Tuna vs Catfish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tuna to catfish, we picked the tuna.
Why?
Today in “that which is more expensive and/or harder to get is not necessarily healthier”…
Looking at their macros, tuna has more protein and less fat (and overall, less saturated fat, and also less cholesterol).
In the category of vitamins, both are good but tuna distinguishes itself: tuna has more of vitamins A, B1, B2, B3, B6, and D, while catfish has more of vitamins B5, B9, B12, E, and K. They are both approximately equal in choline, and as an extra note in tuna’s favor (already winning 6:5), tuna is a very good source of vitamin D, while catfish barely contains any. All in all: a moderate, but convincing, win for tuna.
When it comes to minerals, things are clearer still: tuna has more copper, iron, magnesium, phosphorus, potassium, and selenium, while catfish has more calcium, manganese, and zinc. Oh, and catfish is also higher in one other mineral: sodium, which most people in industrialized countries need less of, on average. So, a 6:3 win for tuna, before we even take into account the sodium content (which makes the win for tuna even stronger).
In short: tuna wins the day in every category!
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught (It Makes Quite A Difference)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Build Muscle (Healthily!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Do You Have To Gain?
We have previously promised a three-part series about changing one’s weight:
- Losing weight (specifically, losing fat)
- Gaining weight (specifically, gaining muscle)
- Gaining weight (specifically, gaining fat)
And yes, that last one is also something that some people want/need to do (healthily!), and want/need help with that.
There will be, however, no need for a “losing muscle” article, because (even though sometimes a person might have some reason to want to do this), it’s really just a case of “those things we said for gaining muscle? Don’t do those and the muscle will atrophy naturally”.
Here’s the first part: How To Lose Weight (Healthily!)
While some people will want to lose fat, please do be aware that the association between weight loss and good health is not nearly so strong as the weight loss industry would have you believe:
And, while BMI is not a useful measure of health in general, it’s worth noting that over the age of 65, a BMI of 27 (which is in the high end of “overweight”, without being obese) is associated with the lowest all-cause mortality:
BMI and all-cause mortality in older adults: a meta-analysis
Body weight, muscle mass, and protein:
That BMI of 27, or whatever weight you might wish to be, ignores body composition. You’re probably aware that volume-for-volume, muscle weighs more than fat.
You’re also probably aware that if we’re not careful, we tend to lose muscle as we get older. This is known as age-related sarcopenia:
Protein, & Fighting Sarcopenia
Dr. Gabrielle Lyon, our featured expert in the above article, recommends getting at least 1.6g of protein per kg of body weight per day (Americans, divide your weight in pounds by 2.2 to get your weight in kg).
So for example, if you weigh 165lb, that’s 75kg, that’s 1.6×75=120g of protein per day.
There is an upper limit to how much protein per day is healthy, and that limit is probably around 2g of protein per kg of body weight per day:
Protein: How Much Do We Need, Really?
You may be wondering: should we go for animal or plant protein? In which case, the short version is:
- If you only care about muscle growth, any complete sources of protein are fine
- If you care about your general health too, then avoiding red meat is best, but other common protein sources are all fine
- Unprocessed is (unsurprisingly) better than processed in either case
Longer version: Plant vs Animal Protein: Head to Head
What exercises are best for muscle-building?
Of course, different muscles require different exercises, but for all of them, resistance training is what builds muscle the most, and it’s pretty much impossible to build a lot of muscle otherwise.
Check out: Resistance Is Useful! (Especially As We Get Older)
Prepare to fail!
No, really, prepare to fail. Because while resistance training in general is good for maintaining strong muscles and bones, you will only gain muscle if your current muscle is not enough to do the exercise:
- If you do a heavy resistance exercise without undue difficulty, your muscles will say to each other “Good job, team! That was hard, but luckily we were strong enough; no changes necessary”.
- If you do a heavy resistance exercise to the point where you can no longer do it (called: training to failure), then your muscles will say to each other “Oof, what a task! What we’ve got here is clearly not enough, so we’ll have to add more muscle for next time”.
Safety note: training to failure comes with safety risks. If using free weights or weight machines, please do so under well-trained supervision. If doing it with bodyweight (e.g. press-ups until you can press no more) or resistance bands, please check with your doctor first to ensure this is safe for you.
You can also increase the effectiveness of your resistance training by doing it in a way that “confuses” your muscles, making it harder for them to adapt in the moment, and thus forcing them to adapt more in the long term (e.g. get bigger and stronger):
HIIT, But Make It HIRT: High Intensity Resistance Training
Make time for recovery
While many kinds of exercise can be done daily, exercise to build muscle(s) means at the very least resting that muscle (or muscle group) the next day.
For this reason, a lot of bodybuilders have for example a week’s schedule that might look like:
- Monday: Upper body training
- Wednesday: Lower body training
- Friday: Core strength training
…and rest on other days. This gives most muscles a full week of recovery, and every muscle at least 48 hours of recovery.
Note: bodybuilders, like children (who are also doing a lot of body-building, in their own way) need more sleep in order to allow for this recovery and growth to occur. Serious bodybuilders often aim for 12 hours sleep per day. This might be impractical, undesirable, or even impossible for some people, but it’s a factor to be borne in mind and not forgotten.
See also:
Overdone It? How To Speed Up Recovery After Exercise (According To Actual Science)
Anything else that can (safely and healthily) be done to promote muscle growth?
There are a lot of supplements on the market; some are healthy and helpful, other not so much. Here are some we’ve written about:
- What To Eat, Take, And Do Before A Workout
- Creatine: Very Different For Young & Old People
- Ginseng: Exercising With Less Soreness!
- Taurine’s Benefits For Heart Health And More
- Topping Up Testosterone? What To Consider
Take care!
Share This Post
-
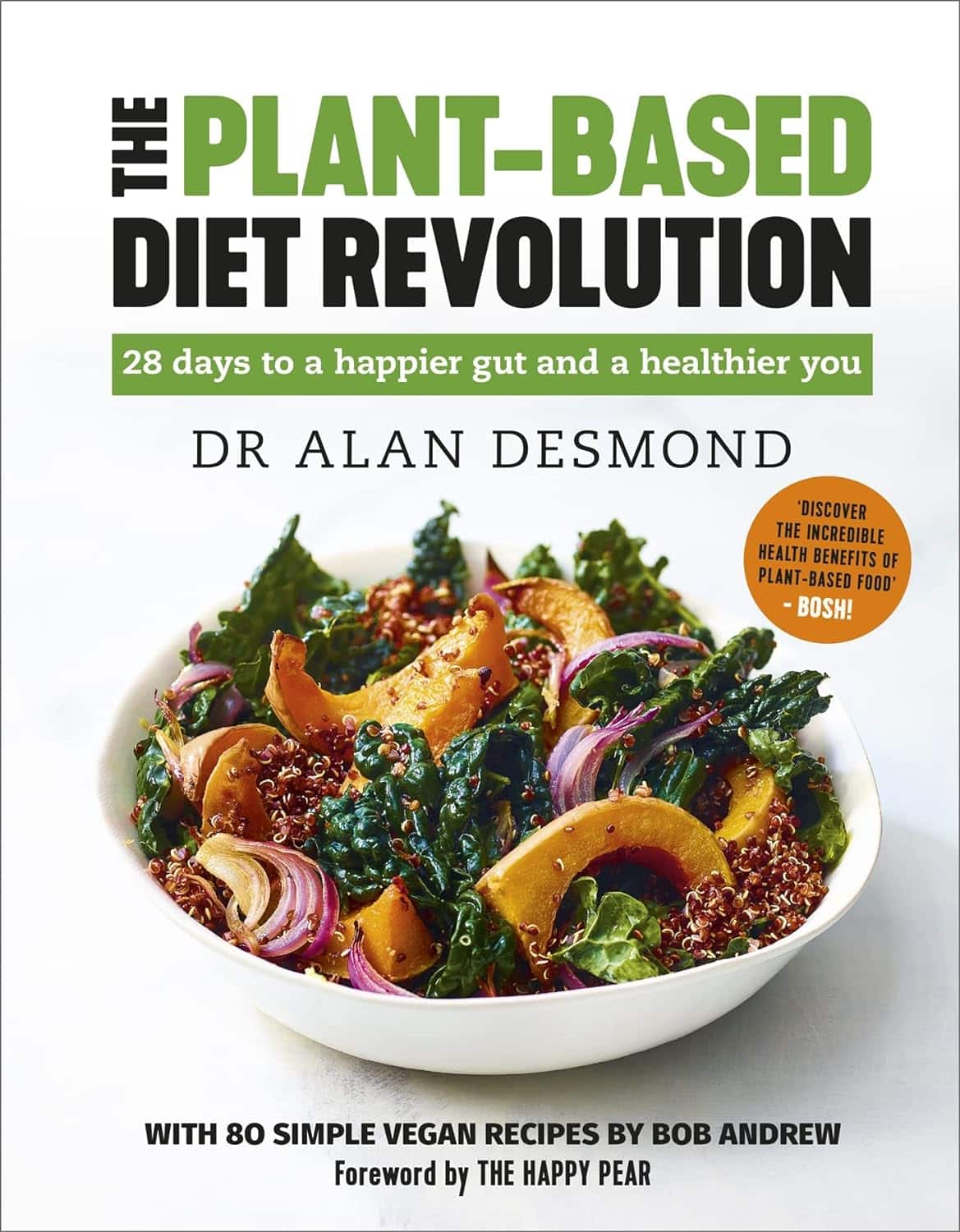
The Plant-Based Diet Revolution – by Dr. Alan Desomond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is this just another gut-healthy cooking guide? Not entirely…
For a start, it’s not just about giving you a healthy gut; it also covers a healthy heart and a healthy brain. There’s lots of science in here!
It’s also aimed as a transitional guide to eating more plants and fewer animal products, if you so choose. And if you don’t so choose, at least having the flexibility to cook both ways.
The recipes themselves (organized into basics, breakfasts, lunches, mains, desserts) are clear and easy while also being calculated to please readers (and their families) who are used to eating more meat. There are, for instance, plenty of healthy proteins, healthy fats, and comfort foods.
The “28 days” of the title refers to a meal plan using the recipes from the book; it’s not a big feature of the book though, so use it or don’t, but the cooking advice itself is more than worth the price of the book and the recipes are certainly great.
Bottom line: if you’re thinking of taking a “Meatless Mondays” approach to making your diet healthier, this book can help you do that in style!
Click here to check out The Plant-Based Diet Revolution, and upgrade your culinary repertoire!
Share This Post
-
Your Brain On (And Off) Estrogen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Lisa Mosconi. She’s a professor of Neuroscience in Neurology and Radiology, and is one of the 1% most influential scientists of the 21st century. That’s not a random number or an exaggeration; it has to do with citation metrics collated over 20 years:
A standardized citation metrics author database annotated for scientific field
What does she want us to know?
Women’s brains age differently from men’s
This is largely, of course, due to menopause, and as such is a generalization, but it’s a statistically safe generalization, because:
- Most women go through menopause—and most women who don’t, avoid it by dying pre-menopause, so the aging also does not occur in those cases
- Menopause is very rarely treated immediately—not least of all because menopause is diagnosed officially when it has been one year since one’s last period, so there’s almost always a year of “probably” first, and often numerous years, in the case of periods slowing down before stopping
- Menopausal HRT is great, but doesn’t completely negate that menopause occurred—because of the delay in starting HRT, some damage can be done already and can take years to reverse.
Medicated and unmedicated menopause proceed very differently from each other, and this fact has historically caused obfuscation of a lot of research into age-related neurodegeneration.
For example, it is well-established that women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
Superficially, one might conclude “estrogen is to blame” or maybe “the xx-chromosomal karyotype is to blame”.
The opposite, however, is true with regard to estrogen—estrogen appears to be a protective factor in women’s neurological health, which is why increased neurodegeneration occurs when estrogen levels decline (for example, in menopause).
For a full rundown on this, see:
Alzheimer’s Sex Differences May Not Be What They Appear
It’s not about the extra X
Dr. Mosconi examines this in detail in her book “The XX Brain”. To summarize and oversimplify a little: the XX karyotype by itself makes no difference, or more accurately, the XY karyotype by itself makes no difference (because biologically speaking, female physiological attributes are more “default” than male ones; it is only 12,000ish* years of culture that has flipped the social script on this).
*Why 12,000ish years? It’s because patriarchalism largely began with settled agriculture, for reasons that are fascinating but beyond the scope of this article, which is about health science, not archeology.
The topic of “which is biologically default” is relevant, because the XY karyotype (usually) informs the body “ignore previous instructions about ovaries, and adjust slightly to make them into testes instead”, which in turn (usually) results in a testosterone-driven system instead of an estrogen-driven system. And that is what makes the difference to the brain.
One way we can see that it’s about the hormones not the chromosomes, is in cases of androgen insensitivity syndrome, in which the natal “congratulations, it’s a girl” pronouncement may later be in conflict with the fact it turns out she had XY chromosomes all along, but the androgenic instructions never got delivered successfully, so she popped out with fairly typical female organs. And, relevantly for Dr. Mosconi, a typically female brain that will age in a typically female fashion, because it’s driven by estrogen, regardless of the Y-chromosome.
The good news
The good news from all of this is that while we can’t (with current science, anyway) do much about our chromosomes, we can do plenty about our hormones, and also, the results of changes in same.
Remember, Dr. Mosconi is not an endocrinologist, nor a gynecologist, but a neurologist. As such, she makes the case for how a true interdisciplinary team for treating menopause should not confined to the narrow fields usually associated with “bikini medicine”, but should take into account that a lot of menopause-related changes are neurological in nature.
We recently reviewed another book by Dr. Mosconi:
The Menopause Brain – by Dr. Lisa Mosconi
…and as we noted there, many sources will mention “brain fog” as a symptom of menopause, Dr. Mosconi can (and will) point to a shadowy patch on a brain scan and say “that’s the brain fog, there”.
And so on, for other symptoms that are often dismissed as “all in your head”, as though that’s a perfectly acceptable place for problems to be.
This is critical, because it’s treating real neurological things as the real things they are.
Dr. Mosconi’s advice, beyond HRT
Dr. Mosconi notes that brain health tends to dip during perimenopause but often recovers, showing the brain’s resilience to hormonal shifts. As such, all is not lost if for whatever reason, hormone replacement therapy isn’t a viable option for you.
Estrogen plays a crucial role in brain energy, and women’s declining estrogen levels during menopause increase the need for antioxidants to protect brain health—something not often talked about.
Specifically, Dr. Mosconi tells us, women need more antioxidants and have different metabolic responses to diets compared to men.*
*Yes, even though men usually have negligible estrogen, because their body (and thus brain, being also part of their body) is running on testosterone instead, which is something that will only happen if either you are producing normal male amounts of testosterone (requires normal male testes) or you are taking normal male amounts of testosterone (requires big bottles of testosterone; this isn’t the kind of thing you can get from a low dose of testogel as sometimes prescribed as part of menopausal HRT to perk your metabolism up).
Note: despite women being a slight majority on Earth, and despite an aging population in wealthy nations, meaning “a perimenopausal woman” is thus the statistically average person in, for example, the US, and despite the biological primacy of femaleness… Medicine still mostly looks to men as the “default person”, which in this case can result in seriously low-balled estimates of what antioxidants are needed.
In terms of supplements, therefore, she recommends:
- Antioxidants: key for brain health, especially in women. Rich sources include fruits (especially berries) and vegetables. Then there’s the world’s most-consumed antioxidant, which is…
- Coffee: Italian-style espresso has the highest antioxidant power. Adding a bit of fat (e.g. oat milk) helps release caffeine more slowly, reducing jitters. Taking it alongside l-theanine also “flattens the curve” and thus improves its overall benefits.
- Flavonoids: important for both men and women but particularly essential for women. Found in many fruits and vegetables.
- Chocolate: dark chocolate is an excellent source of antioxidants and flavonoids!
- Turmeric: a natural neuroprotectant with anti-inflammatory properties, best boosted by taking with black pepper, which improves absorption as well as having many great qualities of its own.
- B Vitamins: B6, B9, and B12 are essential for anti-aging and brain health; deficiency in B6 is rare, while deficiency in B9 (folate) and especially B12 is very common later in life.
- Vitamins C & E: important antioxidants, but caution is needed with fat-soluble vitamins to avoid toxicity.
- Omega-3s: important for brain health; can be consumed in the diet, but supplements may be necessary.
- Caution with zinc: zinc can support immunity and endocrine health (and thus, indirectly, brain health) but may be harmful in excess, particularly for brain health.
- Probiotics & Prebiotics: beneficial for gut health, and in Dr. Mosconi’s opinion, hard to get sufficient amounts from diet alone.
For more pointers, you might want to check out the MIND diet, that is to say, the “Mediterranean-DASH Intervention for Neurodegenerative Delay” upgrade to make the Mediterranean diet even brain-healthier than it is by default:
Four Ways To Upgrade The Mediterranean Diet
Want to know more from Dr. Mosconi?
Here’s her TED talk:
Click Here If The Embedded Video Doesn’t Load Automatically!
Enjoy!
Share This Post
Related Posts
-
The Metabolism Reset Diet – by Alan Christianson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The liver is an incredible organ that does a very important job, but what’s not generally talked about is how we can help it… Beyond the obvious “try to not poison it too much with alcohol, tobacco, etc”. But what can we do that’s actually positive for it?
That’s what Alan Christianson offers in this book.
Now, usually when someone speaks of a “four week cleanse” as this book advertises on its front cover, it’s a lot of bunk. The liver cleanses itself, and the liver and kidneys between them (along with some other organs and processes) detoxify your body for you. No amount of celery juice will do that. However, this book does better than that:
What it’s about, is not really about trying to do a “detox” at all, so much as supporting your liver function by:
- Giving your liver what it needs to regenerate (mostly: protein)
- Not over-taxing your liver while it does so
The liver is a self-regenerating organ (the mythological story of Prometheus aside, here in real life it can regenerate up to 80% of itself, given the opportunity), so whatever the current state of your liver, it’s probably not too late to fix it.
Maybe you’ve been drinking a little too much, or maybe you’ve been taking some meds that have hobbled it a bit (some medications strain the liver rather), or maybe your diet hasn’t been great. Christianson invites you to draw a line under that, and move forwards:
The book gives an overview of the science involved, and explains about the liver’s role in metabolism (hence the promised weight loss benefits) and our dietary habits’ impact on liver function. This is about what we eat, and also about when we eat it, and how and when our body metabolizes that.
Christianson also provides meal ideas and recipes. If we’re honest (and we always are), the science/principles part of the book are worth a lot more than the meal-plan part of the book, though.
In short: a great book for understanding how the liver works and how we can help it do its job effectively.
Click here to check out “The Metabolism Reset Diet” on Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Some Friendships Last And Others Don’t
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Friendships matter a lot, playing a significant role in our wellbeing, physical as well as mental. They bring additional meaning to our lives, help us cope with setbacks, and hopefully will be at our side through the highs and lows of life. And yet, for something that’s in principle good for everyone involved, there can be problems:
Friend to the end?
Firstly, some people find it harder to make (and then further deepen) friendships with others, which can be for a whole host of reasons.
Approaching new people can feel intimidating, but it’s a common struggle. Research shows that people often underestimate how much others enjoy their company, a phenomenon known as the “liking gap.” By reminding ourselves that others are likely to appreciate our presence and expecting to be well-received (the “acceptance prophecy”), we can approach social interactions with greater confidence.
As relationships grow, they often deepen through companionship and closeness:
- Companionship arises from shared hobbies, interests, or values, and it builds rapport.
- Closeness involves sharing thoughts, feelings, and experiences, which can build intimacy together.
An important key to these is consistency, which—whether through regular chats, honoring plans, or showing support—helps strengthen bonds, even in long-distance friendships (something often considered a barrier to closeness).
Even the strongest friendships can face challenges, of course. Conflicts may arise from a lack of support during difficult moments, or worse, betrayal. Or it could all be a misunderstanding. These situations are best addressed through honest, non-judgmental conversations. Avoiding defensiveness or accusations, and instead focusing on sharing feelings and understanding the other person’s perspective, can turn these tough discussions into opportunities for growth and stronger connections.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Self-Compassion – by Dr. Kristin Neff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of people struggle with self-esteem, and depending on one’s surrounding culture, it can even seem socially obligatory to be constantly valuing oneself highly (or else, who else will if we do not?). But, as Dr. Neff points out, there’s an inherent problem with reinforcing for oneself even a positive message like “I am smart, strong, and capable!” because sometimes all of us have moments of being stupid, weak, and incapable (occasionally all three at once!), which places us in a position of having to choose between self-deceit and self-deprecation, neither of which are good.
Instead, Dr. Neff advocates for self-compassion, for treating oneself as one (hopefully) would a loved one—seeing their/our mistakes, weaknesses, failures, and loving them/ourself anyway.
She does not, however, argue that we should accept just anything from ourselves uncritically, but rather, we identify our mistakes, learn, grow, and progress. So not “I should have known better!”, nor even “How was I supposed to know?!”, but rather, “Now I have learned a thing”.
The style of the book is quite personal, as though having a heart-to-heart over a hot drink perhaps, but the format is organized and progresses naturally from one idea to the next, taking the reader to where we need to be.
Bottom line: if you have trouble with self-esteem (as most people do), then that’s a trap that there is a way out of, and it doesn’t require being perfect or lowering one’s standards, just being kinder to oneself along the way—and this book can help inculcate that.
Click here to check out Self-Compassion, and indeed be kind to yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: