When BMI Doesn’t Measure Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When BMI Doesn’t Quite Measure Up
Last month, we did a “Friday Mythbusters” edition of 10almonds, tackling many of the misconceptions surrounding obesity. Amongst them, we took a brief look at the usefulness (or lack thereof) of the Body Mass Index (BMI) scale of weight-related health for individuals. By popular subscriber request, we’re now going to dive a little deeper into that today!
The wrong tool for the job
BMI was developed as a tool to look at large-scale demographic trends, stemming from a population study of white European men, who were for the purpose of the study (the widescale health of the working class in that geographic area in that era), considered a reasonable default demographic.
In other words: as a system, it’s now being used in a way it was never made for, and the results of that misappropriation of an epidemiological tool for individual health are predictably unhelpful.
If you want to know yours…
Here’s the magic formula for calculating your BMI:
- Metric: divide your weight in kilograms by your height in square meters
- Imperial: divide your weight in pounds by your height in square inches and then multiply by 703
“What if my height doesn’t come in square meters or square inches, because it’s a height, not an area?”
We know. Take your height and square it anyway. If this seems convoluted and arbitrary, yes, it is.
But!
While on the one hand it’s convoluted and arbitrary… On the other hand, it’s also a gross oversimplification. So, yay for the worst of both worlds?
If you don’t want to grab a calculator, here’s a quick online tool to calculate it for you.
So, how did you score?
According to the CDC, a BMI score…
- Under 18.5 is underweight
- 18.5 to 24.9 is normal
- 25 to 29.9 is overweight
- 30 and over is obese
And, if we’re looking at a representative sample of the population, where the representation is average white European men of working age, that’s not a bad general rule of thumb.
For the rest of us, not so representative
BMI is a great and accurate tool as a rule of thumb, except for…
Women
An easily forgotten demographic, due to being a mere 51% of the world’s population, women generally have a higher percentage of body fat than men, and this throws out BMI’s usefulness.
If pregnant or nursing
A much higher body weight and body fat percentage—note that these are two things, not one. Some of the extra weight will be fat to nourish the baby; some will be water weight, and if pregnant, some will be the baby (or babies!). BMI neither knows nor cares about any of these things. And, this is a big deal, because BMI gets used by healthcare providers to judge health risks and guide medical advice.
People under the age of 16 or over the age of 65
Not only do people below and above those ages (respectively) tend to be shorter—which throws out the calculations and mean health risks may increase before the BMI qualifies as overweight—but also:
- BMI under 23 in people over the age of 65 is associated with a higher health risk
- A meta-analysis showed that a BMI of 27 was the best in terms of decreased mortality risk for the over-65 age group
This obviously flies in the face of conventional standards regards BMI—as you’ll recall from the BMI brackets we listed above.
Read the science: BMI and all-cause mortality in older adults: a meta-analysis
Athletic people
A demographic often described in scientific literature as “athletes”, but that can be misleading. When we say “athletes”, what comes to mind? Probably Olympians, or other professional sportspeople.
But also athletic, when it comes to body composition, are such people as fitness enthusiasts and manual laborers. Which makes for a lot more people affected by this!
Athletic people tend to have more lean muscle mass (muscle weighs more than fat), and heavier bones (can’t build strong muscles on weak bones, so the bones get stronger too, which means denser)… But that lean muscle mass can actually increase metabolism and help ward off many of the very same things that BMI is used as a risk indicator for (e.g. heart disease, and diabetes). So people in this category will actually be at lower risk, while (by BMI) getting told they are at higher risk.
If not white
Physical characteristics of race can vary by more than skin color, relevant considerations in this case include, for example:
- Black people, on average, not only have more lean muscle mass and less fat than white people, but also, have completely different risk factors for diseases such as diabetes.
- Asian people, on average, are shorter than white people, and as such may see increased health risks before BMI qualifies as overweight.
- Hispanic people, on average, again have different physical characteristics that throw out the results, in a manner that would need lower cutoffs to be even as “useful” as it is for white people.
Further reading on this: BMI and the BIPOC Community
In summary:
If you’re an average white European working-age man, BMI can sometimes be a useful general guide. If however you fall into one or more of the above categories, it is likely to be inaccurate at best, if not outright telling the opposite of the truth.
What’s more useful, then?
For heart disease risk and diabetes risk both, waist circumference is a much more universally reliable indicator. And since those two things tend to affect a lot of other health risks, it becomes an excellent starting point for being aware of many aspects of health.
Pregnancy will still throw off waist circumference a little (measure below the bump, not around it!), but it will nevertheless be more helpful than BMI even then, as it becomes necessary to just increase the numbers a little, according to gestational month and any confounding factors e.g. twins, triplets, etc. Ask your obstetrician about this, as it’s beyond the scope of today’s newsletter!
As to what’s considered a risk:
- Waist circumference of more than 35 inches for women
- Waist circumference of more than 40 inches for men
These numbers are considered applicable across demographics of age, sex, ethnicity, and lifestyle.
There are more options than just waist circumference though; we delve into them in detail here:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Be 7.5x More Likely To Develop Chronic Fatigue Syndrome
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what is it?
Many more people have chronic fatigue, which is the symptom of being exhausted all the time, than have chronic fatigue syndrome (CFS) which is the illness of myalgic encephalomyelitis (ME).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
The chronic disease pipeline
While it had been strongly suspected that COVID infection could lead to CFS, with long COVID having chronic fatigue as one of its characteristic symptoms, a research team led by Dr. Suzanne Vernon has now established the nature of the relationship.
It was a large (n=13,224) longitudinal observational cohort study of people with no pre-existing ME/CFS, grouped according to their COVID infection status:
- acute infected, enrolled within 30 days of infection or enrolled as uninfected who became infected (n=4,515)
- post-acute infected, enrolled greater than 30 days after infection (n=7,270)
- uninfected (n=1,439).
(to be clear, that last means “never infected”, or else they would be in group 2)
Note: people who had COVID and were hospitalized for it were excluded from the study, so this risk is the risk represented by even just more “moderate” infections.
What they found:
❝The proportion of all RECOVER-Adult participants that met criteria for ME/CFS following SARS-CoV-2 infection was 4.5% (531 of 11,785) compared to 0.6% (9 of 1439) in uninfected participants.❞
There are then different numbers if we look per 100 person-years, as the study also did—in which case, we get a re-modelled increase in risk of 5x instead of 7.5x, but a) that’s still not good b) the “here-and-now” figures of 4.5% vs 0.6% are also relevant.
Read in full: Incidence and Prevalence of Post-COVID-19 Myalgic Encephalomyelitis: A Report from the Observational RECOVER-Adult Study
The killer nobody wants to talk about anymore
Of course, as we all know the pandemic is over, because politicians declared it so, which is very reassuring.
Nevertheless, COVID is currently the still 4th leading cause of death in the US, placing it higher than stroke, Alzheimer’s, diabetes, and others.
See also: Emergency or Not, Covid Is Still Killing People. Here’s What Doctors Advise to Stay Safe
So, while it’s very good to take care of our hearts, brains, blood sugars, and so forth, let’s at the very least continue to keep on top of our vaccinations, avoid enclosed crowded spaces where possible, etc.
And for extra boosts to one’s chances: Why Some People Get Sick More (And How To Not Be One Of Them)
What if I do get (or already have) long COVID and/or ME/CFS?
Well, that is definitely going to suck, but there are still some things that can be done.
Here’s a big one: How To Eat To Beat Chronic Fatigue ← this will not, of course, cure you, but it’s a way of getting maximum nutrition for minimum effort, given that for someone with chronic fatigue, effort is a very finite resource that must be used sparingly
Finally, here are some further resources:
Support For Long COVID & Chronic Fatigue
Take care!
Share This Post
-
The 7 Approaches To Pain Management
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More Than One Way To Kill Pain
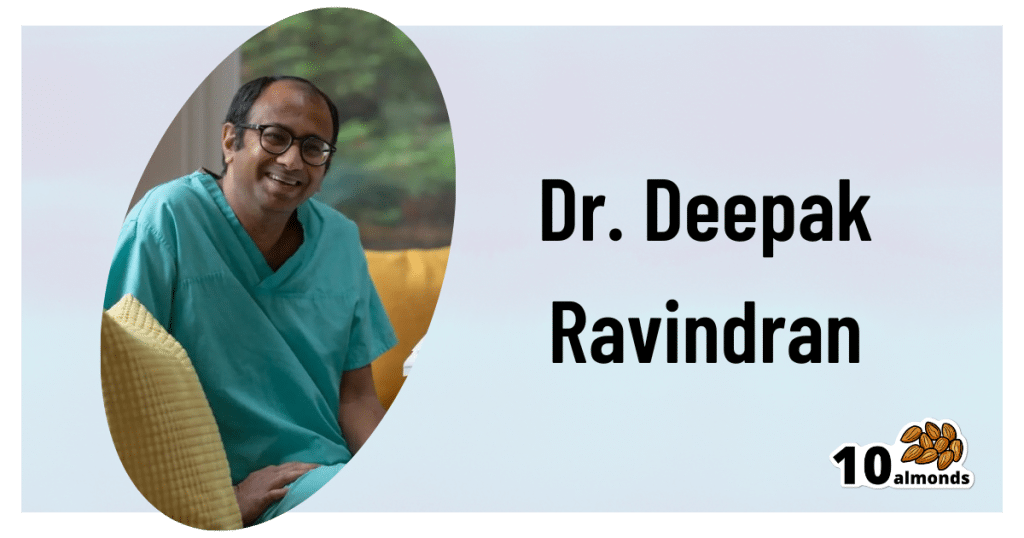
This is Dr. Deepak Ravindran (MD, FRCA. FFPMRCA, EDRA. FIPP, DMSMed). He has decades of experience and is a specialist in acute and chronic pain management, anesthesia, musculoskeletal medicine, and lifestyle medicine.
A quick catch-up, first:
We’ve written about chronic pain management before:
Managing Chronic Pain (Realistically!)
As well as:
Science-Based Alternative Pain Relief
Dr. Ravindran’s approach
Dr. Ravindran takes a “trauma-informed care” approach to his professional practice, and recommends the same for others.
In a nutshell, this means starting from a position of not “what’s wrong with you?”, but rather “what happened to you?”.
This seemingly subtle shift is important, because it means actually dealing with a person’s issues, instead of “take one of these and call my secretary next month”. Read more:
Pain itself can be something of a many-headed hydra. Dr. Ravindran’s approach is equally many-headed; specifically, he has a 7-point plan:
Medications
Dr. Ravindran sees painkillers (and a collection of other drugs, like antidepressants and muscle relaxants) as a potential means to an end worth exploring, but he doesn’t expect them to be the best choice for everyone, and nor does he expect them to be a cure-all. Neither should we. He also advises being mindful of the drawbacks and potential complications of these drugs, too.
Interventions
Sometimes, surgery is the right choice. Sometimes it isn’t. Often, it will change a life—one way or the other. Similar to with medications, Dr. Ravindran is very averse to a “one size fits all” approach here. See also:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Neuroscience and stress management
Often a lot of the distress of pain is not just the pain itself, but the fear associated with it. Will it get worse if I move wrong or eat the wrong thing? How long will it last? Will it ever get better? Will it get worse if I do nothing?. Dr. Ravindran advises tackling this, with the same level of importance as the pain itself. Here’s a good start:
Stress, And Building Psychological Resilience
Diet and the microbiome
Many chronic illnesses are heavily influenced by this, and Dr. Ravindran’s respect for lifestyle medicine comes into play here. While diet might not fix all our ills, it certainly can stop things from being a lot worse. Beyond the obvious “eat healthily” (Mediterranean diet being a good starting point for most people), he also advises doing elimination tests where appropriate, to screen out potential flare-up triggers. You also might consider:
Four Ways To Upgrade The Mediterranean Diet
Sleep
“Get good sleep” is easy advice for those who are not in agonizing pain that sometimes gets worse from staying in the same position for too long. Nevertheless, it is important, and foundational to good health. So it’s important to explore—whatever limitations one might realistically have—what can be done to improve it.
If you can only sleep for a short while at a time, you may get benefit from this previous main feature of ours:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Exercise and movement
The trick here is to move little and often; without overdoing it, but without permitting loss of mobility either. See also:
The Doctor Who Wants Us To Exercise Less, And Move More
Therapies of the mind and body
This is about taking a holistic approach to one’s wellness. In Dr. Ravindran’s words:
❝Mind-body therapies are often an extremely sensitive topic about which people hold very strong opinions and sometimes irrational beliefs.
Some, like reiki and spiritual therapy and homeopathy, have hardly any scientific evidence to back them up, while others like yoga, hypnosis, and meditation/mindfulness are mainstream techniques with many studies showing the benefits, but they all work for certain patients.❞
In other words: evidence-based is surely the best starting point, but if you feel inclined to try something else and it works for you, then it works for you. And that’s a win.
Want to know more?
You might like his book…
The Pain-Free Mindset: 7 Steps to Taking Control and Overcoming Chronic Pain
He also has a blog and a podcast.
Take care!
Share This Post
-
Where to Get Turmeric?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
“I liked the info on Turmeric. The problem for me is that I do not like black pepper which should be ingested with the turmeric for best results. Is black pepper sold in capsule form?”
Better than just black pepper being sold in capsule form, it’s usually available in the same capsules as the turmeric. As in: if you buy turmeric capsules, there is often black pepper in them as well, for precisely that reason. Check labels, of course, but here’s an example on Amazon.
“I would like to read more on loneliness, meetup group’s for seniors. Thank you”
Well, 10almonds is an international newsletter, so it’s hard for us to advise about (necessarily: local) meetup groups!
But a very popular resource for connecting to your local community is Nextdoor, which operates throughout the US, Canada, Australia, and large parts of Europe including the UK.
In their own words:
Get the most out of your neighborhood with Nextdoor
It’s where communities come together to greet newcomers, exchange recommendations, and read the latest local news. Where neighbors support local businesses and get updates from public agencies. Where neighbors borrow tools and sell couches. It’s how to get the most out of everything nearby. Welcome, neighbor.
Curious? Click here to check it out and see if it’s of interest to you
“It was superb !! Just loved that healthy recipe !!! I would love to see one of those every day, if possible !! Keep up the fabulous work !!!”
We’re glad you enjoyed! We can’t promise a recipe every day, but here’s one just for you:
! Share This Post
Related Posts
-
Steps vs Cardio | Which is Best for Fat Loss, Health, & Performance?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Move more”, they say; but does it matter how quickly?
Use it or lose it
For general performance:
- More steps per day do offer slight aerobic benefits but do not significantly improve endurance.
- Higher-intensity cardio (ideally, HIIT) is essential for improving aerobic fitness.
- Training should match endurance goals (e.g. long-distance running vs team sports vs whatever it is that you care about for you).
For general health:
- Both cardio and step tracking reduce mortality risk and improve longevity.
- 2–3 hours of cardio per week provides most health benefits, with diminishing returns after 8 hours per week.
- 10,000+ steps/day is optimal, but 5,000+ steps/day still benefits health. And, not mentioned in this video, but really (per science) there seem to be diminishing returns after about 8,000 steps per day.
Fun fact: the reason it’s 10,000 steps per day that everyone talks about as the default goal, is just because the Japanese person who popularized it noted that the kanji for 10,000 looks a bit like a walking person: 万
For fat loss:
- Both step tracking and cardio do help.
- Step tracking better reflects total daily movement, while cardio burns calories in sessions—but if it’s not HIIT, there is likely to be a compensatory metabolic slump afterwards.
- High-intensity cardio increases fatigue, which may impact resistance training and diet adherence.
- Excessive endurance training can slightly inhibit muscle growth, but low-intensity steps have minimal interference.
So for fat loss, it’s best to get those steps in, and throw in a few HIIT sessions per week, with adequate recovery time between them.
For more on all of these things, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Do HIIT (Without Wrecking Your Body)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Get Your First Pull-Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pull-ups are a great compound exercise that works most of the upper body. However, it can be frustrating for many, if unable to do more than dangle and struggle while not going anywhere. That’s not actually bad, by the way! Of course it’s not great athletic performance, but in terms of exercise, “dangling and struggling while not going anywhere” is an isometric exercise that has plenty of benefits of its own. However, for those who would rather go up in the world, personal trainer Meg Gallagher shows the way:
The Only Way Is Up?
Gallagher offers a few methods; the first is simply an improvement on the “dangling and struggling while not going anywhere” method, but doing it with good form. It’s called the…
Hollow body hold:
- Hang from the bar with legs and feet together.
- Maintain a posterior pelvic tilt (i.e. don’t let your hips roll forwards, and don’t let your butt stick out more than is necessary by mere virtue of having a butt)
- Engage your core by shortening the space between your ribs and pelvis.
- Turn on your abs and lats, with your head slightly behind the bar.
- Practice the hollow body hang instead of dead hangs to build grip and core strength.
Another method is now moving on from the hollow body hold, and shows that in fact, up is not the only way. It’s called…
Negative pull-ups:
- Jump up to get your chin over the bar, then slowly lower yourself in a controlled manner.
- Prioritize negative pull-ups over other exercises to build strength.
- You can use modifications like resistance bands or feet assistance if necessary to extend the duration of your negative pull-up, but these are “crutches”, so try to move on from them as soon as you reasonably can—same if your gym has an “assisted pull-up” machine, consisting of a moving platform with a variable counterweight, mimicking how a pull-up would feel if your body were lighter.
- Practice resisting throughout the entire range of motion.
To give a sense of direction, Gallagher offers the following program:
- On day 1, test how long you can resist the negative pull-up (e.g., 10 seconds).
- For each session, multiply your time by 2 (e.g., 10 seconds × 2 = 20 seconds total).
- Break the total volume into as many sets as needed (e.g., 2 sets of 10 seconds or 4 sets of 5 seconds).
- After each session, add 2 seconds to the total volume for the next session.
- Aim for 3 sessions per week for 3–4 weeks, increasing by 2 seconds each session.
- When you reach about 25 seconds, you should be close to performing your first pull-up.
For more on all of this, plus a few other things to try, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 7 Approaches To Pain Management
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More Than One Way To Kill Pain
This is Dr. Deepak Ravindran (MD, FRCA. FFPMRCA, EDRA. FIPP, DMSMed). He has decades of experience and is a specialist in acute and chronic pain management, anesthesia, musculoskeletal medicine, and lifestyle medicine.
A quick catch-up, first:
We’ve written about chronic pain management before:
Managing Chronic Pain (Realistically!)
As well as:
Science-Based Alternative Pain Relief
Dr. Ravindran’s approach
Dr. Ravindran takes a “trauma-informed care” approach to his professional practice, and recommends the same for others.
In a nutshell, this means starting from a position of not “what’s wrong with you?”, but rather “what happened to you?”.
This seemingly subtle shift is important, because it means actually dealing with a person’s issues, instead of “take one of these and call my secretary next month”. Read more:
Pain itself can be something of a many-headed hydra. Dr. Ravindran’s approach is equally many-headed; specifically, he has a 7-point plan:
Medications
Dr. Ravindran sees painkillers (and a collection of other drugs, like antidepressants and muscle relaxants) as a potential means to an end worth exploring, but he doesn’t expect them to be the best choice for everyone, and nor does he expect them to be a cure-all. Neither should we. He also advises being mindful of the drawbacks and potential complications of these drugs, too.
Interventions
Sometimes, surgery is the right choice. Sometimes it isn’t. Often, it will change a life—one way or the other. Similar to with medications, Dr. Ravindran is very averse to a “one size fits all” approach here. See also:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Neuroscience and stress management
Often a lot of the distress of pain is not just the pain itself, but the fear associated with it. Will it get worse if I move wrong or eat the wrong thing? How long will it last? Will it ever get better? Will it get worse if I do nothing?. Dr. Ravindran advises tackling this, with the same level of importance as the pain itself. Here’s a good start:
Stress, And Building Psychological Resilience
Diet and the microbiome
Many chronic illnesses are heavily influenced by this, and Dr. Ravindran’s respect for lifestyle medicine comes into play here. While diet might not fix all our ills, it certainly can stop things from being a lot worse. Beyond the obvious “eat healthily” (Mediterranean diet being a good starting point for most people), he also advises doing elimination tests where appropriate, to screen out potential flare-up triggers. You also might consider:
Four Ways To Upgrade The Mediterranean Diet
Sleep
“Get good sleep” is easy advice for those who are not in agonizing pain that sometimes gets worse from staying in the same position for too long. Nevertheless, it is important, and foundational to good health. So it’s important to explore—whatever limitations one might realistically have—what can be done to improve it.
If you can only sleep for a short while at a time, you may get benefit from this previous main feature of ours:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Exercise and movement
The trick here is to move little and often; without overdoing it, but without permitting loss of mobility either. See also:
The Doctor Who Wants Us To Exercise Less, And Move More
Therapies of the mind and body
This is about taking a holistic approach to one’s wellness. In Dr. Ravindran’s words:
❝Mind-body therapies are often an extremely sensitive topic about which people hold very strong opinions and sometimes irrational beliefs.
Some, like reiki and spiritual therapy and homeopathy, have hardly any scientific evidence to back them up, while others like yoga, hypnosis, and meditation/mindfulness are mainstream techniques with many studies showing the benefits, but they all work for certain patients.❞
In other words: evidence-based is surely the best starting point, but if you feel inclined to try something else and it works for you, then it works for you. And that’s a win.
Want to know more?
You might like his book…
The Pain-Free Mindset: 7 Steps to Taking Control and Overcoming Chronic Pain
He also has a blog and a podcast.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: