Brazil Nuts vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Brazil nuts to cashews, we picked the cashews.
Why?
Looking at the macros first, Brazil nuts have more fat and fiber, while cashews have more carbs and protein. So, it really comes down to what you want to prioritize. We’d generally consider fiber the tie-breaker, making this category a subjective marginal win for Brazil nuts—and especially marginal since they are both low glycemic index foods in any case.
When it comes to vitamins, Brazil nuts have more of vitamins C, E, and choline, while cashews have more of vitamins B2, B3, B5, B6, B7, B9, and K, so while both are great, this category is a clear by-the-numbers win for cashews.
The category of minerals is an interesting one. Brazil nuts have more calcium, magnesium, phosphorus, and selenium, while cashews have more copper, iron, manganese, and zinc. That would be a 4:4 tie, but let’s take a closer look at those selenium levels:
- A cup of cashews contains 109% of the RDA of selenium. Your hair will be luscious and shiny.
- A cup of Brazil nuts contains 10,456% of the RDA of selenium. This is way past the point of selenium toxicity, and your (luscious, shiny) hair will fall out.
For this reason, it’s recommended to eat no more than 3–4 Brazil nuts per day.
We consider that a point against Brazil nuts.
Adding up the section makes for a win for cashews. Of course, enjoy Brazil nuts too if you will, but in careful moderation please!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Pesto Pizza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not only is this pizza full of foods that punch above their weight healthwise, there’s no kneading and no waiting when it comes to the base, either. Homemade pizzas made easy!
You will need
For the topping:
- 1 zucchini, sliced
- 1 red bell pepper, cut into strips
- 3 oz mushrooms, sliced
- 3 shallots, cut into quarters
- 6 sun-dried tomatoes, roughly chopped
- ½ bulb garlic (paperwork done, but cloves left intact, unless they are very large, in which case halve them)
- 1 oz pitted black olives, halved
- 1 handful arugula
- 1 tbsp extra virgin olive oil
- 2 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
For the base:
- ½ cup chickpea flour (also called besan or gram flour)
- 2 tsp extra virgin olive oil
- ½ tsp baking powder
- ⅛ tsp MSG or ¼ tsp low-sodium salt
For the pesto sauce:
- 1 large bunch basil, chopped
- ½ avocado, pitted and peeled
- 1 oz pine nuts
- ¼ bulb garlic, crushed
- 2 tbsp nutritional yeast
- 1 tsp black pepper
- Juice of ½ lemon
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Toss the zucchini, bell pepper, mushrooms, shallots, and garlic cloves in 1 tbsp olive oil, ensuring an even coating. Season with the black pepper and MSG/salt, and put on a baking tray lined with baking paper, to roast for about 20 minutes, until they are slightly charred.
3) When the vegetables are in the oven, make the pizza base by combining the dry ingredients in a bowl, making a pit in the middle of it, adding the olive oil and whisking it in, and then slowly (i.e., a little bit at a time) whisking in 1 cup cold water. This should take under 5 minutes.
4) Don’t panic when this doesn’t become a dough; it is supposed to be a thick batter, so that’s fine. Pour it into a 9″ pizza pan, and bake for about 15 minutes, until firm. Rotate it if necessary partway through; whether it needs this or not will depend on your oven.
5) While the pizza base is in the oven, make the pesto sauce by blending all the pesto sauce ingredients in a high-speed blender until smooth.
6) When the base and vegetables are ready (these should be finished around the same time), spread the pesto sauce on the base, scatter the arugula over it followed by the vegetables and then the olives and sun-dried tomatoes.
7) Serve, adding any garnish or other final touches that take your fancy.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Bell Peppers To Pick? A Spectrum Of Specialties
- Ergothioneine In Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Black Olives vs Green Olives – Which is Healthier
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Coconut vs Avocado – Which is Healthier?
- Herbs for Evidence-Based Health & Healing
- Spermidine For Longevity
Take care!
Share This Post
-
Hoisin Sauce vs Teriyaki Sauce – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hoisin sauce to teriyaki sauce, we picked the teriyaki sauce.
Why?
Neither are great! But spoonful for spoonful, the hoisin sauce has about 5x as much sugar.
Of course, exact amounts will vary by brand, but the hoisin will invariably be much more sugary than the teriyaki.
On the flipside, the teriyaki sauce may sometimes have slightly more salt, but they are usually in approximately the same ballpark of saltiness, so this is not a big deciding factor.
As a general rule of thumb, the first few ingredients will look like this for each, respectively:
Hoisin:
- Sugar
- Water
- Soybeans
Teriyaki:
- Soy sauce (water, soybeans, salt)
- Rice wine
- Sugar
In essence: hoisin is a soy-flavored syrup, while teriyaki is a sweetened soy sauce
Wondering about that rice wine? The alcohol content is negligible, sufficiently so that teriyaki sauce is not considered alcoholic. For health purposes, it is well under the 0.05% required to be considered alcohol-free.
For religious purposes, we are not your rabbi or imam, but to our best understanding, teriyaki sauce is generally considered kosher* (the rice wine being made from rice) and halal (the rice wine being de-alcoholized by the processing, making the sauce non-intoxicating).
Want to try some?
You can compare these examples side-by-side yourself:
Enjoy!
Share This Post
-
What are plyometric exercises? How all that hopping and jumping builds strength, speed and power
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve ever seen people at the gym or the park jumping, hopping or hurling weighted balls to the ground, chances are they were doing plyometric exercises.
Examples include:
- box jumps, where you repeatedly leap quickly on and off a box
- lateral skater hops, where you bound from side to side like a speeding ice skater
- rapidly throwing a heavy medicine ball against a wall, or to the ground
- single leg hops, which may involve hopping on the spot or through an obstacle course
- squat jumps, where you repeatedly squat and then launch yourself into the air.
Photo by cottonbro studio/Pexels There are many more examples of plyometric exercises.
What ties all these moves together is that they use what’s known as the “stretch shortening cycle”. This is where your muscles rapidly stretch and then contract.
Runners routinely practise plyometric exercises to improve explosive leg strength. WoodysPhotos/Shutterstock Potential benefits
Research shows incorporating plyometric exercise into your routine can help you:
- jump higher
- sprint faster
- reduce the chances of getting a serious sporting injuries such as anterior cruciate ligament (ACL) tears
- build muscle strength
- improve bone mineral density (especially when combined with resistance training such as weight lifting), which is particularly important for women and older people at risk of falls.
Studies have found plyometric exercises can help:
- older people who want to retain and build muscle strength, boost bone health, improve posture and reduce the risk of falls
- adolescent athletes who want to build the explosive strength needed to excel in sports such as athletics, tennis, soccer, basketball and football
- female athletes who want to jump higher or change direction quickly (a useful skill in many sports)
- endurance runners who want to boost physical fitness, run time and athletic performance.
And when it comes to plyometric exercises, you get out what you put in.
Research has found the benefits of plyometrics are significantly greater when every jump was performed with maximum effort.
Jumping can help boost bone strength. WoodysPhotos/Shutterstock Potential risks
All exercise comes with risk (as does not doing enough exercise!)
Plyometrics are high-intensity activities that require the body to absorb a lot of impact when landing on the ground or catching medicine balls.
That means there is some risk of musculoskeletal injury, particularly if the combination of intensity, frequency and volume is too high.
You might miss a landing and fall, land in a weird way and crunch your ankle, or get a muscle tear if you’re overdoing it.
The National Strength and Conditioning Association, a US educational nonprofit that uses research to support coaches and athletes, recommends:
- a maximum of one to three plyometric sessions per week
- five to ten repetitions per set and
- rest periods of one to three minutes between sets to ensure complete muscle recovery.
With the right guidance, jumps can be safe for older people and may help reduce the risk of falls as you age. Realstock/Shutterstock One meta-analysis, where researchers looked at many studies, found plyometric training was feasible and safe, and could improve older people’s performance, function and health.
Overall, with appropriate programming and supervision, plyometric exercise can be a safe and effective way to boost your health and athletic performance.
Justin Keogh, Associate Dean of Research, Faculty of Health Sciences and Medicine, Bond University and Mandy Hagstrom, Senior Lecturer, Exercise Physiology. School of Health Sciences, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
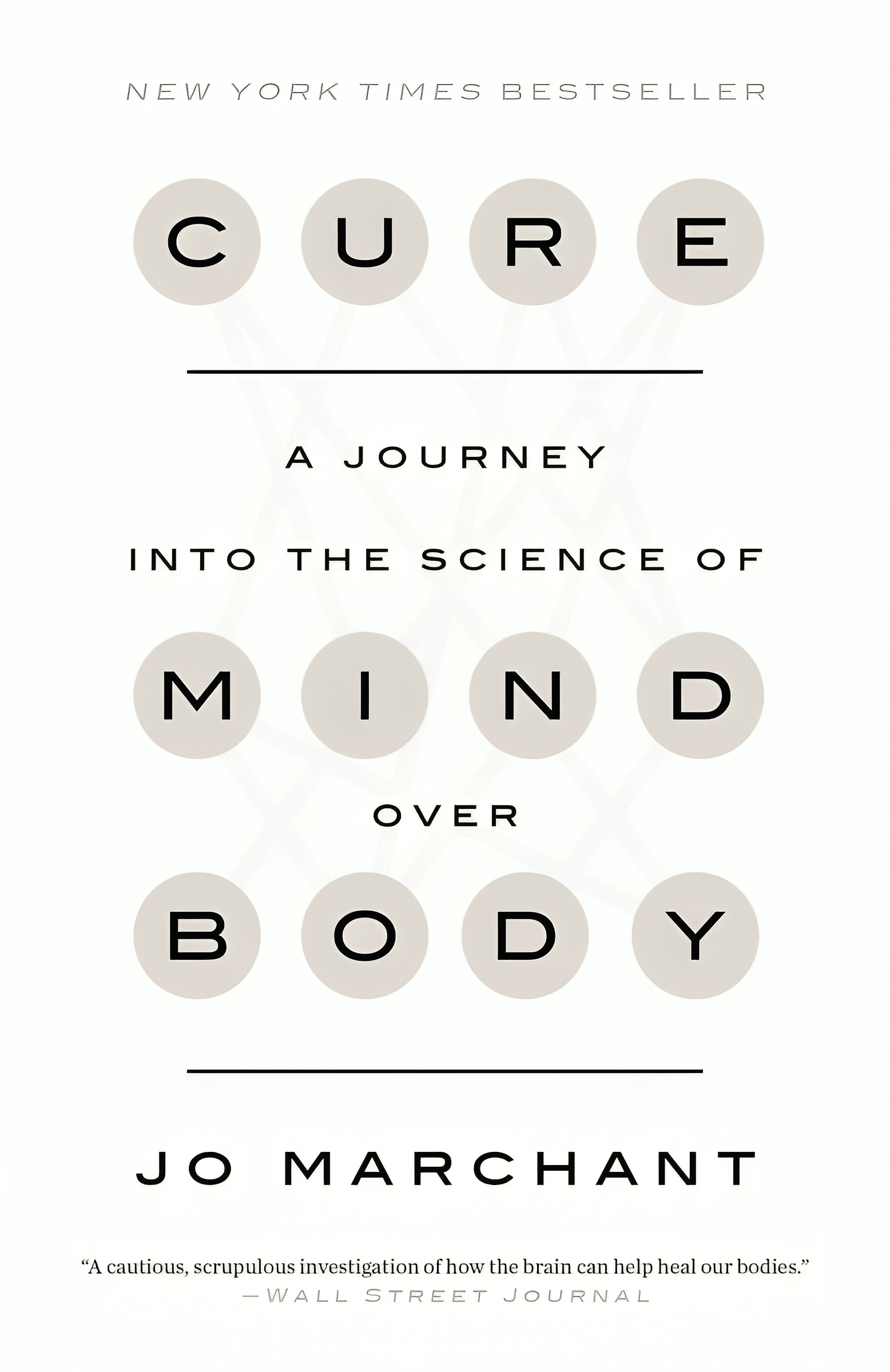
Cure – by Dr. Jo Marchant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle here, “a journey into the science of mind over body”, prompts an immediate question: is this book actually about science?
And yes, yes it is. It’s not about “positive energy” or “tapping into your divine essence” or anysuch. It’s about science, and scientific studies.
The author’s PhD is in genetics and medical microbiology, not metaphysics or something.
For those of us who read a lot of clinical studies about a lot of things (hi, regular researcher/writer here), we’re very used to placebo being used as a control in medical science.
“This drug performed no better than placebo” is generally considered a disappointing statement… But what if the placebo was already having a profound effect? Shouldn’t that be worthy of note too?
Dr. Marchant looks at more than just drugs, though, and also looks into the science (complete with EEGs and such) of hypnosis and virtual reality.
The writing style here is very accessible without skimping on science. This is to be expected; Dr. Marchant also has an MSc in science communication, and spent a time as senior editor of New Scientist magazine.
This isn’t a how-to book, but there are some practical takeaways too, specific things we can do to augment (or avoid sabotaging) any medications we take, for example.
Bottom line: placebo effect (and its evil twin, the nocebo effect) has a profound impact on all of us whether we want it or not, so we might as well learn about how it works and how to leverage it. This book gives a very good, hard science grounding.
Click here to check out “Cure” and get the most out of whatever you take (or do) for your health!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Recognize Perfectly Hidden Depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Margaret Rutherford shares her insights from 30 years of professional experience:
There’s only one way to know
In this video, Dr. Rutherford discusses several (presumably pseudonymized) cases of people who came to her therapy office seeming to have their lives very much together when they very much didn’t, including the woman who came in with symptoms of mild anxiety, and then tried to kill herself, and the man who was outwardly an overachiever while consumed with feelings of guilt and shame.
She discusses how even the most skilled mental health professionals will tend to miss hidden depression, as they focus on visible symptoms from the DSM criteria, which may not reflect the patient’s reality, especially for those hiding their struggles.
So, the crux becomes: why do people hide their struggles? One does not go to the emergency room with a broken limb and then say to the doctor “I’m fine thank you; how are you?” so why do people do that when it comes to mental health issues?
The reality is that the shame of revealing feelings like shame itself, fear, and self-loathing keeps people silent, and in particular, research (Schneiderman et al.) shows that emotional pain plays a central role in suicide, and (per Blatt et al.) perfectionism can drastically alter the presentation of depression, making it even harder to diagnose through standard criteria than it already was.
As for what can be done about it? Dr. Rutherford advocates for a cultural shift where talking about emotional pain, including suicidal thoughts, is seen as normal and not shameful. That people need to feel safe expressing these feelings, to prevent tragic outcomes. Instead of judging or dismissing someone with suicidal thoughts, she encourages a compassionate and accepting approach to open up dialogue and understanding.
In short, that everyone can contribute to a culture that views transparency and vulnerability as strengths, helping reduce the stigma around mental health struggles.
And that’s the only way we’ll ever be able to recognize perfectly hidden depression—if people no longer feel that they have to hide it.
For more on all of this, here’s Dr. Rutherford herself:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Mental Health First Aid (That You’ll Hopefully Never Need) ← This is about managing depression, in yourself or others
- How To Stay Alive (When You Really Don’t Want To) ← This is about managing suicidality, in yourself or others
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Seven-Day Sleep Prescription – by Dr. Aric Prather
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You probably already know about sleep hygiene. So, what does this book have to offer?
Dr. Aric Prather offers seven days’ worth of adjustments, practices to take up, from when you get up in the morning to when you lay your head down at night.
Some you’ll surely be familiar with, like avoiding blue light and social media at night.
Others, you might not be familiar with, like scheduling 15 minutes for worrying in the daytime. The rationale for this one is that when you find yourself inclined to worry at a time that will keep you awake, you’ll know that you can put off such thoughts to your scheduled “worrying time”. That they’ll be addressed then, and that you can thus sleep soundly meanwhile.
Where the book really comes into its own is in such things as discussing how to not just manage sleep debt, but how to actually use it in your favour.
Nor does Dr. Prather shy away from the truths of our world… That the world these days is not built for us to sleep well. That there are so many other priorities; to get our work done, to succeed and achieve, to pay bills, to support our kids and partners. That so many of these things make plenty of sense in the moment, but catch up with us eventually.
Bottom line: what this book aims to give is a genuinely sustainable approach to sleeping—controlling what we can, and working with what we can’t. If you’d like to have a better relationship with sleep, this book is an excellent choice.
Click here to check out the Seven-Day Sleep Prescription, and improve yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: