Coconut & Lemongrass Protein Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The main protein here is pea protein, but the soup’s health benefits don’t stop there. With healthy MCTs from the coconut, as well as phytochemical benefits from the ginger and chili, this wonderfully refreshing soup has a lot to offer.
You will need
- 1 can coconut milk
- 1 cup vegetable stock (making your own, or buying a low-sodium option)
- 1 cup frozen petits pois
- 1 oz fresh ginger, roughly chopped
- ½ oz lemongrass stalk, crumpled without being broken into multiple pieces
- 1 red chili, roughly chopped
- 1 tbsp white miso paste
- zest and juice of 1 lime
- Optional: garnish of your choice
Method
(we suggest you read everything at least once before doing anything)
1) Mix the coconut milk, vegetable stock, ginger, and chili in a saucepan, and simmer for 15 minutes
2) Remove the lemongrass and ginger (and the chili if you don’t want more heat), and add the petit pois. Bring back to a simmer for about 2 minutes more, stir in the miso paste and lime, then take off the heat.
3) Blend the soup to a smooth purée. Since it is hot, you will need to either use a stick blender, or else a food processor that is ok with blending hot liquids (many are not, so don’t use yours unless you’re sure, as it might explode if it’s not made for that). Alternatively, you can let it cool, blend it, and then reheat it.
4) Serve, adding a garnish if you so wish:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Can Saturated Fats Be Healthy?
- Ginger Does A Lot More Than You Think
- Capsaicin For Weight Loss And Against Inflammation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Natural Remedies and Foods for Osteoarthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Natural solutions for osteoarthritis. Eg. Rosehip tea, dandelion root tea. Any others??? What foods should I absolutely leave alone?❞
We’ll do a main feature on arthritis (in both its main forms) someday soon, but meanwhile, we recommend eating for good bone/joint health and against inflammation. To that end, you might like these main features we did on those topics:
- We Are Such Stuff As Fish Are Made Of (collagen for bone and joint health)
- The Bare-Bones Truth About Osteoporosis (eating for bone health generally)
- Keep Inflammation At Bay (dietary tips for minimizing inflammation—also, our all-time most popular article to date!)
Of these, probably the last one is the most critical, and also will have the speediest effects if implemented.
Share This Post
-
Kiwi Fruit vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi fruit to pineapple, we picked the kiwi.
Why?
In terms of macros, they’re mostly quite comparable, being fruits made of mostly water, and a similar carb count (slightly different proportions of sugar types, but nothing that throws out the end result, and the GI is low for both). Technically kiwi has twice the protein, but they are fruits and “twice the protein” means “0.5g difference per 100g”. Aside from that, and more meaningfully, kiwi also has twice the fiber.
When it comes to vitamins, kiwi has more of vitamins A, B9, C, E, K, and choline, while pineapple has more of vitamins B1, B2, B3, B5, and B6. This would be a marginal (6:5) win for kiwi, but kiwi’s margins of difference are greater per vitamin, including 72x more vitamin E (with a cupful giving 29% of the RDA, vs a cupful of pineapple giving 0.4% of the RDA) and 57x more vitamin K (with a cupful giving a day’s RDA, vs a cupful of pineapple giving a little under 2% of the RDA). So, this is a fair win for kiwi.
In the category of minerals, things are clear: kiwi has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pineapple has more manganese. An overwhelming win for kiwi.
Looking at their respective anti-inflammatory powers, pineapple has its special bromelain enzymes, which is a point in its favour, but when it comes to actual polyphenols, the two fruits are quite balanced, with kiwi’s flavonoids vs pineapple’s lignans.
Adding up the sections, it’s a clear win for kiwi—but pineapple is a very respectable fruit too (especially because of its bromelain content), so do enjoy both!
Want to learn more?
You might like to read:
Bromelain vs Inflammation & Much More
Take care!
Share This Post
-
Delicious Quinoa Avocado Bread
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
They’re gluten-free, full of protein and healthy fats, generous with the fiber, easy to make, and tasty too! What’s not to love? Keep this recipe (and its ingredients) handy for next time you want healthy burger buns or similar:
You will need
- 2½ cups quinoa flour
- 2 cups almond flour (if allergic, just substitute more quinoa flour)
- 1 avocado, peeled, pitted, and mashed
- zest and juice of 1 lime
- 2 tbsp ground flaxseed
- 1 tsp baking powder
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: seeds, oats, or similar for topping the buns
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉/175℃.
2) Mix the flaxseed with ⅓ cup warm water and set aside.
3) Mix, in a large bowl, the quinoa flour and almond flour with the baking powder and the MSG or salt.
4) Mix, in a separate smaller bowl, the avocado and lime.
5) Add the wet ingredients to the dry, slowly, adding an extra ½ cup water as you do, and knead into a dough.
6) Divide the dough into 4 equal portions, each shaped into a ball and then slightly flattened, to create a burger bun shape. If you’re going to add any seeds or similar as a topping, add those now.
7) Bake them in the oven (on a baking sheet lined with baking paper) for 20–25 minutes. You can check whether they’re done the same way you would a cake, by piercing them to the center with a toothpick and seeing whether it comes out clean.
8) Serve when sufficiently cooled.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Gluten: What’s The Truth?
- Why You Should Diversify Your Nuts!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post
Related Posts
-
Which Osteoporosis Medication, If Any, Is Right For You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Which Osteoporosis Medication, If Any, Is Right For You?
We’ve written about osteoporosis before, so here’s a quick recap first in case you missed these:
- The Bare-bones Truth About Osteoporosis
- Exercises To Do (And Exercises To Avoid) If You Have Osteoporosis
- We Are Such Stuff As Fish Are Made Of
- Vit D + Calcium: Too Much Of A Good Thing?
All of those look and diet and/or exercise, with “diet” including supplementation. But what of medications?
So many choices (not all of them right for everyone)
The UK’s Royal Osteoporosis Society says of the very many osteoporosis meds available:
❝In terms of effectiveness, they all reduce your risk of broken bones by roughly the same amount.
Which treatment is right for you will depend on a number of things.❞
…before then going on to list a pageful of things it will depend on, and giving no specific information about what prescriptions or proscriptions may be made based on those factors.
Source: Royal Osteoporosis Society | Which medication should I take?
We’ll try to do better than that here, though we have less space. So let’s get down to it…
First line drug offerings
After diet/supplementation and (if applicable) hormones, the first line of actual drug offerings are generally biphosphates.
Biphosphates work by slowing down your osteoclasts—the cells that break down your bones. They may sound like terrible things to have in the body at all, but remember, your body is always rebuilding itself and destruction is a necessary act to facilitate creation. However, sometimes things can get out of balance, and biphosphates help tip things back into balance.
Common biphosphates include Alendronate/Fosamax, Risedronate/Actonel, Ibandronate/Boniva, and Zolendronic acid/Reclast.
A common downside is that they aren’t absorbed well by the stomach (despite being mostly oral administration, though IV versions exist too) and can cause heartburn / general stomach upset.
An uncommon downside is that messing with the body’s ability to break down bones can cause bones to be rebuilt-in-place slightly incorrectly, which can—paradoxically—cause fractures. But that’s rare and is more common if the drugs are taken in much higher doses (as for bone cancer rather than osteoporosis).
Bone-builders
If you already have low bone density (so you’re fighting to rebuild your bones, not just slow deterioration), then you may need more of a boost.
Bone-building medications include Teriparatide/Forteo, Abaloparatide/Tymlos, and Romosozumab/Evenity.
These are usually given by injection, usually for a course of one or two years.
Once the bone has been built up, it’ll probably be recommended that you switch to a biphosphate or other bone-stabilizing medication.
Estrogen-like effects, without estrogen
If your osteoporosis (or osteoporosis risk) comes from being post-menopausal, estrogen is a very common (and effective!) prescription. However, some people may wish to avoid it, if for example you have a heightened breast cancer risk, which estrogen can exacerbate.
So, medications that have estrogen-like effects post-menopause, but without actually increasing estrogen levels, include: Raloxifene/Evista, and also all the meds we mentioned in the bone-building category above.
Raloxifene/Evista specifically mimics the action of estrogen on bones, while at the same time blocking the effect of estrogen on other tissues.
Learn more…
Want a more thorough grounding than we have room for here? You might find the following resource useful:
List of 82 Osteoporosis Medications Compared (this has a big table which is sortable by various variables)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Savory Protein Crêpe
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pancakes have a bad reputation healthwise, but they don’t have to be so. Here’s a very healthy crêpe recipe, with around 20g of protein per serving (which is about how much protein most people’s body’s can use at one sitting) and a healthy dose of fiber too:
You will need
Per crêpe:
- ½ cup milk (your preference what kind; we recommend oat milk for this)
- 2 oz chickpea flour (also called garbanzo bean flour, or gram flour)
- 1 tsp nutritional yeast
- 1 tsp ras el-hanout (optional but tasty and contains an array of beneficial phytochemicals)
- 1 tsp dried mixed herbs
- ⅛ tsp MSG or ¼ tsp low-sodium salt
For the filling (also per crêpe):
- 6 cherry tomatoes, halved
- Small handful baby spinach
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Mix the dry crêpe ingredients in a bowl, and then stir in the milk, whisking to mix thoroughly. Leave to stand for at least 5 minutes.
2) Meanwhile, heat a little olive oil in a skillet, add the tomatoes and fry for 1 minute, before adding the spinach, stirring, and turning off the heat. As soon as the spinach begins to wilt, set it aside.
3) Heat a little olive oil either in the same skillet (having been carefully wiped clean) or a crêpe pan if you have one, and pour in a little of the batter you made, tipping the pan so that it coats the pan evenly and thinly. Once the top is set, jiggle the pan to see that it’s not stuck, and then flip your crêpe to finish on the other side.
If you’re not confident of your pancake-tossing skills, or your pan isn’t good enough quality to permit this, you can slide it out onto a heatproof chopping board, and use that to carefully turn it back into the pan to finish the other side.
4) Add the filling to one half of the crêpe, and fold it over, pushing down at the edges with a spatula to make a seal, cooking for another 30 seconds or so. Alternatively, you can just serve a stack of crêpes and add the filling at the table, folding or rolling per personal preference:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Three Daily Servings of Beans?
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Sea Salt vs MSG – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How they did it: STAT reporters expose how ailing seniors suffer when Medicare Advantage plans use algorithms to deny care
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a call with a long-time source, what stood out most to STAT reporters Bob Herman and Casey Ross was just how viscerally frustrated and angry the source was about an algorithm used by insurance companies to decide how long patients should stay in a nursing home or rehab facility before being sent home.
The STAT stories had a far-reaching impact:
- The U.S. Senate Committee on Homeland Security and Government Affairs took a rare step of launching a formal investigation into the use of algorithms by the country’s three largest Medicare Advantage insurers.
- Thirty-two House members urged the Centers for Medicare and Medicaid Services to increase the oversight of algorithms that health insurers use to make coverage decisions.
- In a rare step, CMS launched its own investigation into UnitedHealth. It also stiffened its regulations on the use of proprietary algorithms and introduced plans to audit denials across Medicare Advantage plans in 2024.
- Based on STAT’s reporting, Medicare Advantage beneficiaries filed two class-action lawsuits against UnitedHealth and its NaviHealth subsidiary, the maker of the algorithm, and against Humana, another major health insurance company that was also using the algorithm.
- Amid scrutiny, UnitedHealth renamed NaviHealth.
The companies never allowed an on-the-record interview with their executives, but they acknowledged that STAT’s reporting was true, according to the news organization.
Ross and Herman spoke with The Journalist’s Resource about their project and shared the following eight tips.
1. Search public comments on proposed federal rules to find sources.
Herman and Ross knew that the Centers for Medicare and Medicaid Services had put out a request for public comments, asking stakeholders within the Medicare Advantage industry how the system could improve.
There are two main ways to get Medicare coverage: original Medicare, which is a fee-for-service health plan, and Medicare Advantage, which is a type of Medicare health plan offered by private insurance companies that contract with Medicare. Medicare Advantage plans have increasingly become popular in recent years.
Under the Social Security Act, the public has the opportunity to submit comments on Medicare’s proposed national coverage determinations. CMS uses public comments to inform its proposed and final decisions. It responds in detail to all public comments when issuing a final decision.
The reporters began combing through hundreds of public comments attached to a proposed Medicare Advantage rule that was undergoing federal review. NaviHealth, the UnitedHealth subsidiary and the maker of the algorithm, came up in many of the comments, which include the submitters’ information.
“These are screaming all-caps comments to federal regulators about YOU NEED TO SOMETHING ABOUT THIS BECAUSE IT’S DISGUSTING,” Ross says.
“The federal government is proposing rules and regulations all the time,” adds Herman, STAT’s business of health care reporter. “If someone’s going to take the time and effort to comment on them, they must have at least some knowledge of what’s going on. It’s just a great tool for any journalist to use to figure out more and who to contact.”
The reporters also found several attorneys who had complained in the comments. They began reaching out to them, eventually gaining access to confidential documents and intermediaries who put them in touch with patients to show the human impact of the algorithm.
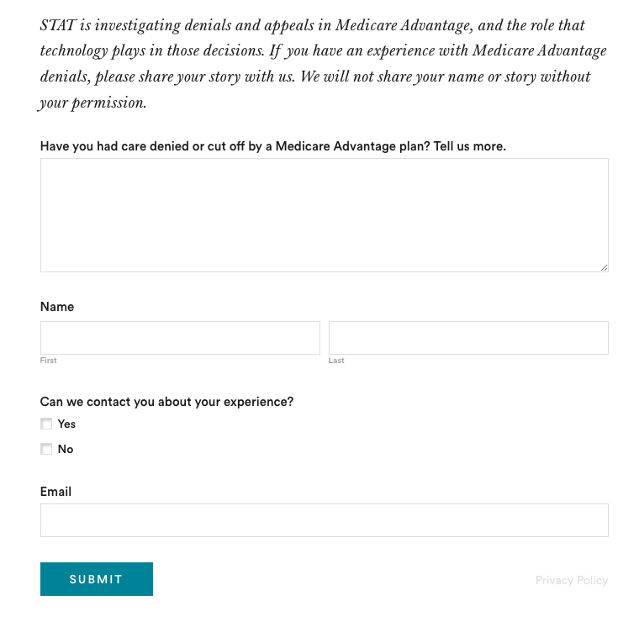
2. Harness the power of the reader submission box.
At the suggestion of an editor, the reporters added a reader submission box at the bottom of their first story, asking them to share their own experiences with Medicare Advantage denials.
The floodgates opened. Hundreds of submissions arrived.
By the end of their first story, Herman and Ross had confidential records and some patients, but they had no internal sources in the companies they were investigating, including Navihealth. The submission box led them to their first internal source.
(Screenshot of STAT’s submission box.) The journalists also combed through LinkedIn and reached out to former and current employees, but the response rate was much lower than what they received via the submission box.
The submission box “is just right there,” Herman says. “People who would want to reach out to us can do it right then and there after they read the story and it’s fresh in their minds.”
3. Mine podcasts relevant to your story.
The reporters weren’t sure if they could get interviews with some of the key figures in the story, including Tom Scully, the former head of the Centers for Medicare and Medicaid Services who drew up the initial plans for NaviHealth years before UnitedHealth acquired it.
But Herman and another colleague had written previously about Scully’s private equity firm and they had found a podcast where he talked about his work. So Herman went back to the podcast — where he discovered Scully had also discussed NaviHealth.
The reporters also used the podcast to get Scully on the phone for an interview.
“So we knew we had a good jumping off point there to be like, ‘OK, you’ve talked about NaviHealth on a podcast, let’s talk about this,’” Herman says. “I think that helped make him more willing to speak with us.”
4. When covering AI initiatives, proceed with caution.
“A source of mine once said to me, ‘AI is not magic,’” Ross says. “People need to just ask questions about it because AI has this aura about it that it’s objective, that it’s accurate, that it’s unquestionable, that it never fails. And that is not true.”
AI is not a neutral, objective machine, Ross says. “It’s based on data that’s fed into it and people need to ask questions about that data.”
He suggests several questions to ask about the data behind AI tools:
- Where does the data come from?
- Who does it represent?
- How is this tool being applied?
- Do the people to whom the tool is being applied match the data on which it was trained? “If racial groups or genders or age of economic situations are not adequately represented in the training set, then there can be an awful lot of bias in the output of the tool and how it’s applied,” Ross says.
- How is the tool applied within the institution? Are people being forced to forsake their judgment and their own ability to do their jobs to follow the algorithm?
5. Localize the story.
More than half of all Medicare beneficiaries have Medicare Advantage and there’s a high likelihood that there are multiple Medicare Advantage plans in every county across the nation.
“So it’s worth looking to see how Medicare Advantage plans are growing in your area,” Herman says.
Finding out about AI use will most likely rely on shoe-leather reporting of speaking with providers, nursing homes and rehab facilities, attorneys and patients in your community, he says. Another source is home health agencies, which may be caring for patients who were kicked out of nursing homes and rehab facilities too soon because of a decision by an algorithm.
The anecdote that opens their first story involves a small regional health insurer in Wisconsin, which was using NaviHealth and a contractor to manage post-acute care services, Ross says.
“It’s happening to people in small communities who have no idea that this insurer they’ve signed up with is using this tool made by this other company that operates nationally,” Ross says.
There are also plenty of other companies like NaviHealth that are being used by Medicare Advantage plans, Herman says. “So it’s understanding which Medicare Advantage plans are being sold in your area and then which post-acute management companies they’re using,” he adds.
Some regional insurers have online documents that show which contractors they use to evaluate post-acute care services.
6. Get familiar with Medicare’s appeals databases
Medicare beneficiaries can contest Medicare Advantage denials through a five-stage process, which can last months to years. The appeals can be filed via the Office of Medicare Hearings and Appeals.
“Between 2020 and 2022, the number of appeals filed to contest Medicare Advantage denials shot up 58%, with nearly 150,000 requests to review a denial filed in 2022, according to a federal database,” Ross and Herman write in their first story. “Federal records show most denials for skilled nursing care are eventually overturned, either by the plan itself or an independent body that adjudicates Medicare appeals.”
There are several sources to find appeals data. Be mindful that the cases themselves are not public to protect patient privacy, but you can find the number of appeals filed and the rationale for decisions.
CMS has two quality improvement organizations, or QIOs, Livanta and Kepro, which are required to file free, publicly-available annual reports, about the cases they handle, Ross says.
Another company, Maximus, a Quality Improvement Contractor, also files reports on prior authorization cases it adjudicates for Medicare. The free annual reports include data on raw numbers of cases and basic information about the percentage denials either overturned or upheld on appeal, Ross explains.
CMS also maintains its own database on appeals for Medicare Part C (Medicare Advantage plans) and Part D, which covers prescription drugs, although the data is not complete, Ross explains.
7. Give your editor regular updates.
“Sprinkle the breadcrumbs in front of your editors,” Ross says.
“If you wrap your editors in the process, you’re more likely to be able to get to the end of [the story] before they say, ‘That’s it! Give me your copy,’” Ross says.
8. Get that first story out.
“You don’t have to know everything before you write that first story,” Ross says. “Because with that first story, if it has credibility and it resonates with people, sources will come forward and sources will continue to come forward.”
Read the stories
Denied by AI: How Medicare Advantage plans use algorithms to cut off care for seniors in need
UnitedHealth pushed employees to follow an algorithm to cut off Medicare patients’ rehab care
UnitedHealth used secret rules to restrict rehab care for seriously ill Medicare Advantage patients
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: