Herring vs Sardines – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing herring to sardine, we picked the sardines.
Why?
In terms of macros, they are about equal in protein and fat, but herring has about 2x the saturated fat and about 2x the cholesterol. So, sardines win this category easily.
When it comes to vitamins, herring has more of vitamins B1, B2, B6, B9, and B12, while sardines have more of vitamins B3, E, and K. That’s a 5:3 win for herring, although it’s worth mentioning that the margins of difference are mostly not huge, except for that sardines have 26x the vitamin K content. Still, by the overall numbers, this one’s a win for herring.
In the category of minerals, herring is not richer in any minerals*, while sardines are richer in calcium, copper, iron, manganese, phosphorus, and selenium, meaning a clear win for sardines.
*unless we want to consider mercury to be a mineral, in which case, let’s mention that on average, herring is 6x higher in mercury. However, we consider that also a win for sardines.
All in all, sardines are better for the heart (much lower in cholesterol), bones (much higher in calcium), and brain (much lower in mercury).
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: Antibiotics, Mercury, & More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Reduce Chronic Stress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sunday Stress-Buster
First, an important distinction:
- Acute stress (for example, when stepping out of your comfort zone, engaging in competition, or otherwise focusing on something that requires your full attention for best performance) is generally a good thing. It helps you do you your best. It’s sometimes been called “eustress”, “good stress”.
- Chronic stress (for example, when snowed under at work and you do not love it, when dealing with a serious illness, and/or faced with financial problems) is unequivocally a bad thing. Our body is simply not made to handle that much cortisol (the stress hormone) all the time.
Know the dangers of too much cortisol
We covered this as a main feature last month: Lower Your Cortisol! (Here’s Why & How)
…but it bears mentioning again and for those who’ve joined us since then:
A little spike of cortisol now and again can be helpful. Having it spiking all the time, or even a perpetual background low-to-moderate level, can be ruinous to the health in so many ways.
The good news is, the physiological impact of stress on the body (which ranges from face-and-stomach fat deposits, to rapid aging), can be reversed—even the biological aging!
Read: Biological age is increased by stress and restored upon recovery ← this study is so hot-of-the-press that it was published literally two days ago
Focus on what you can control
A lot of things that cause you stress may be outside of your control. Focus on what is within your control. Oftentimes, we are so preoccupied with the stress, that we employ coping strategies that don’t actually deal with the problem.
That’s a maladaptive response to an evolutionary quirk—our bodies haven’t caught up with modern life, and on an evolutionary scale, are still priming us to deal with sabre-toothed tigers, not financial disputes, for example.
But, how to deal with the body’s “wrong” response?
First, deal with the tiger. There isn’t one, but your body doesn’t know that. Do some vigorous exercise, or if that’s not your thing, tense up your muscles strongly for a few seconds and then relax them, doing each part of your body. This is called progressive relaxation, and how it works is basically tricking your body into thinking you successfully fled the tiger, or fought the tiger and won.
Next, examine what the actual problem is, that’s causing you stress. You’re probably heavily emotionally attached to the problem, or else it wouldn’t be stressing you. So, imagine what advice you would give to help a friend deal with the same problem, and then do that.
Better yet: enlist an actual friend (or partner, family member, etc) to help you. We are evolved to live in a community, engaged in mutual support. That’s how we do well; that’s how we thrive best.
By dealing with the problem—or sometimes even just having support and/or something like a plan—your stress will evaporate soon enough.
The power of “…and then what?”
Sometimes, things are entirely out of your control. Sometimes, bad things are entirely possible; perhaps even probable. Sometimes, they’re so bad, that it’s difficult to avoid stressing about the possible outcomes.
If something seems entirely out of your control and/or inevitable, ask yourself:
“…and then what?”
Writer’s storytime: when I was a teenager, sometimes I would go out without a coat, and my mother would ask, pointedly, “But what will you do if it rains?!”
I’d reply “I’ll get wet, of course”
This attitude can go just the same for much more serious outcomes, up to and including death.
So when you find yourself stressing about some possible bad outcome, ask yourself, “…and then what?”.
- What if this is cancer? Well, it might be. And then what? You might seek cancer treatment.
- What if I can’t get treatment, or it doesn’t work? Well, you might die. And then what?
In Dialectic Behavior Therapy (DBT), this is called “radical acceptance” and acknowledges bad possible/probable/known outcomes, allows one to explore the feelings, and come up with a plan for managing the situation, or even just coming to terms with the fact that sometimes, suffering is inevitable and is part of the human condition.
It’ll still be bad—but you won’t have added extra suffering in the form of stress.
Breathe.
Don’t underestimate the power of relaxed deep breathing to calm the rest of your body, including your brain.
Also: we’ve shared this before, a few months ago, but this 8 minute soundscape was developed by sound technicians working with a team of psychologists and neurologists. It’s been clinically tested, and found to have a much more relaxing effect(in objective measures of lowering heart rate and lowering cortisol levels, as well as in subjective self-reports) than merely “relaxing music”.
Try it and see for yourself:
! Share This Post
-
Understanding Cellulitis: Skin And Soft Tissue Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference between a minor passing skin complaint, and a skin condition that’s indicative of something more serious? Dr. Thomas Watchman explains:
More than skin-deep
Cellulitis sounds benign enough, like having a little cellulite perhaps, but in fact it means an infection of the skin and—critically—the underlying soft tissues.
Normally, the skin acts as a barrier against infections, but this barrier can be breached by physical trauma (i.e. an injury that broke the skin), eczema, fungal nail infections, skin ulcers, and other similar things that disrupt the skin’s ability to protect us.
Things to watch out for: Dr. Watchman advises we keep an eye out for warm, reddened skin, swelling, and blisters. Specifically, a golden-yellow crust to these likely indicates a Staphylococcus aureus infection (hence the name).
There’s a scale of degrees of severity:
- Class 1: No systemic toxicity or comorbidities
- Class 2: Systemic toxicity or comorbidities present
- Class 3: Significant systemic toxicity or comorbidities with risk of significant deterioration
- Class 4: Sepsis or life-threatening infection
…with antibiotics being recommended in the latter two cases there, or in other cases for frail, young, old, or immunocompromised patients. Given the rather “scorched earth” results of antibiotics (they cause a lot of collateral iatrogenic damage), this can be taken as a sign of how seriously such infections should be taken.
For more about all this, including visual guides, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Of Brains & Breakouts: The Brain-Skin Doctor
- Beyond Supplements: The Real Immune-Boosters!
- Antibiotics? You Might Want To Think Thrice
Take care!
Share This Post
-
Should You Go Light Or Heavy On Carbs?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Carb-Strong or Carb-Wrong?
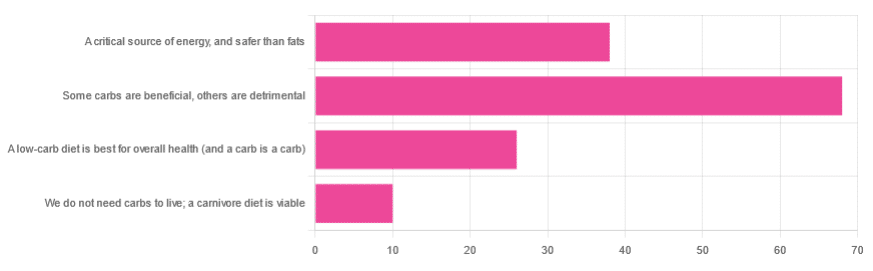
We asked you for your health-related view of carbs, and got the above-depicted, below-described, set of responses
- About 48% said “Some carbs are beneficial; others are detrimental”
- About 27% said “Carbs are a critical source of energy, and safer than fats”
- About 18% said “A low-carb diet is best for overall health (and a carb is a carb)”
- About 7% said “We do not need carbs to live; a carnivore diet is viable”
But what does the science say?
Carbs are a critical source of energy, and safer than fats: True or False?
True and False, respectively! That is: they are a critical source of energy, and carbs and fats both have an important place in our diet.
❝Diets that focus too heavily on a single macronutrient, whether extreme protein, carbohydrate, or fat intake, may adversely impact health.❞
Source: Low carb or high carb? Everything in moderation … until further notice
(the aforementioned lead author Dr. de Souza, by the way, served as an external advisor to the World Health Organization’s Nutrition Guidelines Advisory Committee)
Some carbs are beneficial; others are detrimental: True or False?
True! Glycemic index is important here. There’s a big difference between eating a raw carrot and drinking high-fructose corn syrup:
Which Sugars Are Healthier, And Which Are Just The Same?
While some say grains and/or starchy vegetables are bad, best current science recommends:
- Eat some whole grains regularly, but they should not be the main bulk of your meal (non-wheat grains are generally better)
- Starchy vegetables are not a critical food group, but in moderation they are fine.
To this end, the Mediterranean Diet is the current gold standard of healthful eating, per general scientific consensus:
A low-carb diet is best for overall health (and a carb is a carb): True or False?
True-ish and False, respectively. We covered the “a carb is a carb” falsehood earlier, so we’ll look at “a low-carb diet is best”.
Simply put: it can be. One of the biggest problems facing the low-carb diet though is that adherence tends to be poor—that is to say, people crave their carby comfort foods and eat more carbs again. As for the efficacy of a low-carb diet in the context of goals such as weight loss and glycemic control, the evidence is mixed:
❝There is probably little to no difference in weight reduction and changes in cardiovascular risk factors up to two years’ follow-up, when overweight and obese participants without and with T2DM are randomised to either low-carbohydrate or balanced-carbohydrate weight-reducing diets❞
Source: Low-carbohydrate versus balanced-carbohydrate diets for reducing weight and cardiovascular risk
❝On the basis of moderate to low certainty evidence, patients adhering to an LCD for six months may experience remission of diabetes without adverse consequences.
Limitations include continued debate around what constitutes remission of diabetes, as well as the efficacy, safety, and dietary satisfaction of longer term LCDs❞
~ Dr. Joshua Goldenberg et al.
Source: Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission
❝There should be no “one-size-fits-all” eating pattern for different patient´s profiles with diabetes.
It is clinically complex to suggest an ideal percentage of calories from carbohydrates, protein and lipids recommended for all patients with diabetes.❞
Source: Current Evidence Regarding Low-carb Diets for The Metabolic Control of Type-2 Diabetes
We do not need carbs to live; a carnivore diet is viable: True or False?
False. For a simple explanation:
The Carnivore Diet: Can You Have Too Much Meat?
There isn’t a lot of science studying the effects of consuming no plant products, largely because such a study, if anything other than observational population studies, would be unethical. Observational population studies, meanwhile, are not practical because there are so few people who try this, and those who do, do not persist after their first few hospitalizations.
Putting aside the “Carnivore Diet” as a dangerous unscientific fad, if you are inclined to meat-eating, there is some merit to the Paleo Diet, at least for short-term weight loss even if not necessarily long-term health:
What’s The Real Deal With The Paleo Diet?
For longer-term health, we refer you back up to the aforementioned Mediterranean Diet.
Enjoy!
Share This Post
Related Posts
-
You can train your nose – and 4 other surprising facts about your sense of smell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Would you give up your sense of smell to keep your hair? What about your phone?
A 2022 US study compared smell to other senses (sight and hearing) and personally prized commodities (including money, a pet or hair) to see what people valued more.
The researchers found smell was viewed as much less important than sight and hearing, and valued less than many commodities. For example, half the women surveyed said they’d choose to keep their hair over sense of smell.
Smell often goes under the radar as one of the least valued senses. But it is one of the first sensory systems vertebrates developed and is linked to your mental health, memory and more.
Here are five fascinating facts about your olfactory system.
DimaBerlin/Shutterstock 1. Smell is linked to memory and emotion
Why can the waft of fresh baking trigger joyful childhood memories? And why might a certain perfume jolt you back to a painful breakup?
Smell is directly linked to both your memory and emotions. This connection was first established by American psychologist Donald Laird in 1935 (although French novelist Marcel Proust had already made it famous in his reverie about the scent of madeleines baking.)
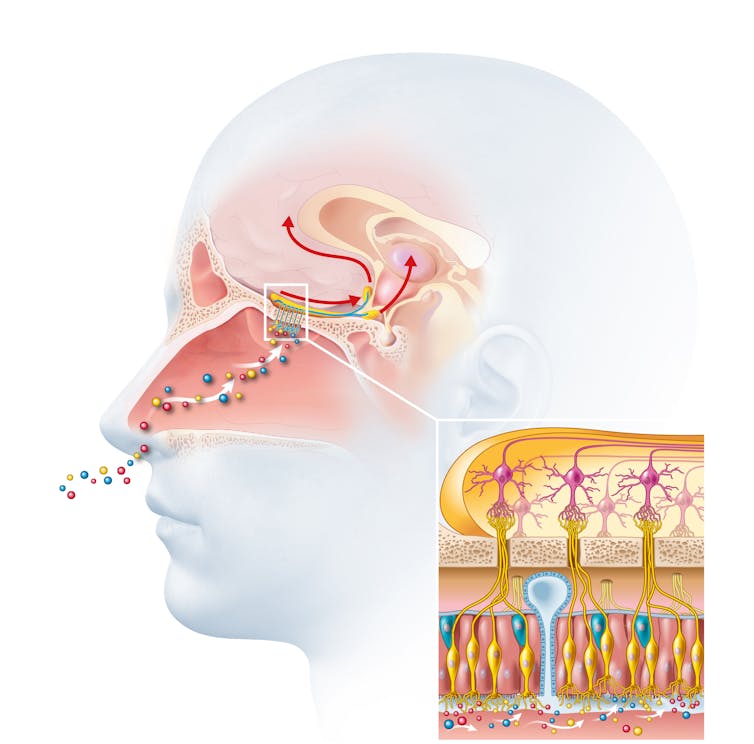
Odours are first captured by special olfactory nerve cells inside your nose. These cells extend upwards from the roof of your nose towards the smell-processing centre of your brain, called the olfactory bulb.
Smells are first detected by nerve cells in the nose. Axel_Kock/Shutterstock From the olfactory bulb they form direct connection with the brain’s limbic system. This includes the amygdala, where emotions are generated, and the hippocampus, where memories are created.
Other senses – such as sight and hearing – aren’t directly connected to the lymbic system.
One 2004 study used functional magnetic resonance imaging to demonstrate odours trigger a much stronger emotional and memory response in the brain than a visual cue.
2. Your sense of smell constantly regenerates
You can lose your ability to smell due to injury or infection – for example during and after a COVID infection. This is known as olfactory dysfunction. In most cases it’s temporary, returning to normal within a few weeks.
This is because every few months your olfactory nerve cells die and are replaced by new cells.
We’re not entirely sure how this occurs, but it likely involves your nose’s stem cells, the olfactory bulb and other cells in the olfactory nerves.
Other areas of your nervous system – including your brain and spinal cord – cannot regenerate and repair after an injury.
Constant regeneration may be a protective mechanism, as the olfactory nerves are vulnerable to damage caused by the external environment, including toxins (such as cigarette smoke), chemicals and pathogens (such as the flu virus).
But following a COVID infection some people might continue to experience a loss of smell. Studies suggest the virus and a long-term immune response damages the cells that allow the olfactory system to regenerate.
3. Smell is linked to mental health
Around 5% of the global population suffer from anosmia – total loss of smell. An estimated 15-20% suffer partial loss, known as hyposmia.
Given smell loss is often a primary and long-term symptom of COVID, these numbers are likely to be higher since the pandemic.
Yet in Australia, the prevalence of olfactory dysfunction remains surprisingly understudied.
Losing your sense of smell is shown to impact your personal and social relationships. For example, it can mean you miss out on shared eating experiences, or cause changes in sexual desire and behaviour.
In older people, declining ability to smell is associated with a higher risk of depression and even death, although we still don’t know why.
Losing your sense of smell can have a major impact on mental health. Halfpoint/Shutterstock 4. Loss of smell can help identify neurodegenerative diseases
Partial or full loss of smell is often an early indicator for a range of neurodegenerative diseases, including Alzheimer’s and Parkinson’s diseases.
Patients frequently report losing their sense of smell years before any symptoms show in body or brain function. However many people are not aware they are losing their sense of smell.
There are ways you can determine if you have smell loss and to what extent. You may be able to visit a formal smell testing centre or do a self-test at home, which assesses your ability to identify household items like coffee, wine or soap.
5. You can train your nose back into smelling
“Smell training” is emerging as a promising experimental treatment option for olfactory dysfunction. For people experiencing smell loss after COVID, it’s been show to improve the ability to detect and differentiate odours.
Smell training (or “olfactory training”) was first tested in 2009 in a German psychology study. It involves sniffing robust odours — such as floral, citrus, aromatic or fruity scents — at least twice a day for 10—20 seconds at a time, usually over a 3—6 month period.
Participants are asked to focus on the memory of the smell while sniffing and recall information about the odour and its intensity. This is believed to help reorganise the nerve connections in the brain, although the exact mechanism behind it is unclear.
Some studies recommend using a single set of scents, while others recommend switching to a new set of odours after a certain amount of time. However both methods show significant improvement in smelling.
This training has also been shown to alleviate depressive symptoms and improve cognitive decline both in older adults and those suffering from dementia.
Just like physiotherapy after a physical injury, olfactory training is thought to act like rehabilitation for your sense of smell. It retrains the nerves in your nose and the connections it forms within the brain, allowing you to correctly detect, process and interpret odours.
Lynn Nazareth, Research Scientist in Olfactory Biology, CSIRO
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Artichoke vs Asparagus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to asparagus, we picked the artichoke.
Why?
Both are great and it was close!
In terms of macros, artichoke has a little more protein and around 3x the carbs and fiber: the ratio there means that both vegetables have an identical glycemic index, so we’ll go with the “most food per food” reckoning of nutritional density, and call it for the artichoke.
When it comes to vitamins, artichoke has more of vitamins B3, B5, B6, B7, B9, C, and choline, while asparagus has more of vitamins A, B1, B2, E, and K. Both very respectable nutritional sets, but artichoke gets a marginal 6:5 win on strength of numbers.
In the category of minerals, artichoke has more calcium, copper, magnesium, manganese, phosphorus, and potassium, while asparagus has more iron, selenium, and zinc. A clearer 6:3 win for artichoke this time.
Once again, both of these are great foods, so by all means enjoy either or both. But if you’re looking for the nutritionally densest option, it’s the artichoke!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Keep Your Mind From Wandering
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether your mind keeps wandering more as you get older, or you’re a young student whose super-active brain is more suited to TikTok than your assigned reading, sustained singular focus can be a challenge for everyone—and yet (alas!) it remains a required skill for so much in life.
Today’s edition of 10Almonds presents a nifty trick to get yourself through those tasks! We’ll also be taking some time to reply to your questions and comments, in our weekly interactive Q&A.
First of all though, we’ve a promise to make good on, so…
How To Stay On The Ball (Or The Tomato?) The Easy Way
For most of us, we face three main problems when it comes to tackling our to-dos:
- Where to start?
- The task seems intimidating in its size
- We get distracted and/or run out of energy
If you’re really not sure where to start, we recommended a powerful tool in last Friday’s newsletter!
For the rest, we love the Pomodoro Technique:
- Set a timer for 25 minutes, and begin your task.
- Keep going until the timer is done! No other tasks, just focus.
- Take a 5-minute break.
- Repeat
This approach has three clear benefits:
- No matter the size of the task, you are only committing to 25 minutes—everything is much less overwhelming when there’s an end in sight!
- Being only 25 minutes means we are much more likely to stay on track; it’s easier to defer other activities if we know that there will be a 5-minute break for that soon.
- Even without other tasks to distract us, it can be difficult to sustain attention for long periods; making it only 25 minutes at a time allows us to approach it with a (relatively!) fresh mind.
Have you heard that a human brain can sustain attention for only about 40 minutes before focus starts to decline rapidly?
While that’s been a popular rationale for school classroom lesson durations (and perhaps coincidentally ties in with Zoom’s 40-minute limit for free meetings), the truth is that focus starts dropping immediately, to the point that one-minute attention tests are considered sufficient to measure the ability to focus.
So a 25-minute Pomodoro is a more than fair compromise!
Why’s it called the “Pomodoro” technique?
And why is the 25-minute timed work period called a Pomodoro?
It’s because back in the 80s, university student Francesco Cirillo was struggling to focus and made a deal with himself to focus just for a short burst at a time—and he used a (now “retro” style) kitchen timer in the shape of a tomato, or “pomodoro”, in Italian.
If you don’t have a penchant for kitsch kitchenware, you can use this free, simple Online Pomodoro Timer!
(no registration/login/download necessary; it’s all right there on the web page)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: