Hoisin Sauce vs Teriyaki Sauce – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hoisin sauce to teriyaki sauce, we picked the teriyaki sauce.
Why?
Neither are great! But spoonful for spoonful, the hoisin sauce has about 5x as much sugar.
Of course, exact amounts will vary by brand, but the hoisin will invariably be much more sugary than the teriyaki.
On the flipside, the teriyaki sauce may sometimes have slightly more salt, but they are usually in approximately the same ballpark of saltiness, so this is not a big deciding factor.
As a general rule of thumb, the first few ingredients will look like this for each, respectively:
Hoisin:
- Sugar
- Water
- Soybeans
Teriyaki:
- Soy sauce (water, soybeans, salt)
- Rice wine
- Sugar
In essence: hoisin is a soy-flavored syrup, while teriyaki is a sweetened soy sauce
Wondering about that rice wine? The alcohol content is negligible, sufficiently so that teriyaki sauce is not considered alcoholic. For health purposes, it is well under the 0.05% required to be considered alcohol-free.
For religious purposes, we are not your rabbi or imam, but to our best understanding, teriyaki sauce is generally considered kosher* (the rice wine being made from rice) and halal (the rice wine being de-alcoholized by the processing, making the sauce non-intoxicating).
Want to try some?
You can compare these examples side-by-side yourself:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Triple Your Breast Cancer Survival Chances
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Keeping Abreast Of Your Cancer Risk
It’s the kind of thing that most people think won’t happen to them. And hopefully, it won’t!
But…
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
- *and even this depends on the type of double mastectomy and other circumstances, and technically there will always be a non-zero risk, because of complicating factors.
- Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
- That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
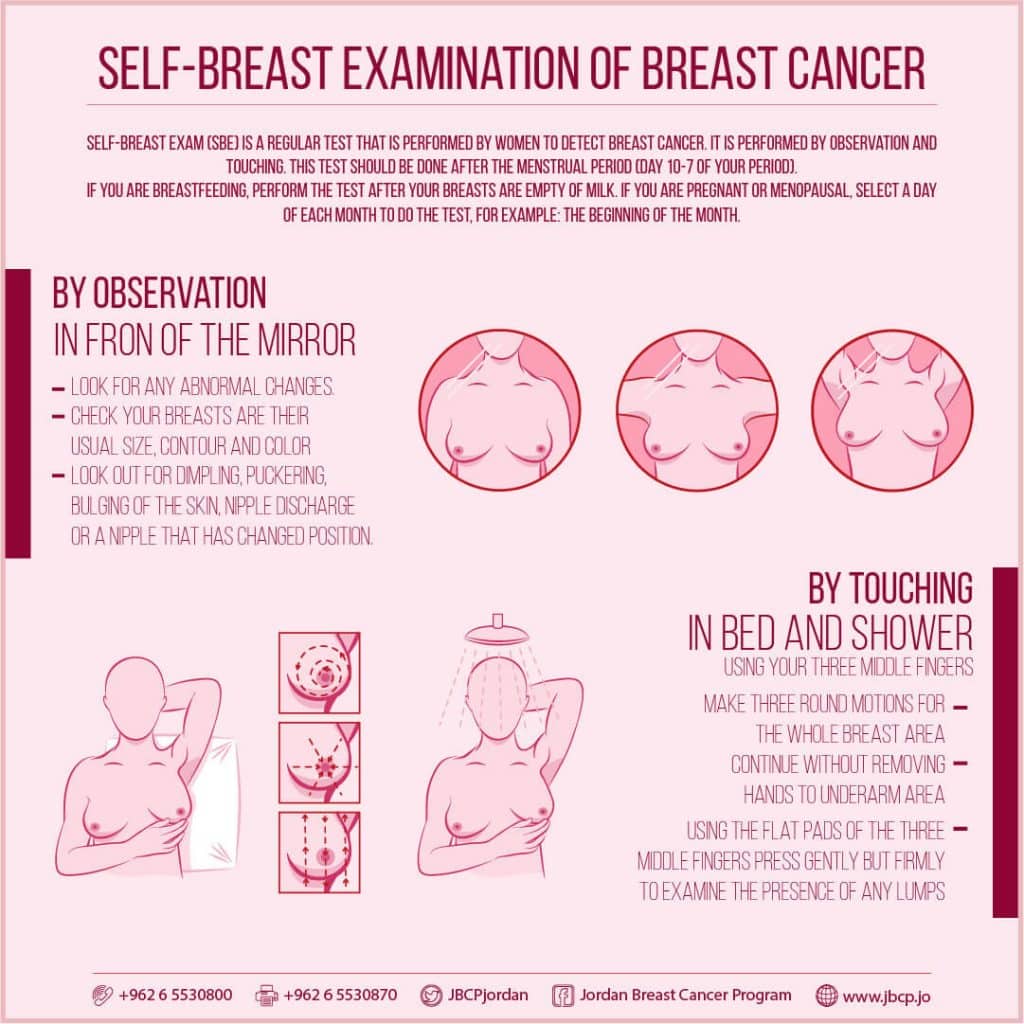
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
(This graphic was created by the Jordan Breast Cancer Program—check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it:
Click Here To Take The Free 4-Minute Breast Health Assessment!
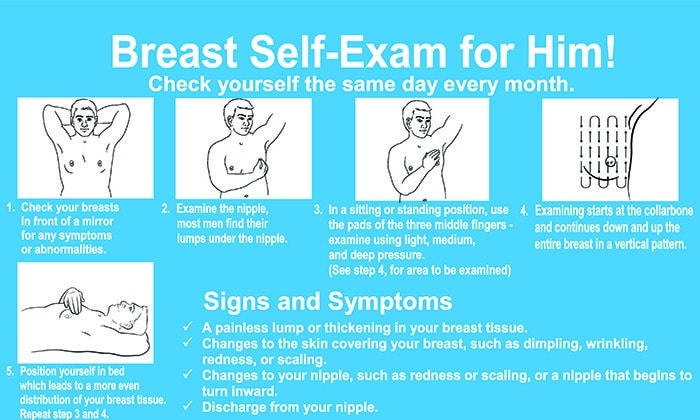
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to!
Take care of yourself; you’re important.
Share This Post
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
-
Vit D + Calcium: Too Much Of A Good Thing?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Vit D + Calcium: Too Much Of A Good Thing?
- Myth: you can’t get too much calcium!
- Myth: you must get as much vitamin D as possible!
Let’s tackle calcium first:
❝Calcium is good for you! You need more calcium for your bones! Be careful you don’t get calcium-deficient!❞
Contingently, those comments seem reasonable. Contingently on you not already having the right amount of calcium. Most people know what happens in the case of too little calcium: brittle bones, osteoporosis, and so forth.
But what about too much?
Hypercalcemia
Having too much calcium—or “hypercalcemia”— can lead to problems with…
- Groans: gastrointestinal pain, nausea, and vomiting. Peptic ulcer disease and pancreatitis.
- Bones: bone-related pains. Osteoporosis, osteomalacia, arthritis and pathological fractures.
- Stones: kidney stones causing pain.
- Moans: refers to fatigue and malaise.
- Thrones: polyuria, polydipsia, and constipation
- Psychic overtones: lethargy, confusion, depression, and memory loss.
(mnemonic courtesy of Sadiq et al, 2022)
What causes this, and how do we avoid it? Is it just dietary?
It’s mostly not dietary!
Overconsumption of calcium is certainly possible, but not common unless one has an extreme diet and/or over-supplementation. However…
Too much vitamin D
Again with “too much of a good thing”! While keeping good levels of vitamin D is, obviously, good, overdoing it (including commonly prescribed super-therapeutic doses of vitamin D) can lead to hypercalcemia.
This happens because vitamin D triggers calcium absorption into the gut, and acts as gatekeeper to the bloodstream.
Normally, the body only absorbs 10–20% of the calcium we consume, and that’s all well and good. But with overly high vitamin D levels, the other 80–90% can be waved on through, and that is very much Not Good™.
See for yourself:
- Hypercalcemia of Malignancy: An Update on Pathogenesis and Management
- Vitamin D-Mediated Hypercalcemia: Mechanisms, Diagnosis, and Treatment
How much is too much?
The United States’ Office of Dietary Supplements defines 4000 IU (100μg) as a high daily dose of vitamin D, and recommends 600 IU (15μg) as a daily dose, or 800 IU (20μg) if aged over 70.
See for yourself: Vitamin D Fact Sheet for Health Professionals ← there’s quite a bit of extra info there too
Share This Post
-
Turmeric (Curcumin) Dos and Don’ts With Dr. Kim
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Turmeric is a fabulous spice, most well-known for its anti-inflammatory powers; its antioxidant effects benefit all of the body, including the brain. While it fights seemingly everything from arthritis to atherosclerosis to Alzheimer’s and more, it also boosts brain-derived neurotrophic factor, looks after your cardiovascular health, holds back diabetes, reduces the risk of cancer, fights depression, slows aging, and basically does everything short of making you sing well too.
Dr. Leonid Kim goes over the scientific evidence for these, and also talks about some of the practicalities of taking turmeric, and safety considerations.
For the most part, turmeric is very safe even at high doses (up to 8g at least); indeed, at smaller doses (e.g. 500mg) it largely does the same job as non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, with fewer problems.
It also does the job of several antidiabetic medications, by increasing uptake of glucose (thus reducing blood sugar levels) while simultaneously decreasing the glucose secretion from the liver. It does this by regulating the AMPK signalling pathway, just like metformin—while again, being safer.
Dr. Kim also looks at the (good!) evidence for turmeric in managing PCOS and undoing NAFLD; so far, so good.
Dosage: he bids us pay attention whether we’re taking it as turmeric itself or as curcumin standardized extract. The latter is the active compound, and in principle more powerful, but in practice it can get metabolized too quickly and easily—before it can have its desired effect. So, turmeric itself is a very good choice.
Absorption: since we do want it to be absorbed well, though, he does recommend taking it with piperine (as in black pepper).
You may be thinking: isn’t this going to cause the same problem you were just talking about, and cause it to be metabolized too quickly? And the answer is: no! How piperine works is almost the opposite; it protects the curcumin in the turmeric from our digestive enzymes, and thus allows them to get absorbed without being broken down too quickly—thus increasing the bioavailability by slowing the process down.
Lipophilia: no, that’s not a disease (or a fetish), rather it means that curcumin is soluble in fats, so we should take it near in time to a meal that contains at least a tablespoon of oil in total (so if you’re cooking a curry with your turmeric, this need is covered already, for example).
Supplement provenance: he recommends picking a supplement that’s been tested by a reputable 3rd party, as otherwise turmeric can be quite prone to impurities (which can include lead and arsenic, so, not great).
Contraindications: for some people, curcumin can cause gastrointestinal issues (less likely if taking with meals), and also, it can interact with blood-thinners. While taking aspirin or curcumin alone might help avoid circulatory problems, taking both could increase the bleeding risk for some people, for example. Similarly, if taking curcumin and metformin while diabetic, one must watch out for the combination being too effective at lowering blood sugar levels, and thus causing hypoglycemia instead. Similar deal with blood pressure medications.
There’s more in the video though (yes really; we know we wrote a lot but it’s information-dense), so do check it out:
Click Here If The Embedded Video Doesn’t Load Automatically
Want to know more?
You can also check out our related articles:
Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Black Pepper’s Impressive Anti-Cancer Arsenal (And More)Share This Post
Related Posts
-
Plum vs Persimmon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plum to persimmon, we picked the plum.
Why?
Looking at the macros first, persimmon has 3x the carbs for only the same amount of fiber, on account of which plum has the lower glycemic index, so we’ll go with plum here, though your opinion could vary.
In terms of vitamins, it’s much less subjective: plums have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, E, K, and choline, while persimmon has more vitamin C. So, unless you have scurvy, plums will be the best choice for most people.
In the category of minerals, plums have more copper, magnesium, manganese, and zinc, while persimmon has more calcium, iron, phosphorus, and potassium—thus, a 4:4 tie on minerals.
Adding up the sections gives an overall win for plums, but of course, enjoy either or both; diversity is good!
PS: plums have an extra bonus too; check out the link below…
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← plums kill cancer cells while sparing healthy ones
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Real Benefit Of Genetic Testing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Genetic Testing: Health Benefits & Methods
Genetic testing is an oft-derided American pastime, but there’s a lot more to it than finding out about your ancestry!
Note: because there are relatively few companies offering health-related genetic testing services, and we are talking about the benefits of those services, some of this main feature may seem like an advert.
It’s not; none of those companies are sponsoring us, and if any of them become a sponsor at some point, we’ll make it clear and put it in the clearly-marked sponsor segment.
As ever, our only goal here is to provide science-backed information, to enable you to make your own, well-informed, decisions.
Health genomics & genetic testing
The basic goal of health genomics and genetic testing is to learn:
- What genetic conditions you have
- Clearcut genetic conditions, such as Fragile X syndrome, or Huntington’s disease
- What genetic predispositions you have
- Such as an increased/decreased risk for various kinds of cancer, diabetes, heart conditions, and so forth
- What genetic traits you have
- These may range from “blue eyes” to “superathlete muscle type”
- More specifically, pharmacogenomic information
- For example, “fast caffeine metabolizer” or “clopidogrel (Plavix) non-responder” (i.e., that drug simply will not work for you)
Wait, what’s the difference between health genomics and genetic testing?
- Health genomics is the science of how our genes affect our health.
- Genetic testing can be broadly defined as the means of finding out which genes we have.
A quick snippet…
More specifically, a lot of these services look at which single nucleotide polymorphisms (SNPs, pronounced “snips”) we have. While we share almost all of our DNA with each other (and indeed, with most vertebrates), our polymorphisms are the bits that differ, and are the bits that, genetically speaking, make us different.
So, by looking just at the SNPs, it means we “only” need to look at about 3,000,000 DNA positions, and not our entire genome. For perspective, those 3,000,000 DNA positions make up about 0.1% of our whole genome, so without focusing on SNPs, the task would be 1000x harder.
For example, the kind of information that this sort of testing may give you, includes (to look at some “popular” SNPs):
- rs53576 in the oxytocin receptor influences social behavior and personality
- rs7412 and rs429358 can raise the risk of Alzheimer’s disease by more than 10x
- rs6152 can influence baldness
- rs333 resistance to HIV
- rs1800497 in a dopamine receptor may influence the sense of pleasure
- rs1805007 determines red hair and sensitivity to anesthetics
- rs9939609 triggers obesity and type-2 diabetes
- rs662799 prevents weight gain from high fat diets
- rs12255372 linked to type-2 diabetes and breast cancer
- rs1799971 makes alcohol cravings stronger
- rs17822931 determines earwax, sweating and body odor
- rs1333049 coronary heart disease
- rs1051730 and rs3750344 nicotine dependence
- rs4988235 lactose intolerance
(You can learn about these and more than 100,000 other SNPs at SNPedia.com)
I don’t know what SNPs I have, and am disinclined to look them up one by one!
The first step to knowing, is to get your DNA out of your body and into a genetic testing service. This is usually done by saliva or blood sample. This writer got hers done many years ago by 23andMe and was very happy with that service, but there are plenty of other options.
Healthline did an independent review of the most popular companies, so you might like to check out:
Healthline: Best DNA Testing Kits of 2023
Those companies will give you some basic information, such as “6x higher breast cancer risk” or “3x lower age-related macular degeneration risk” etc.
However, to really get bang-for-buck, what you want to do next is:
- Get your raw genetic data (the companies above should provide it); this will probably look like a big text file full of As, Cs, Gs, and Ts, but it make take another form.
- Upload it to Promethease. When this writer got hers done , the cost was $2; that price has now gone up to a whopping $12.
- You will then get a report that will cross-reference your data with everything known about SNPs, and give a supremely comprehensive, readable-to-the-human-eye, explanation of what it all means for you—from much more specific health risk prognostics, to more trivial things like whether you can roll your tongue or smell decomposed asparagus metabolites in urine.
A note on privacy: anything you upload to Promethease will be anonymized, and/but in doing so, you consent to it going into the grand scientific open-source bank of “things we know about the human genome”, and thus contribute to the overall sample size of genetic data.
In our opinion, it means you’re doing your bit for science, without personal risk. But your opinion may differ, and that’s your decision to make.
Lastly, on the pros and cons of pharmacogenetic testing specifically:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- What genetic conditions you have
-
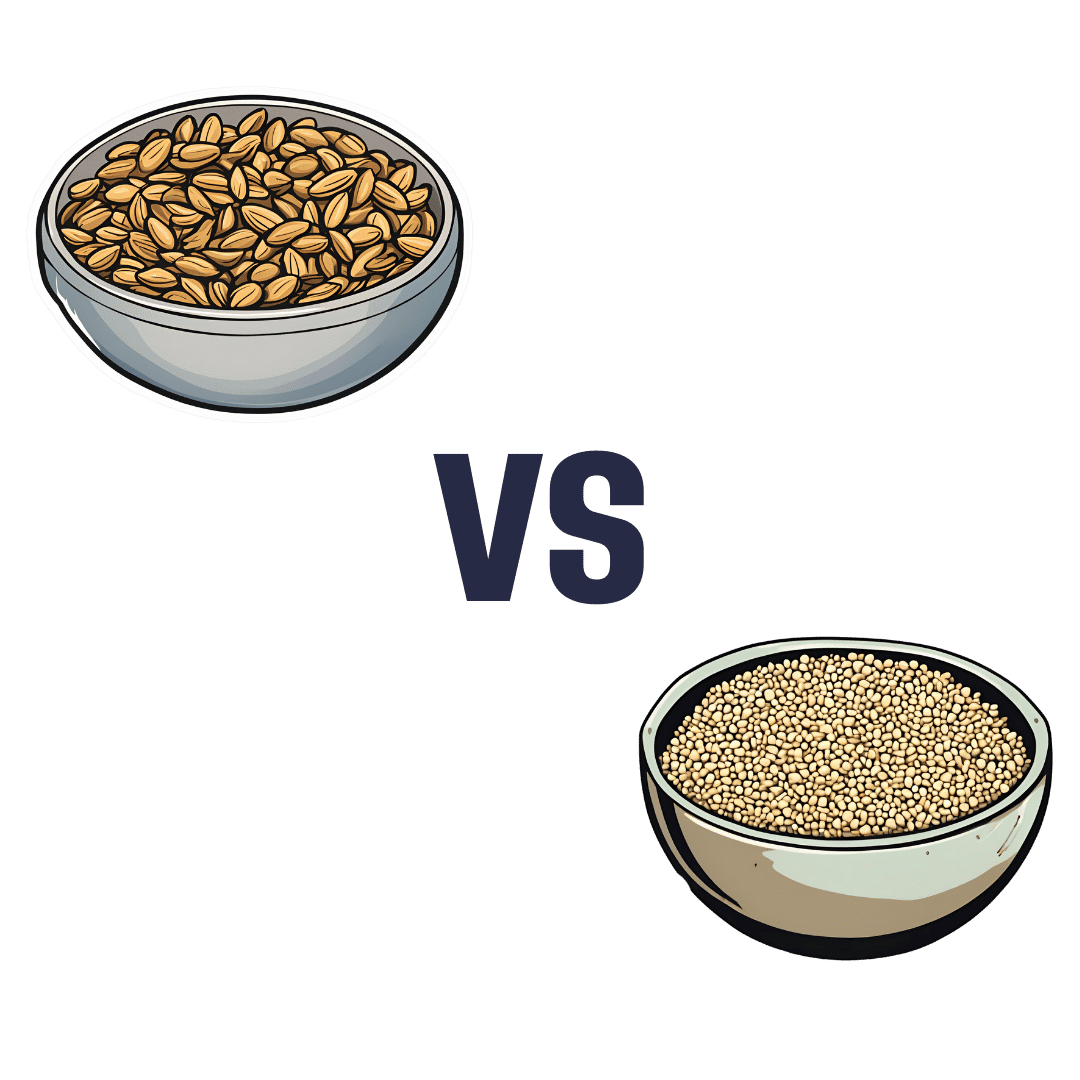
Sunflower Seeds vs Sesame Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sunflower seeds to sesame seeds, we picked the sunflower.
Why?
In moderation, both are very healthy. We say “in moderation” because they’re both about 50% fat and such fats, while vital for life, are generally best enjoyed in small portions. Of that fat, sunflower has the slightly better fat profile; they’re both mostly poly- and monounsaturated fats, but sunflower has 10% saturated fat while sesame has 15%. Aside from fats, sunflower has slightly more protein and sesame has slightly more carbs. While sesame has slightly more fiber, because of the carb profile sunflower still has the lower glycemic index. All in all, a moderate win for sunflower in the macros category.
You may be wondering, with all that discussion of fats, what they’re like for omega-3, and sesame seeds have more omega-3, though sunflower seeds contain it too. Still, a point in sesame’s favor here.
When it comes to vitamins, sunflower has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, and choline, while sesame is not higher in any vitamins.
In the category of minerals, sunflower has more phosphorus, potassium, and selenium, while sesame has more calcium, copper, iron, and zinc. This is nominally a marginal win for sesame, but it should be noted that sunflower is still very rich in copper, iron, and zinc too (but not calcium).
Adding up the categories makes for a moderate win for sunflower seeds, but as ever, enjoy both; diversity is best!
Want to learn more?
You might like to read:
Sunflower Seeds vs Pumpkin Seeds – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: