?
In other words, in the comparison of fermented soy to fermented soy, we picked the fermented soy. But the relevant difference here is that nattō is fermented whole soybeans, while tofu is fermented soy milk of which the coagulated curds are then compressed into a block—meaning that the nattō is the one that has “more food per food”.
Looking at the macros, it’s therefore no surprise that nattō has a lot more fiber to go with its higher carb count; it also has slightly more protein. You may be wondering what tofu has more of, and the answer is: water.
In terms of vitamins, nattō has more of vitamins B2, B4, B6, C, E, K, and choline, while tofu has more of vitamins A, B3, and B9. So, a 7:3 win for nattō, even before considering that that vitamin C content of nattō is 65x more than what tofu has.
When it comes to minerals, nattō has more copper, iron, magnesium, manganese, potassium, and zinc, while tofu has more calcium, phosphorus, and selenium. So, a 6:3 win for nattō, and yes, the margins of difference are comparable (being 2–3x more for most of these minerals).
In short, both of these foods are great, but nattō is better.
Want to learn more?
You might like to read:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Brain-Skin Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of Brains And Breakouts
Today’s spotlight is on Dr. Claudia Aguirre. She’s a molecular neuroscientist, and today she’s going to be educating us about skin.
What? Why?
When we say “neuroscience”, we generally think of the brain. And indeed, that’s a very important part of it.
We might think about eyes, which are basically an extension of the brain.
We don’t usually think about skin, which (just like our eyes) is constantly feeding us a lot of information about our surroundings, via a little under three million nerve endings. Guess where the other ends of those nerves lead!
There’s a constant two-way communication going on between our brain and our skin.
What does she want us to know?
Psychodermatology
The brain and the skin talk to each other, and maladies of one can impact the other:
- Directly, e.g. stress prompting skin breakouts (actually this is a several-step process physiologically, but for the sake of brevity we’ll call this direct)
- Indirectly, e.g. nervous disorders that result in people scratching or picking at their skin, which prompts a whole vicious cycle of one thing making the other worse
Read more: Psychodermatology: The Brain-Skin Connection
To address both kinds of problems, clearly something beyond moisturizer is needed!
Mindfulness (meditation and beyond)
Mindfulness is a well-evidenced healthful practice for many reasons, and Dr. Aguirra argues the case for it being good for our skin too.
As she points out,
❝Cultural stress and anxiety can trigger or aggravate many skin conditions—from acne to eczema to herpes, psoriasis, and rosacea.
Conversely, a disfiguring skin condition can trigger stress, anxiety, depression, and even suicide.
Chronic, generalized anxiety can create chronic inflammation and exacerbate inflammatory skin conditions, such as those I mentioned previously.
Chronic stress can result in chronic anxiety, hypervigilance, poor sleep, and a whole cascade of effects resulting in a constant breakdown of tissues and organs, including the skin.❞
So, she recommends mindfulness-based stress reduction (MBSR), for the above reasons, along with others!
Read more: Mind Matters
How to do it: No-Frills, Evidence-Based Mindfulness
And as for “and beyond?”
Do you remember in the beginning of the pandemic, when people were briefly much more consciously trying to avoid touching their faces so much? That, too, is mindfulness. It may have been a stressed and anxious mindfulness for many*, but mindfulness nonetheless.
*which is why “mindfulness-based stress reduction” is not a redundant tautology repeated more than once unnecessarily, one time after another 😉
So: do try to keep aware of what you are doing to your skin, and so far as is reasonably practicable, only do the things that are good for it!
The skin as an endocrine organ
Nerves are not the only messengers in the body; hormones do a lot of our body’s internal communication too. And not just the ones everyone remembers are hormones (e.g. estrogen, testosterone, although yes, they do both have a big impact on skin too), but also many more, including some made in the skin itself!
Dr. Aguirra gives us a rundown of common conditions, the hormones behind them, and what we can do if we don’t want them:
Read more: Rethinking The Skin As An Endocrine Organ
Take-away advice:
For healthy skin, we need to do more than just hydrate, get good sleep, have good nutrition, and get a little sun (but not too much).
- We should also practice mindfulness-based stress reduction, and seek help for more serious mental health issues.
- We should also remember the part our hormones play in our skin, and not just the obvious ones.
Did you know that vitamin D is also a hormone, by the way? It’s not the only hormone at play in your skin by a long way, but it is an important one:
Society for Endocrinology | Vitamin D
Want to know more?
You might like this interview with Dr. Aguirre:
The Brain in Our Skin: An Interview with Dr. Claudia Aguirre
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
You Are Not Broken – by Dr. Kelly Casperson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many women express “I think I’m broken down there”, and it turns out simply that neither they nor their partners had the right knowledge, that’s all. The good news is: bedroom competence is an entirely learnable skill!
Dr. Casperson is a urologist, and over the years has expanded her work into all things pelvic, including the relevant use of both systemic and topical hormones (as in, hormones to increase overall blood serum levels of that hormone, like most HRT, and also, creams and lotions to increase levels of a given hormone in one particular place).
However, this is not 200 pages to say “take hormones”. Rather, she covers many areas of female sexual health and wellbeing, including yes, simply pleasure. From the physiological to the psychological, Dr. Casperson talks the reader through avoiding blame games and “getting out of your head and into your body”.
Bottom line: if you (or a loved one) are one of the many women who have doubts about being entirely correctly set up down there, then this book is definitely for you.
Click here to check out You Are Not Broken, and indeed stop “should-ing” all over your sex life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: