California Becomes Latest State To Try Capping Health Care Spending
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
California’s Office of Health Care Affordability faces a herculean task in its plan to slow runaway health care spending.
The goal of the agency, established in 2022, is to make care more affordable and accessible while improving health outcomes, especially for the most disadvantaged state residents. That will require a sustained wrestling match with a sprawling, often dysfunctional health system and powerful industry players who have lots of experience fighting one another and the state.
Can the new agency get insurers, hospitals, and medical groups to collaborate on containing costs even as they jockey for position in the state’s $405 billion health care economy? Can the system be transformed so that financial rewards are tied more to providing quality care than to charging, often exorbitantly, for a seemingly limitless number of services and procedures?
The jury is out, and it could be for many years.
California is the ninth state — after Connecticut, Delaware, Massachusetts, Nevada, New Jersey, Oregon, Rhode Island, and Washington — to set annual health spending targets.
Massachusetts, which started annual spending targets in 2013, was the first state to do so. It’s the only one old enough to have a substantial pre-pandemic track record, and its results are mixed: The annual health spending increases were below the target in three of the first five years and dropped beneath the national average. But more recently, health spending has greatly increased.
In 2022, growth in health care expenditures exceeded Massachusetts’ target by a wide margin. The Health Policy Commission, the state agency established to oversee the spending control efforts, warned that “there are many alarming trends which, if unaddressed, will result in a health care system that is unaffordable.”
Neighboring Rhode Island, despite a preexisting policy of limiting hospital price increases, exceeded its overall health care spending growth target in 2019, the year it took effect. In 2020 and 2021, spending was largely skewed by the pandemic. In 2022, the spending increase came in at half the state’s target rate. Connecticut and Delaware, by contrast, both overshot their 2022 targets.
It’s all a work in progress, and California’s agency will, to some extent, be playing it by ear in the face of state policies and demographic realities that require more spending on health care.
And it will inevitably face pushback from the industry as it confronts unreasonably high prices, unnecessary medical treatments, overuse of high-cost care, administrative waste, and the inflationary concentration of a growing number of hospitals in a small number of hands.
“If you’re telling an industry we need to slow down spending growth, you’re telling them we need to slow down your revenue growth,” says Michael Bailit, president of Bailit Health, a Massachusetts-based consulting group, who has consulted for various states, including California. “And maybe that’s going to be heard as ‘we have to restrain your margins.’ These are very difficult conversations.”
Some of California’s most significant health care sectors have voiced disagreement with the fledgling affordability agency, even as they avoid overtly opposing its goals.
In April, when the affordability office was considering an annual per capita spending growth target of 3%, the California Hospital Association sent it a letter saying hospitals “stand ready to work with” the agency. But the proposed number was far too low, the association argued, because it failed to account for California’s aging population, new investments in Medi-Cal, and other cost pressures.
The hospital group suggested a spending increase target averaging 5.3% over five years, 2025-29. That’s slightly higher than the 5.2% average annual increase in per capita health spending over the five years from 2015 to 2020.
Five days after the hospital association sent its letter, the affordability board approved a slightly less aggressive target that starts at 3.5% in 2025 and drops to 3% by 2029. Carmela Coyle, the association’s chief executive, said in a statement that the board’s decision still failed to account for an aging population, the growing need for mental health and addiction treatment, and a labor shortage.
The California Medical Association, which represents the state’s doctors, expressed similar concerns. The new phased-in target, it said, was “less unreasonable” than the original plan, but the group would “continue to advocate against an artificially low spending target that will have real-life negative impacts on patient access and quality of care.”
But let’s give the state some credit here. The mission on which it is embarking is very ambitious, and it’s hard to argue with the motivation behind it: to interject some financial reason and provide relief for millions of Californians who forgo needed medical care or nix other important household expenses to afford it.
Sushmita Morris, a 38-year-old Pasadena resident, was shocked by a bill she received for an outpatient procedure last July at the University of Southern California’s Keck Hospital, following a miscarriage. The procedure lasted all of 30 minutes, Morris says, and when she received a bill from the doctor for slightly over $700, she paid it. But then a bill from the hospital arrived, totaling nearly $9,000, and her share was over $4,600.
Morris called the Keck billing office multiple times asking for an itemization of the charges but got nowhere. “I got a robotic answer, ‘You have a high-deductible plan,’” she says. “But I should still receive a bill within reason for what was done.” She has refused to pay that bill and expects to hear soon from a collection agency.
The road to more affordable health care will be long and chock-full of big challenges and unforeseen events that could alter the landscape and require considerable flexibility.
Some flexibility is built in. For one thing, the state cap on spending increases may not apply to health care institutions, industry segments, or geographic regions that can show their circumstances justify higher spending — for example, older, sicker patients or sharp increases in the cost of labor.
For those that exceed the limit without such justification, the first step will be a performance improvement plan. If that doesn’t work, at some point — yet to be determined — the affordability office can levy financial penalties up to the full amount by which an organization exceeds the target. But that is unlikely to happen until at least 2030, given the time lag of data collection, followed by conversations with those who exceed the target, and potential improvement plans.
In California, officials, consumer advocates, and health care experts say engagement among all the players, informed by robust and institution-specific data on cost trends, will yield greater transparency and, ultimately, accountability.
Richard Kronick, a public health professor at the University of California-San Diego and a member of the affordability board, notes there is scant public data about cost trends at specific health care institutions. However, “we will know that in the future,” he says, “and I think that knowing it and having that information in the public will put some pressure on those organizations.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A person in Texas caught bird flu after mixing with dairy cattle. Should we be worried?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States’ Centers for Disease Control and Prevention (CDC) has issued a health alert after the first case of H5N1 avian influenza, or bird flu, seemingly spread from a cow to a human.
A farm worker in Texas contracted the virus amid an outbreak in dairy cattle. This is the second human case in the US; a poultry worker tested positive in Colorado in 2022.
The virus strain identified in the Texan farm worker is not readily transmissible between humans and therefore not a pandemic threat. But it’s a significant development nonetheless.
Some background on bird flu
There are two types of avian influenza: highly pathogenic or low pathogenic, based on the level of disease the strain causes in birds. H5N1 is a highly pathogenic avian influenza.
H5N1 first emerged in 1997 in Hong Kong and then China in 2003, spreading through wild bird migration and poultry trading. It has caused periodic epidemics in poultry farms, with occasional human cases.
Influenza A viruses such as H5N1 are further divided into variants, called clades. The unique variant causing the current epidemic is H5N1 clade 2.3.4.4b, which emerged in late 2020 and is now widespread globally, especially in the Americas.
In the past, outbreaks could be controlled by culling of infected birds, and H5N1 would die down for a while. But this has become increasingly difficult due to escalating outbreaks since 2021.
Wild animals are now in the mix
Waterfowl (ducks, swans and geese) are the main global spreaders of avian flu, as they migrate across the world via specific routes that bypass Australia. The main hub for waterfowl to migrate around the world is Quinghai lake in China.
But there’s been an increasing number of infected non-waterfowl birds, such as true thrushes and raptors, which use different flyways. Worryingly, the infection has spread to Antarctica too, which means Australia is now at risk from different bird species which fly here.
H5N1 has escalated in an unprecedented fashion since 2021, and an increasing number of mammals including sea lions, goats, red foxes, coyotes, even domestic dogs and cats have become infected around the world.
Wild animals like red foxes which live in peri-urban areas are a possible new route of spread to farms, domestic pets and humans.
Dairy cows and goats have now become infected with H5N1 in at least 17 farms across seven US states.
What are the symptoms?
Globally, there have been 14 cases of H5N1 clade 2.3.4.4b virus in humans, and 889 H5N1 human cases overall since 2003.
Previous human cases have presented with a severe respiratory illness, but H5N1 2.3.4.4b is causing illness affecting other organs too, like the brain, eyes and liver.
For example, more recent cases have developed neurological complications including seizures, organ failure and stroke. It’s been estimated that around half of people infected with H5N1 will die.
The case in the Texan farm worker appears to be mild. This person presented with conjunctivitis, which is unusual.
Food safety
Contact with sick poultry is a key risk factor for human infection. Likewise, the farm worker in Texas was likely in close contact with the infected cattle.
The CDC advises pasteurised milk and well cooked eggs are safe. However, handling of infected meat or eggs in the process of cooking, or drinking unpasteurised milk, may pose a risk.
Although there’s no H5N1 in Australian poultry or cattle, hygienic food practices are always a good idea, as raw milk or poorly cooked meat, eggs or poultry can be contaminated with microbes such as salmonella and E Coli.
If it’s not a pandemic, why are we worried?
Scientists have feared avian influenza may cause a pandemic since about 2005. Avian flu viruses don’t easily spread in humans. But if an avian virus mutates to spread in humans, it can cause a pandemic.
One concern is if birds were to infect an animal like a pig, this acts as a genetic mixing vessel. In areas where humans and livestock exist in close proximity, for example farms, markets or even in homes with backyard poultry, the probability of bird and human flu strains mixing and mutating to cause a new pandemic strain is higher.
There are a number of potential pathways to a pandemic caused by influenza. Author provided The cows infected in Texas were tested because farmers noticed they were producing less milk. If beef cattle are similarly affected, it may not be as easily identified, and the economic loss to farmers may be a disincentive to test or report infections.
How can we prevent a pandemic?
For now there is no spread of H5N1 between humans, so there’s no immediate risk of a pandemic.
However, we now have unprecedented and persistent infection with H5N1 clade 2.3.4.4b in farms, wild animals and a wider range of wild birds than ever before, creating more chances for H5N1 to mutate and cause a pandemic.
Unlike the previous epidemiology of avian flu, where hot spots were in Asia, the new hot spots (and likely sites of emergence of a pandemic) are in the Americas, Europe or in Africa.
Pandemics grow exponentially, so early warnings for animal and human outbreaks are crucial. We can monitor infections using surveillance tools such as our EPIWATCH platform.
The earlier epidemics can be detected, the better the chance of stamping them out and rapidly developing vaccines.
Although there is a vaccine for birds, it has been largely avoided until recently because it’s only partially effective and can mask outbreaks. But it’s no longer feasible to control an outbreak by culling infected birds, so some countries like France began vaccinating poultry in 2023.
For humans, seasonal flu vaccines may provide a small amount of cross-protection, but for the best protection, vaccines need to be matched exactly to the pandemic strain, and this takes time. The 2009 flu pandemic started in May in Australia, but the vaccines were available in September, after the pandemic peak.
To reduce the risk of a pandemic, we must identify how H5N1 is spreading to so many mammalian species, what new wild bird pathways pose a risk, and monitor for early signs of outbreaks and illness in animals, birds and humans. Economic compensation for farmers is also crucial to ensure we detect all outbreaks and avoid compromising the food supply.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney; Ashley Quigley, Senior Research Associate, Global Biosecurity, UNSW Sydney; Haley Stone, PhD Candidate, Biosecurity Program, Kirby Institute, UNSW Sydney; Matthew Scotch, Associate Dean of Research and Professor of Biomedical Informatics, College of Health Solutions, Arizona State University, and Rebecca Dawson, Research Associate, The Kirby Institute, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
5 Ways To Avoid Hearing Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hear Ye, Hear Ye
Hearing loss is often associated with getting older—but it can strike at any age. In the US, for example…
- Around 13% of adults have hearing difficulties
- Nearly 27% of those over 65 have hearing difficulties
Complete or near-complete hearing loss is less common. From the same source…
- A little under 2% of adults in general had a total or near-total inability to hear
- A little over 4% of those over 65 had a total or near-total inability to hear
Source: CDC | Hearing Difficulties Among Adults: United States, 2019
So, what to do if we want to keep our hearing as it is?
Avoid loud environments
An obvious one, but it bears stating for the sake of being methodical. Loud environments damage our ears, but how loud is too loud?
You can check how loud an environment is by using a free smartphone app, such as:
Decibel Pro: dB Sound Level Meter (iOS / Android)
An 82 dB environment is considered safe for 16 hours. That’s the equivalent of, for example moderate traffic.
Every 3 dB added to that halves the safe exposure time, for example:
- An 85 dB environment is considered safe for 8 hours. That’s the equivalent of heavier traffic, or a vacuum cleaner.
- A 94 dB environment is considered safe for 1 hour. That might be a chainsaw, a motorcycle, or a large sporting event.
Many nightclubs or concert venues often have environments of 110 dB and more. So the safe exposure time would be under two minutes.
Source: NIOSH | Noise and Hearing Loss
With differences like that per 3 dB increase, then you may want to wear hearing protection if you’re going to be in a noisy environment.
Discreet options include things like these -20 dB silicone ear plugs that live in a little case on one’s keyring.
Stop sticking things in your ears
It’s said “nothing smaller than your elbow should go in your ear canal”. We’ve written about this before:
What’s Good (And What’s Not) Against Earwax
Look after the rest of your health
Our ears are not islands unaffected by the rest of our health, and indeed, they’re larger and more complex organs than we think about most of the time, since we only tend to think about the (least important!) external part.
Common causes of hearing loss that aren’t the percussive injuries we discussed above include:
- Diabetes
- High blood pressure
- Smoking
- Infections
- Medications
Lest that last one sound a little vague, it’s because there are hundreds of medications that have hearing loss as a potential side-effect. Here’s a list so you can check if you’re taking any of them:
List of Ototoxic Medications That May Cause Tinnitus or Hearing Loss
Get your hearing tested regularly.
There are online tests, but we recommend an in-person test at a local clinic, as it won’t be subject to the limitations and quirks of the device(s) you’re using. Pretty much anywhere that sells hearing aids will probably offer you a free test, so take advantage of it!
And, more generally, if you suddenly notice you lost some or all of your hearing in one or more ears, then get thee to a doctor, and quickly.
Treat it as an emergency, because there are many things that can be treated if and only if they are caught early, before the damage becomes permanent.
Use it or lose it
This one’s important. As we get older, it’s easy to become more reclusive, but the whole “neurons that fire together, wire together” neuroplasticity thing goes for our hearing too.
Our brain is, effectively, our innermost hearing organ, insofar as it processes the information it receives about sounds that were heard.
There are neurological hearing problems that can show up without external physical hearing damage (auditory processing disorders being high on the list), but usually these things are comorbid with each other.
So if we want to maintain our ability to process the sounds our ears detect, then we need to practice that ability.
Important implication:
That means that if you might benefit from a hearing aid, you should get it now, not later.
It’s counterintuitive, we know, but because of the neurological consequences, hearing aids help people retain their hearing, whereas soldiering on without can hasten hearing loss.
On the topic of hearing difficulty comorbidities…
Tinnitus (ringing in the ears) is, paradoxically, associated with both hearing loss, and with hyperacusis (hearing supersensitivity, which sounds like a superpower, but can be quite a problem too).
Learn more about managing that, here:
Tinnitus: Quieting The Unwanted Orchestra In Your Ears
Take care!
Share This Post
-
Hair Growth: Caffeine and Minoxidil Strategies
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Hair growth strategies for men combing caffeine and minoxidil?
Well, the strategy for that is to use caffeine and minoxidil! Some more specific tips, though:
- Both of those things need to be massaged (gently!) into your scalp especially around your hairline.
- In the case of caffeine, that boosts hair growth. No extra thought or care needed for that one.
- In the case of minoxidil, it reboots the hair growth cycle, so if you’ve only recently started, don’t be surprised (or worried) if you see more shedding in the first three months. It’s jettisoning your old hairs because new ones were just prompted (by the minoxidil) to start growing behind them. So: it will get briefly worse before it gets better, but then it’ll stay better… provided you keep using it.
- If you’d like other options besides minoxidil, finasteride is a commonly prescribed oral drug that blocks the conversion of testosterone to DHT, which latter is what tells your hairline to recede.
- If you’d like other options besides prescription drugs, saw palmetto performs comparably to finasteride (and works the same way).
- You may also want to consider biotin supplementation if you don’t already enjoy that
- Consider also using a dermaroller on your scalp. If you’re unfamiliar, this is a device that looks like a tiny lawn aerator, with many tiny needles, and you roll it gently across your skin.
- It can be used for promoting hair growth, as well as for reducing wrinkles and (more slowly) healing scars.
- It works by breaking up the sebum that may be blocking new hair growth, and also makes the skin healthier by stimulating production of collagen and elastin (in response to the thousands of microscopic wounds that the needles make).
- Sounds drastic, but it doesn’t hurt and doesn’t leave any visible marks—the needles are that tiny. Still, practise good sterilization and ensure your skin is clean when using it.
See: How To Use A Dermaroller ← also explains more of the science of it
PS: this question was asked in the context of men, but the information goes the same for women suffering from androgenic alepoceia—which is a lot more common than most people think!
Share This Post
- Both of those things need to be massaged (gently!) into your scalp especially around your hairline.
Related Posts
-
Why We’re Called “10almonds”, And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Avid coffee drinker so very interested in the results Also question Is there something that you could take or eat that would prevent the caffeine from stimulating the kidneys? I tried to drink decaf from morning to night not a good result! Thanks❞
That is a good question! The simple answer is “no” (but keep reading, because all is not lost)
There’s no way (that we yet know of) to proof the kidneys against the stimulating effect of caffeine. This is especially relevant because part of caffeine’s stimulating effect is noradrenergic, and that “ren” in the middle there? It’s about the kidneys. This is just because the adrenal gland is situated next to them (actually, it’s pretty much sitting on top of them), hence the name, but it does mean that the kidneys are about the hardest thing in the body to have not affected by caffeine.
However! The effects of caffeine in general can be softened a little with l-theanine (found in tea, or it can be taken as a supplement). It doesn’t stop it from working, but it makes the curve of the effect a little gentler, and so it can reduce some unwanted side effects.
You can read more about l-theanine here:
❝How to jump start a inactive metabolism and keep it going? THANKYOU❞
The good news is, if you’re alive, your metabolism is active (it never stops!). So, it may just need perking up a little.
As for keeping it going, well, that’s what we’re here for! We’re all in favor of healthy longevity.
We’ll do a main feature soon on what we can do to influence our metabolism in either direction, but to give some quick notes here:
- A lot of our metabolism is influenced by genes and is unalterable (without modifying our genes, anyway)
- Metabolism isn’t just one thing—it’s many. And sometimes, parts of our metabolism can be much quicker or slower than others.
- When people talk about wanting a “faster metabolism”, they’re usually referring to fat-burning, and that’s just a small part of the picture, but we understand that it’s a focal point for many.
There really is enough material for a whole main feature on metabolic tweaks, though, so watch this space!
❝Why the name “10 Almonds?” Is this recommended by the Doctor? A daily dosage? And, if so, why? Thanks! Please answer me…I truly want to know!❞
Almonds are very nutritionally dense, and for example 20g of almonds (so, about 20 almonds) would give a 100% daily dose of zinc, amongst other nutrients.
We also do like to think that we give our readers an easily digestible dose of condensed “nutrition” in the form of health information.
However! That’s not actually the reason at all. It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was circulating online! So, calling ourselves 10almonds was a bit of a nod to that story, but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
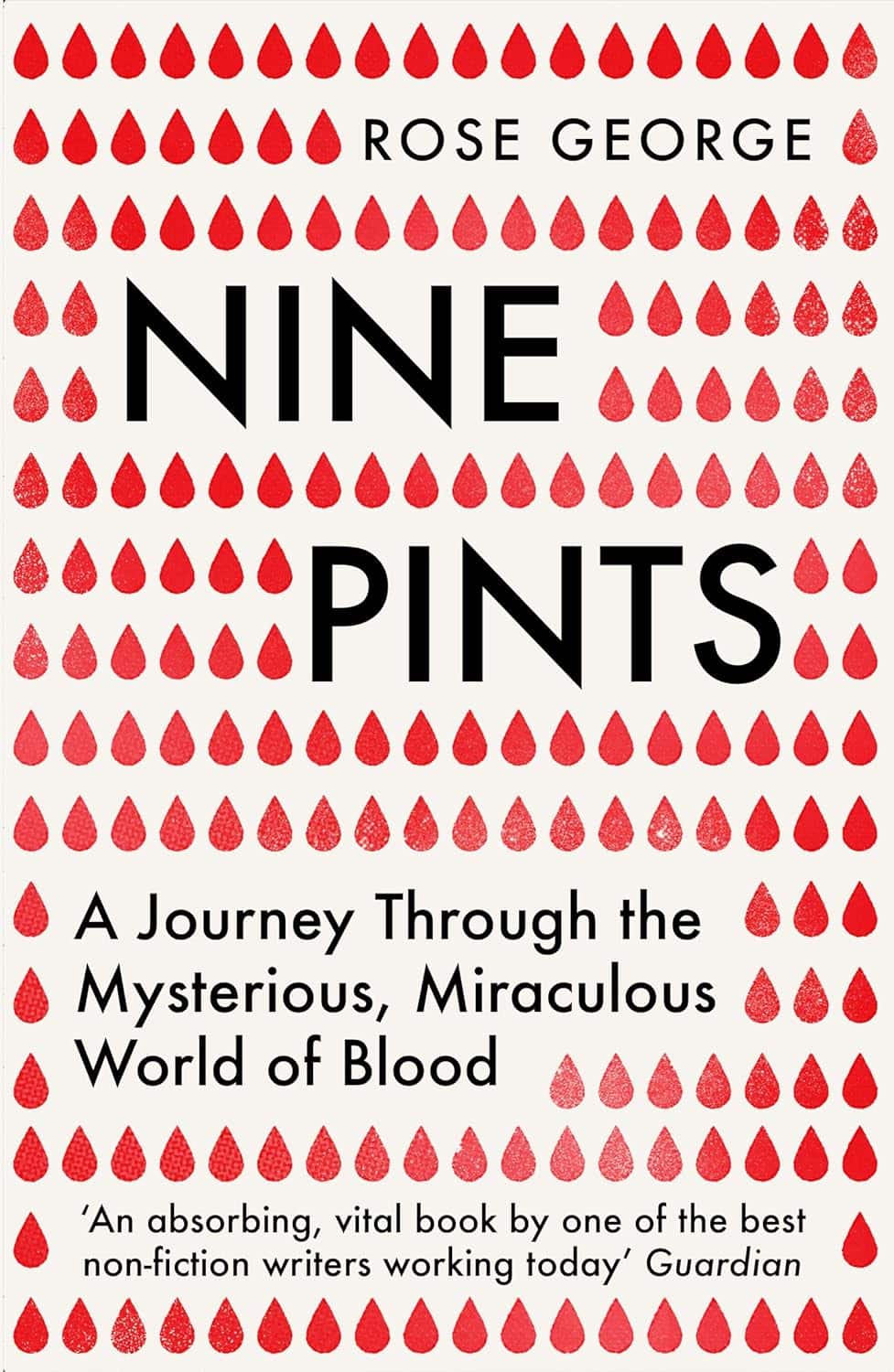
Nine Pints – by Rose George
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rose George is not a scientist, but an investigative journalist. As such, she’s a leave-no-stone-unturned researcher, and that shows here.
The style throughout is, as one might expect, journalistic. But, she’s unafraid of diving into the science of it, interviewing many medical professionals as part of her work. She also looks to people living with various blood-related conditions, ranging from hemophilia to HIV.
Speakling of highly-stigmatized yet very manageable conditions, there’s also a fair section devoted to menstruation, menstrual blood, and societies’ responses to such, from shunning to active support.
We also learn about the industrialization of blood—from blood banks to plasma labs to leech farms. You probably knew leeches are still used as a medical tool in even the most high-tech of hospitals, but you’ll doubtlessly learn a fascinating thing or two from the “insider views” along the way.
Bottom line: if you’d like to know more about the red stuff in all its marvelous aspects, with neither sensationalization nor sanitization (the topic needs neither!), this is the book for you.
Click here to check out Nine Pints, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
52 Ways to Walk – by Annabel Streets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us learned to walk at a very young age and probably haven’t thought much about it since, except perhaps in a case where some injury made it difficult.
Annabel Streets provides a wonderful guide to not just taking up (or perhaps reclaiming) the joy of walking, but also the science of it in more aspects than most of us have considered:
- The physical mechanics of walking—what’s best?
- Boots or shoes? Barefoot?
- Roads, grass, rougher vegetation… Mud?
- Flora & fauna down to the microbiota that affect us
- How much walking is needed, to be healthy?
- Is there such a thing as too much walking?
- What are the health benefits (or risks) of various kinds of weather?
- Is it better to walk quickly or to walk far?
- What about if we’re carrying some injury?
- What’s going on physiologically when we walk?
- And so much more…
Streets writes with a captivating blend of poetic joie-de-vivre coupled with scientific references.
One moment the book is talking about neuroradiology reports of NO-levels in our blood, the impact of Mycobacterium vaccae, and the studied relationship between daily steps taken and production of oligosaccharide 3′-sialyllactose, and the next it’s all:
“As if the newfound lightness in our limbs has crept into our minds, loosening our everyday cares and constraints…”
And all in all, this book helps remind us that sometimes, science and a sense of wonder can and do (and should!) walk hand-in-hand.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: