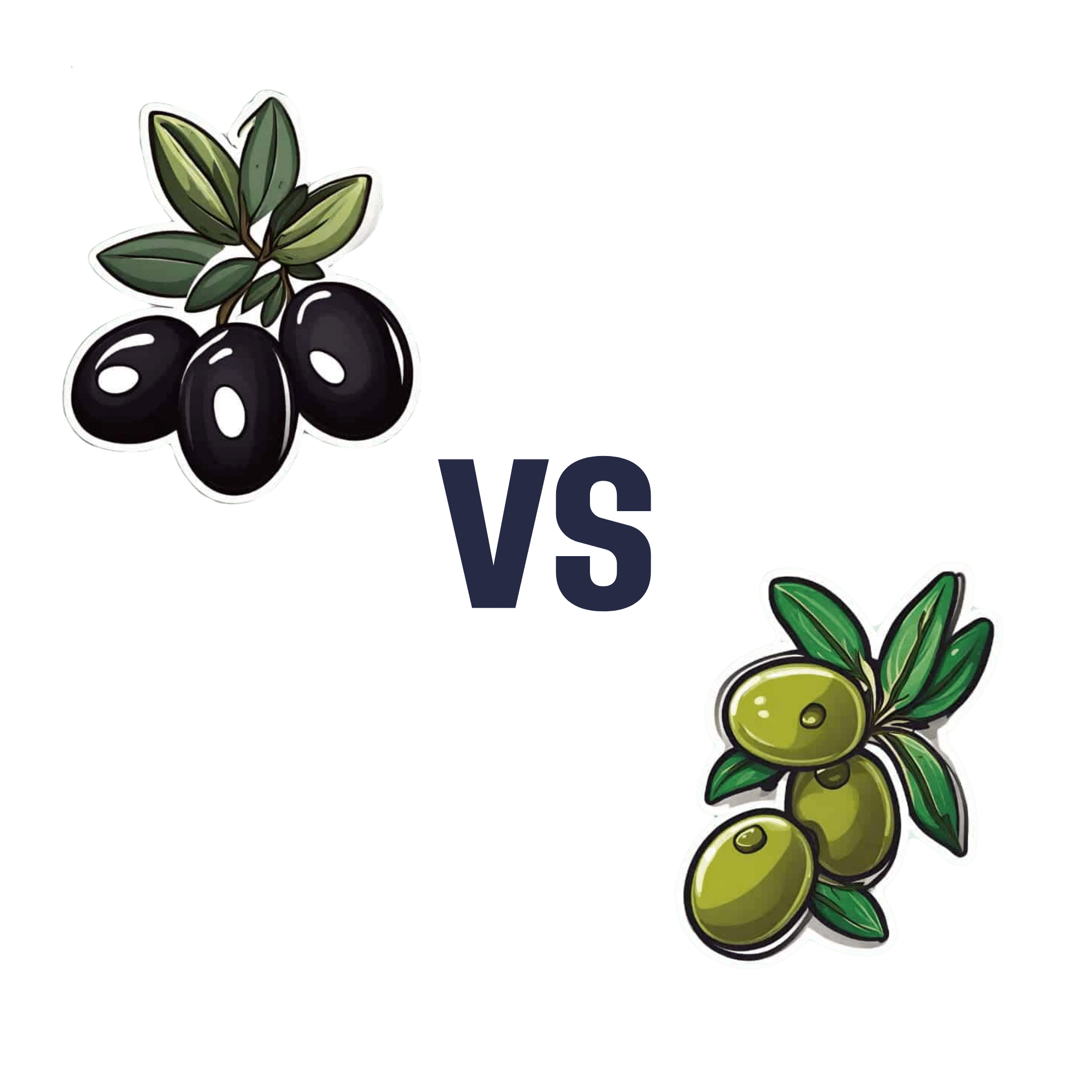
Black Olives vs Green Olives – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing black olives to green olives, we picked the black olives.
Why?
First know this: they are the same plant, just at different stages of ripening (green olives are, as you might expect, less ripe).
Next: the nutritional values of both, from macros down to the phytochemicals, are mostly very similar, but there are a few things that stand out:
• Black olives usually have more calories per serving, average about 25% more. But these are from healthy fats, so unless you’re on a calorie-restricted diet, this is probably not a consideration.
• Green olives are almost always “cured” for longer, which results in a much higher sodium content often around 200% that of black olives. Black olives are often not “cured” at all.
Hence, we chose the black olives!
You may be wondering: do green olives have anything going for them that black olives don’t?
And the answer has a clue in the taste: green olives generally have a stronger, more bitter/pungent taste. And remember what we said about things that have a stronger, more bitter/pungent taste:
Tasty Polyphenols: Enjoy Bitter Foods For Your Heart & Brain
That’s right, green olives are a little higher in polyphenols than black olives.
But! If you want to enjoy the polyphenol content of green olives without the sodium content, the best way to do that is not olives, but olive oil—which is usually made from green olives.
For more about olive oil, check out:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Avocado Oil vs Olive Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado oil to olive oil, we picked the olive oil.
Why?
Avocados and olives are both very healthy foods. However, when they are made into oils, there’s an important distinguishing factor:
Olive oil usually retains a lot of the micronutrients from the olives (including vitamins E and K), whereas no measurable micronutrients usually remain in avocado oil.
So while both olive oil and avocado oil have a similar (excellent; very heart-healthy!) lipids profile, the olive oil has some bonuses that the avocado oil doesn’t.
We haven’t written about the nutritional profiles of either avocados or olives yet, but here’s what we had to say on the different kinds of olive oil available:
And here’s an example of a good one on Amazon, for your convenience 😎
Share This Post
-
Blueberries vs Elderberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blueberries to elderberries, we picked the elderberries.
Why?
Both are certainly top-tier fruits! But…
In terms of macros, elderberries have more than 2x the fiber, while the two berries are approximately equal on other macros. An easy win for elderberries in this category.
In the category of vitamins, blueberries have more of vitamins E, K, and choline, while elderberries have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, and C, scoring another win for elderberries here.
When it comes to minerals, blueberries have more magnesium, manganese, and zinc, while elderberries have more calcium, copper, iron, phosphorus, potassium, and selenium—one more win for elderberries.
In terms of phytochemicals, both berries are (like most berries) an abundant source of polyphenols, but elderberries have more, including more quercetin, too.
Adding up the sections makes for a convincing win for elderberries, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Herbs For Evidence-Based Health & Healing ← elderberry significantly hastens recovery from upper respiratory viral infections 😎
Enjoy!
Share This Post
-
What Seasonal Allergies Mean For Your Heart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people associate seasonal allergies with itchy eyes and stuffy noses, but the effects can go a lot deeper.
This is because allergic reactions don’t just affect the respiratory system; they trigger chronic inflammation throughout the body, and in fact:
❝Allergic disease is a systemic and inflammatory condition❞
~ Dr. Rauno Joks, whose work we will cite in a moment
The important thing to understand in terms of heart health, is that chronic* systemic inflammation can contribute to coronary artery disease, where plaque buildup in arteries (bearing in mind, arterial plaque is in large part made of dead immune cells) raises the risk of heart attacks and strokes.
*Yes, a season once or twice per year counts as “chronic”.
A large (n=603,140) study found that allergic rhinitis (hay fever) increased the odds of coronary heart disease by 25% and heart attacks by 20%. Asthma, especially during flare-ups, posed an even greater risk:
Beyond biology
The effects aren’t just biological; allergies can limit physical activity, leading to a sedentary lifestyle that harms heart health.
In other words: if you’re not going outdoors because there’s pollen, and you’re not exercising because you’re exhausted, then the rest of your health is going to take a nose-dive (so to speak) too.
So, one more reason to take it seriously and not just dismiss it as “it’s just allergies, I’ll survive”.
Practical takeaways
Some things we can all do:
- Monitor your risk factors; i.e. keep on top of your heart health metrics, especially blood pressure and cholesterol, as well as any known genetic predisposition to cardiovascular disease.
- Watch out for alternative causes: symptoms like fatigue or shortness of breath may not always be allergies; they could signal asthma, reflux (for example if wheezing), or even heart disease. An allergist is a good first port-of-call, though.
- Be cautious with medications: some decongestants / allergy meds / asthma meds can raise blood pressure and/or interfere with other medications. Your pharmacist is the best person to speak to about this; they know this kind of thing much better than doctors, as a rule. And whenever you get a new medication, it is good practice to make a habit of always reading the information leaflet that comes with it, and/or look it up on a reputable website such as Drugs.com or the the BNF, to learn about what it is, how it works, what the risks are, what its contraindications are, etc.
- Don’t ignore warning signs: lightheadedness or chest pain could indicate a heart issue and should be addressed immediately. It’s better to be wrong and temporarily embarrassed, than wrong and permanently dead. Besides, even if it’s not a heart issue, it may be something else that would benefit from attention, so taking it seriously is always a good idea.
Want to know more?
Check out:
- What Your Mucus Says About Your Health
- Antihistamines’ Generation Gap
- Oh, Honey: The Bee’s Knees? ← what science has to say about “honey will inoculate you against allergies”
Take care!
Share This Post
Related Posts
-
Thinking about cosmetic surgery? New standards will force providers to tell you the risks and consider if you’re actually suitable
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People considering cosmetic surgery – such as a breast augmentation, liposuction or face lift – should have extra protection following the release this week of new safety and quality standards for providers, from small day-clinics through to larger medical organisations.
The new standards cover issues including how these surgeries are advertised, psychological assessments before surgery, the need for people to be informed of risks associated with the procedure, and the type of care people can expect during and afterwards. The idea is for uniform standards across Australia.
The move is part of sweeping reforms of the cosmetic surgery industry and the regulation of medical practitioners, including who is allowed to call themselves a surgeon.
It is heartening to see these reforms, but some may say they should have come much sooner for what’s considered a highly unregulated area of medicine.
Why do people want cosmetic surgery?
Australians spent an estimated A$473 million on cosmetic surgery procedures in 2023.
The major reason people want cosmetic surgery relates to concerns about their body image. Comments from their partners, friends or family about their appearance is another reason.
The way cosmetic surgery is portrayed on social media is also a factor. It’s often portrayed as an “easy” and “accessible” fix for concerns about someone’s appearance. So such aesthetic procedures have become far more normalised.
The use of “before” and “after” images online is also a powerful influence. Some people may think their appearance is worse than the “before” photo and so they think cosmetic intervention is even more necessary.
People don’t always get the results they expect
Most people are satisfied with their surgical outcomes and feel better about the body part that was previously concerning them.
However, people have often paid a sizeable sum of money for these surgeries and sometimes experienced considerable pain as they recover. So a positive evaluation may be needed to justify these experiences.
People who are likely to be unhappy with their results are those with unrealistic expectations for the outcomes, including the recovery period. This can occur if people are not provided with sufficient information throughout the surgical process, but particularly before making their final decision to proceed.
What’s changing?
According to the new standards, services need to ensure their own advertising is not misleading, does not create unreasonable expectations of benefits, does not use patient testimonials, and doesn’t offer any gifts or inducements.
For some clinics, this will mean very little change as they were not using these approaches anyway, but for others this may mean quite a shift in their advertising strategy.
It will likely be a major challenge for clinics to monitor all of their patient communication to ensure they adhere to the standards.
It is also not quite clear how the advertising standards will be monitored, given the expanse of the internet.
What about the mental health assessment?
The new standards say clinics must have processes to ensure the assessment of a patient’s general health, including psychological health, and that information from a patient’s referring doctor be used “where available”.
According to the guidelines from the Medical Board of Australia, which the standards are said to complement, all patients must have a referral, “preferably from their usual general practitioner or if that is not possible, from another general practitioner or other specialist medical practitioner”.
While this is a step in the right direction, we may be relying on medical professionals who may not specialise in assessing body image concerns and related mental health conditions. They may also have had very little prior contact with the patient to make their clinical impressions.
So these doctors need further training to ensure they can perform assessments efficiently and effectively. People considering surgery may also not be forthcoming with these practitioners, and may view them as “gatekeepers” to surgery they really want to have.
Ideally, mental health assessments should be performed by health professionals who are extensively trained in the area. They also know what other areas should be explored with the patient, such as the potential impact of trauma on body image concerns.
Of course, there are not enough mental health professionals, particularly psychologists, to conduct these assessments so there is no easy solution.
Ultimately, this area of health would likely benefit from a standard multidisciplinary approach where all health professionals involved (such as the cosmetic surgeon, general practitioner, dermatologist, psychologist) work together with the patient to come up with a plan to best address their bodily concerns.
In this way, patients would likely not view any of the health professionals as “gatekeepers” but rather members of their treating team.
If you’re considering cosmetic surgery
The Australian Commission on Safety and Quality in Health Care, which developed the new standards, recommended taking these four steps if you’re considering cosmetic surgery:
-
have an independent physical and mental health assessment before you commit to cosmetic surgery
-
make an informed decision knowing the risks
-
choose your practitioner, knowing their training and qualifications
-
discuss your care after your operation and where you can go for support.
My ultimate hope is people safely receive the care to help them best overcome their bodily concerns whether it be medical, psychological or a combination.
Gemma Sharp, Associate Professor, NHMRC Emerging Leadership Fellow & Senior Clinical Psychologist, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
-
“You Just Need to Lose Weight” And 19 Other Myths About Fat People – by Aubrey Gordon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed another book by this author, “What We Don’t Talk About When We Talk About Fat”, and this time, she’s doing some important mythbusting.
The titular “you just need to lose weight” is a commonly-taken easy-out for many doctors, to avoid having to dispense actual treatment for an actual condition. Whether or not weight loss would help in a given situation is often immaterial; “kicking the can down the road” is the goal.
Most of the book is divided into 20 chapters, each of them devoted to debunking one myth. Think of it like 10almonds’ “Mythbusting Friday” edition (indeed, we did one about obesity), but with an entire book, and as much room as she needs to provide much more detail than we can ever get into in a single article.
And far from being a mere polemic, she does indeed provide that detail—this is clearly a very well-researched book, above and beyond the author’s own personal experience. Further, all the key points are illustrated and articulated clearly, making the book’s ideas very comprehensible.
The style is pop-science, but with frequent bibliographical references for relevant sources.
Bottom line: for some readers, this book will come as a great validation; for others, it may be eye-opening. Either way, it’s a very worthwhile read.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cherries’ Very Healthy Wealth Of Benefits!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cherries’ Health Benefits Simply Pop
First, be aware, there are different kinds:
Sweet & Sour
Cherries can be divided into sweet vs sour. These are mostly nutritionally similar, though sour ones do have some extra benefits.
Sweet and sour cherries are closely related but botanically different plants; it’s not simply a matter of ripeness (or preparation).
These can mostly be sorted into varieties of Prunus avium and Prunus cerasus, respectively:
Cherry Antioxidants: From Farm to Table
Sour cherry varieties include morello and montmorency, so look out for those names in particular when doing your grocery-shopping.
You may remember that it’s a good rule of thumb that foods that are more “bitter, astringent, or pungent” will tend to have a higher polyphenol content (that’s good):
Enjoy Bitter Foods For Your Heart & Brain
Juiced up
Almost certainly for reasons of budget and convenience, as much as for standardization, most studies into the benefits of cherries have been conducted using concentrated cherry juice as a supplement.
At home, we need not worry so much about standardization, and our budget and convenience are ours to manage. To this end, as a general rule of thumb, whole fruits are pretty much always better than juice:
Which Sugars Are Healthier, And Which Are Just The Same?
Antioxidant & anti-inflammatory!
Cherries are a very good source of antioxidants, and as such they also reduce inflammation, which in turn means ameliorating autoimmune diseases, from common things like arthritis…
…to less common things like gout:
Cherry Consumption and the Risk of Recurrent Gout Attacks
This can also be measured by monitoring uric acid metabolites:
Consumption of cherries lowers plasma urate in healthy women
Anti-diabetic effect
Most of the studies on this have been rat studies, and the human studies have been less “the effect of cherry consumption on diabetes” and more a matter of separate studies adding up to this conclusion in, the manner of “cherries have this substance, this substance has this effect, therefore cherries will have this effect”. You can see an example of this discussed over the course of 15 studies, here:
A Review of the Health Benefits of Cherries ← skip to section 2.2.1: “Cherry Intake And Diabetes”
In short, the jury is out on cherry juice, but eating cherries themselves (much like getting plenty of fruit in general) is considered good against diabetes.
Good for healthy sleep
For this one, the juice suffices (actual cherries are still recommended, but the juice gave clear significant positive results):
Pilot Study of the Tart Cherry Juice for the Treatment of Insomnia and Investigation of Mechanisms ← this was specifically in people over the age of 50
Importantly, it’s not that cherries have a sedative effect, but rather they support the body’s ability to produce melatonin adequately when the time comes:
Effect of tart cherry juice (Prunus cerasus) on melatonin levels and enhanced sleep quality
Post-exercise recovery
Cherries are well-known for boosting post-exercise recovery, though they may actually improve performance during exercise too, if eaten beforehand/
For example, these marathon-runners who averaged 13% compared to placebo control:
As for its recovery benefits, we wrote about this before:
How To Speed Up Recovery After A Workout (According To Actual Science)
Want to get some?
We recommend your local supermarket (or farmer’s market!), but if for any reason you prefer to take a supplement, here’s an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: