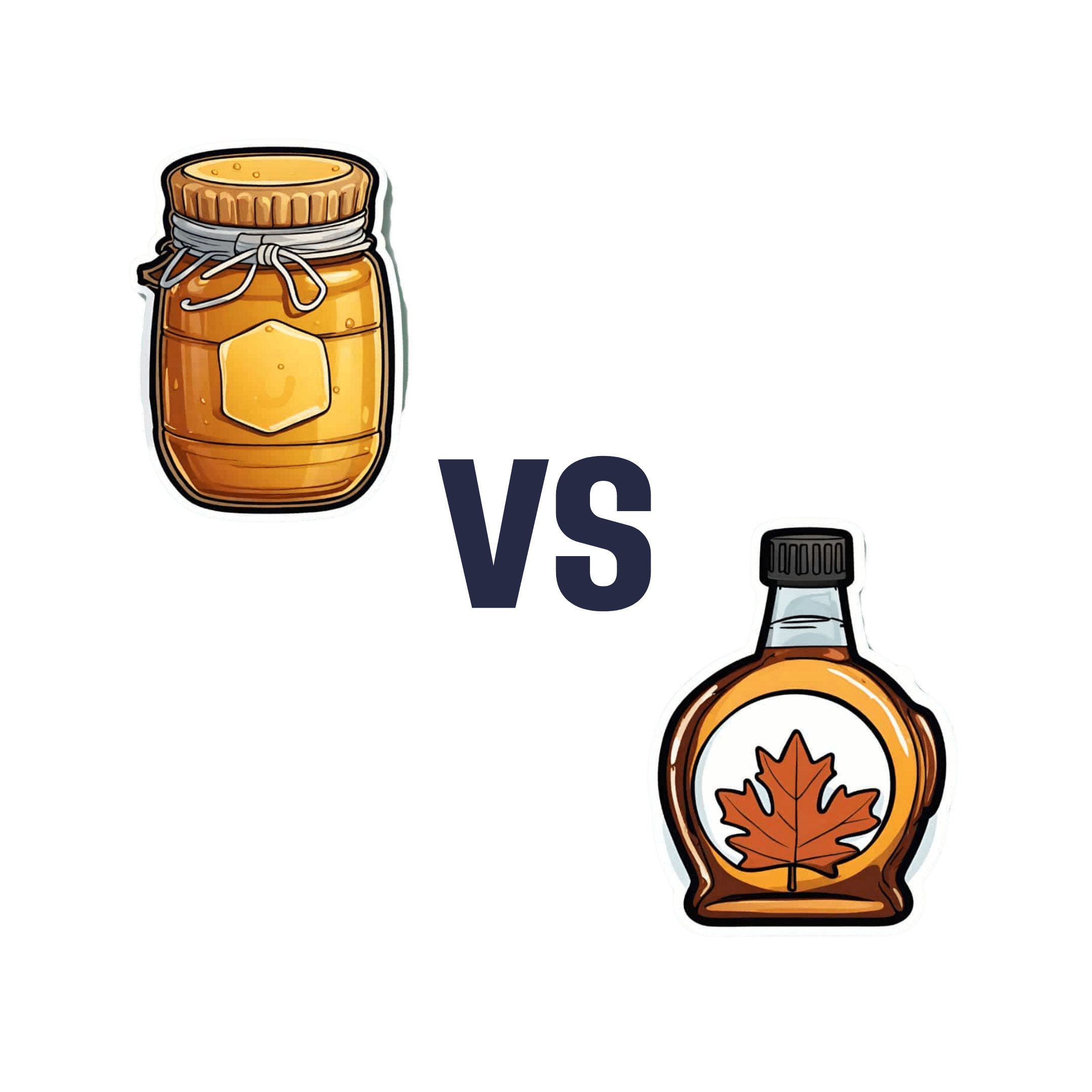
Honey vs Maple Syrup – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing honey to maple syrup, we picked the honey.
Why?
It was very close, as both have small advantages:
• Honey has some medicinal properties (and depending on type, may contain an antihistamine)
• Maple syrup is a good source of manganese, as well as low-but-present amounts of other minerals
However, you wouldn’t want to eat enough maple syrup to rely on it as a source of those minerals, and honey has the lower GI (average 46 vs 54; for comparison, refined sugar is 65), which works well as a tie-breaker.
(If GI’s very important to you, though, the easy winner here would be agave syrup if we let it compete, with its GI of 15)
Read more:
• Can Honey Relieve Allergies?
• From Apples to Bees, and High-Fructose C’s
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Psyllium Is Healthy Through-And-Through
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Psyllium is the powder of the husk of the seed of the plant Plantago ovata.
It can be taken as a supplement, and/or used in cooking.
What’s special about it?
It is fibrous, and the fiber is largely soluble fiber. It’s a “bulk-forming laxative”, which means that (dosed correctly) it is good against both constipation (because it’s a laxative) and diarrhea (because it’s bulk-forming).
See also, because this is Research Review Monday and we provide papers for everything:
In other words, it will tend things towards being a 3 or 4 on the Bristol Stool Scale ← this is not pretty, but it is informative.
Before the bowels
Because of how it increases the viscosity of substances it finds itself in, psyllium slows stomach-emptying, and thus improves feelings of satiety.
Here’s a study in which taking psyllium before breakfast and lunch resulted in increased satiety between meals, and reduction in food-related cravings:
Satiety effects of psyllium in healthy volunteers
Prebiotic benefits
We can’t digest psyllium, but our gut bacteria can—somewhat! Because they can only digest some of the psyllium fibers, that means the rest will have the stool-softening effect, while we also get the usual in-gut benefits from prebiotic fiber first too:
The Effect of Psyllium Husk on Intestinal Microbiota in Constipated Patients and Healthy Controls
Cholesterol-binding
Psyllium can bind to cholesterol during the digestive process. Why only “can”? Well, if you don’t consume cholesterol (for example, if you are vegan), then there won’t be cholesterol in the digestive tract to bind to (yes, we do need some cholesterol to live, but like most animals, we can synthesize it ourselves).
What this cholesterol-binding action means is that the dietary cholesterol thus bound cannot enter the bloodstream, and is simply excreted instead:
Heart health beyond cholesterol
Psyllium supplementation can also help lower high blood pressure but does not significantly lower already-healthy blood pressure, so it can be particularly good for keeping things in safe ranges:
❝Given the overarching benefits and lack of reported side effects, particularly for hypertensive patients, health care providers and clinicians should consider the use of psyllium supplementation for the treatment or abatement of hypertension, or hypertensive symptoms.❞
Read in full: The effect of psyllium supplementation on blood pressure: a systematic review and meta-analysis of randomized controlled trials ← you can see the concrete numbers here
Is it safe?
Psyllium is first and foremost a foodstuff, and is considered very safe unless you have an allergy (which is rare, but possible).
However, it is still recommended to start at a low dose and work up, because anything that changes your gut microbiota, even if it changes it for the better, will be easiest if done slowly (or else, you will hear about it from your gut).
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Share This Post
-
How To Reduce Your Alzheimer’s Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reduce Your Alzheimer’s Risk
Alzheimer’s is just one cause of dementia, but it’s a very notable one, not least of all because it’s
- a) the most common cause of dementia, and
- b) a measurably terminal disease.
For that reason we’re focusing on Alzheimer’s today, although most of the advice will go for avoiding dementia in general.
First, some things not everyone knows about Alzheimer’s:
- Alzheimer’s is a terminal disease.
- People who get a diagnosis at age 60 are typically given 4–8 years to live.
- Some soldier on for as many as 20, but those are rare outliers.
- Alzheimer’s begins 20 years or more before other symptoms start to develop.
- This makes this information very relevant for younger people approaching 40, for example.
- Alzheimer’s accounts for 60–80% of dementia, and affects around 6% of people over 60.
- By the age of 65, that figure is 10%. By the age of 70, however, the percentage is still about the same—this is because of the mortality rate preventing the accumulation of Alzheimer’s patients over time.
Want to know more? Read: 2023 Alzheimer’s Disease Facts And Figures Special Report ← this is a very comprehensive downloadablereference, by the way, including a lot of information about diagnosis, treatmentpathways, and earlyinterventions.
Speaking of diagnosis…
Know what the symptoms are… and aren’t!
Forgetting your car keys can be frustrating. Forgetting them frequently can be worrying.
But: there’s a difference between forgetting your car keys, and forgetting what car keys are used for. The latter is the kind of memory loss that’s more of a red flag for Alzheimer’s.
Similarly: forgetting someone’s name can be embarrassing. Forgetting someone’s name, asking them, forgetting asking them, asking them again, forgetting again (lather rinse repeat) is more of a red flag for Alzheimer’s.
There are other symptoms too, some of them less commonly known:
❝Difficulty remembering recent conversations, names or events; apathy; and depression are often early symptoms. Communication problems, confusion, poor judgment and behavioral changes may occur next. Difficulty walking, speaking, and swallowing are common in the late stages of the disease❞
If you or a loved one are experiencing worrying symptoms: when it comes to diagnosis and intervention, sooner is a lot better than later, so do talk to your doctor.
As for reducing your risk? First, the obvious stuff:
The usual 5 things that go for almost everything:
- Have a good diet—the Mediterranean Diet is once again recommended (we expect this will not be a surprise to regular readers!)
- Get regular exercise—in the case of avoiding Alzheimer’s and other dementias, typically the most important thing here is heart health, so getting regular cardiovascular exercise, such walking, running, or dancing is great. Cycling too. Swimming, not so much. Not that swimming’s bad or anything, it’s just that when your body is horizontal, the heart has less work to do, especially in the upper part of the body, because it’s not defying gravity. Similarly, yoga is great for the health but won’t particularly help with this, nor will weight training.
- Get good sleep—as we get older, we tend to need less sleep, and tend more towards the lower end of the standard “7–9 hours” prescription, but getting at least those 7 hours makes a huge difference.
- Cut down (or eliminate) alcohol consumption—and especially avoid binge-drinking. While “binge-drinking” is typically associated with young people, that Christmas party where that one uncle gets very drunk is also binge-drinking, for example. Plus, heavy drinking in early life has also been correlated with higher risk of Alzheimer’s later.
- Don’t smoke. It’s bad for everything, and Alzheimer’s risk is no exception.
How much do lifestyle changes alone make a difference?
They make a big difference. This 2022 population-based cohort study (so: huge sample size) looked at people who had 4–5 of the healthy lifestyle factors being studied, vs people who had 0–1 of them. They found:
❝A healthy lifestyle was associated with a longer life expectancy among men and women, and they lived a larger proportion of their remaining years without Alzheimer’s dementia.❞
The numbers of years involved by the way ranged between 3 and 20 years, in terms of life expectancy and years without or with Alzheimer’s, with the average increase of healthy life years being approximately the same as the average increase in years. This is important, because:
A lot of people think “well if I’m going to go senile, I might as well [unhealthy choice that shortens lifespan]”, but they misunderstand a critical factor:
The unhealthy choices will reduce their healthy life years, and simply bring the unhealthy ones (and subsequent death) sooner. If you’re going to spend your last few years in ill-health, it’s better to do so at 90 than 50.
The other thing you may already know… And a thing about it that not everyone considers:
Keeping cognitively active is important. This much is broadly known by the general public, and to clinicians, this was the fourth “healthy factor” in the list of five (instead of the sleep that we put there, because we were listing the 5 things that go for most preventable health issues).
Everyone leaps to mention sudoku at this point, so if that’s your thing, great, enjoy it! (This writer personally enjoys chess, which isn’t everyone’s cup of tea; if it yours though, you can come join her on Chess.com and we’ll keep sharp together)
But the more parts of your mental faculties you keep active, the better. Remember, brainpower (as with many things in health and life) is a matter of “use it or lose it” and this is on a “per skill” basis!
What this means: doing sudoku (a number-based puzzle game) or chess (great as it may be) won’t help as much for keeping your language skills intact, for example. Given that language skills are one of the most impactful and key faculties to get lost to Alzheimer’s disease, neglecting such would be quite an oversight!
Some good ways to keep your language skills tip-top:
- Read—but read something challenging, if possible. It doesn’t have to be Thomas Scanlon’s What We Owe To Each Other, but it should be more challenging than a tabloid, for example. In fact, on the topic of examples:
- This newsletter is written to be easy to read, while not shying away from complex ideas or hard science. Our mission is literally to “make [well-sourced, science-based] health and productivity crazy simple”.
- But the academic papers that we link? Those aren’t written to be easy to read. Go read them, or at least the abstracts (in academia, an abstract is essentially an up-front summary, and is usually the first thing you’ll see when you click a link to a study or such). Challenge yourself!
- Write—compared to reading/listening, producing language is a (related, but) somewhat separate skill. Just ask any foreign language learner which is more challenging: reading or writing!
- Journaling is great, but writing for others is better (as then you’ll be forced to think more about it)
- Learn a foreign language—in this case, what matters it that you’re practicing and learning, so in the scale of easy to hard, or doesn’t matter if it’s Esperanto or Arabic. Duolingo is a great free resource that we recommend for this, and they have a wide range of extensive courses these days.
Now for the least obvious things…
Social contact is important.
Especially in older age, it’s easy to find oneself with fewer remaining friends and family, and getting out and about can be harder for everyone. Whatever our personal inclinations (some people being more introverted or less social than others), we are fundamentally a social species, and hundreds of thousands of years of evolution have built us around the idea that we will live our lives alongside others of our kind. And when we don’t, we don’t do as well.
See for example: Associations of Social Isolation and Loneliness With Later Dementia
If you can’t get out and about easily:
- Online socialising is still socializing.
- Online community is still community.
- Online conversations between friends are still conversations between friends.
If you don’t have much (or anyone) in the category of friends and family, join Facebook groups related to your interests, for example.
Berries are surprisingly good
^This may read like a headline from 200,000 BCE, but it’s relevant here!
Particularly recommended are:
- blueberries
- blackberries
- raspberries
- strawberries
- cranberries
We know that many of these berries seem to have a shelf-life of something like 30 minutes from time of purchase, but… Frozen and dried are perfectly good nutritionally, and in many cases, even better nutritionally than fresh.
Read: Effect of berry-based supplements and foods on cognitive function: a systematic review
Turmeric’s health benefits appear to include protecting against Alzheimer’s
Again, this is about risk reduction, and turmeric (also called curcumin, which is not the same as cumin) significantly reduces the build-up of amyloid plaques in the brain. Amyloid plaques are part of the progression of Alzheimer’s.
See for yourself: Protective Effects of Indian Spice Curcumin Against Amyloid Beta in Alzheimer’s Disease
If you don’t like it as a spice (and even if you do, you probably don’t want to put it in your food every day), you can easily get it as a supplement in capsule form.
Lower your homocysteine levels
Lower our what now? Homocysteine is an amino acid used for making certain proteins, and it’s a risk factor for Alzheimer’s.
Foods high in folate (and possible other B-vitamins) seem to lower homocysteine levels. Top choices include:
- Leafy greens
- Cruciferous vegetables
- Tomatoes
Get plenty of lutein
We did a main feature about specifically this a little while ago, so we’ll not repeat our work here, but lutein is found in, well, the same things we just listed above, and lower levels of lutein are associated with Alzheimer’s disease. It’s not a proven causative factor—we don’t know entirely what causes Alzheimer’s, just a lot of factors that have a high enough correlation that it’d be remiss to ignore them.
Catch up on our previous article: Brain Food? The Eyes Have It
Share This Post
-
5 Steps To Beat Overwhelm
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing With Overwhelm
Whether we live a hectic life in general, or we usually casually take each day as it comes but sometimes several days gang up on us at once, everyone gets overwhelmed sometimes.
Today we’re going to look at how to deal with it healthily.
Step 1: Start anywhere
It’s easy to get stuck in “analysis paralysis” and not know how to tackle an unexpected large problem. An (unhealthy) alternative is to try to tackle everything at once, and end up doing nothing very well.
Even the most expert juggler will not successfully juggle 10 random things thrown unexpectedly at them.
So instead, just pick any part of the the mountain of to-dos, and start.
If you do want a little more finesse though, check out:
Procrastination, And How To Pay Off The To-Do List Debt
Step 2: Accept what you’re capable of
This one works both ways. It means being aware of your limitations yes, but also, of your actual abilities:
- Is the task ahead of you really beyond what you are capable of?
- Could you do it right now without hesitation if a loved one’s life depended on it?
- Could you do it, but there’s a price to pay (e.g. you can do it but it’ll wipe you out in some other life area)?
Work out what’s possible and acceptable to you, and make a decision. And remember, it could be that someone else could do it, but everyone has taken the “if you want something doing, give it to someone busy” approach. It’s flattering that people have such confidence in our competence, but it is also necessary to say “no” sometimes, or at least enlisting help.
Step 3: Listen to your body
…like a leader listening to an advisory council. Your perception of tiredness, pain, weakness, and all your emotions are simply messengers. Listen to the message! And then say “thank you for the information”, and proceed accordingly.
Sometimes that will be in the way the messengers seem to be hoping for!
Sometimes, however, maybe we (blessed with a weighty brain and not entirely a slave to our limbic system) know better, and know when it’s right to push through instead.
Similarly, that voice in your head? You get to decide where it goes and doesn’t. On which note…
Step 4: Be responsive, not reactive
We wrote previously on the difference between these:
A Bone To Pick… Up And Then Put Back Where We Found It
Measured responses will always be better than knee-jerk reactions, unless it is literally a case of a split-second making a difference. 99% of our problems in life are not so; usually the problem will still be there unchanged after a moment’s mindful consideration, so invest in that moment.
You’ve probably heard the saying “give me six hours to chop down a tree, and I’ll spend the first four sharpening the axe”. In this case, that can be your mind. Here’s a good starting point:
No-Frills, Evidence-Based Mindfulness
And if your mental state is already worse than that, mind racing with threats (real or perceived) and doom-laden scenarios, here’s how to get out of that negative spiral first, so that you can apply the rest of this:
Do remember to turn it on again afterwards, though
Step 5: Transcend discomfort
This is partly a callback to step 3, but it’s now coming from a place of a clear ready mind, so the territory should be looking quite different now. Nevertheless, it’s entirely possible that your clear view shows discomfort ahead.
You’re going to make a conscious decision whether or not to proceed through the discomfort (and if you’re not, then now’s the time to start calmly and measuredly looking at alternative plans; delegating, ditching, etc).
If you are going to proceed through discomfort, then it can help to frame the discomfort as simply a neutral part of the path to getting where you want. Maybe you’re going to be going way out of your comfort zone in order to deal with something, and if that’s the case, make your peace with it now, in advance.
“Certainly it hurts” / “Well, what’s the trick then?” / “The trick, William Potter, is not minding that it hurts”
(lines from a famous scene from the 1962 movie Lawrence of Arabia)
It’s ok to say to yourself (if it’s what you decide is the right thing to do) “Yep, this experience is going to suck terribly, but I’m going to do it anyway”.
See also (this being about Radical Acceptance):
What’s The Worst That Could Happen?
Take care!
Share This Post
Related Posts
-
Reading At Night: Good Or Bad For Sleep? And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would be interested in your views about “reading yourself to sleep”. I find that current affairs magazines and even modern novels do exactly the opposite. But Dickens – ones like David Copperfield and Great Expectations – I find wonderfully effective. It’s like entering a parallel universe where none of your own concerns matter. Any thoughts on the science that may explain this?!❞
Anecdotally: this writer is (like most writers) a prolific reader, and finds reading some fiction last thing at night is a good way to create a buffer between the affairs of the day and the dreams of night—but I could never fall asleep that way, unless I were truly sleep-deprived. The only danger is if I “one more chapter” my way deep into the night! For what it’s worth, bedtime reading for me means a Kindle self-backlit with low, soft lighting.
Scientifically: this hasn’t been a hugely researched area, but there are studies to work from. But there are two questions at hand (at least) here:
- one is about reading, and
- the other is about reading from electronic devices with or without blue light filters.
Here’s a study that didn’t ask the medium of the book, and concluded that reading a book in bed before going to sleep improved sleep quality, compared to not reading a book in bed:
Here’s a study that concluded that reading on an iPad (with no blue light filter) that found no difference in any metrics except EEG (so, there was no difference on time spent in different sleep states or sleep onset latency), but advised against it anyway because of the EEG readings (which showed slow wave activity being delayed by approximately 30 minutes, which is consistent with melatonin production mechanics):
Here’s another study that didn’t take EEG readings, and/but otherwise confirmed no differences being found:
We’re aware this goes against general “sleep hygiene” advice in two different ways:
- General advice is to avoid electronic devices before bedtime
- General advice is to not do activities besides sleep (and sex) in bed
…but, we’re committed to reporting the science as we find it!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fix Tight Hamstrings In Just 3 Steps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a better way to increase your flexibility than just stretching and stretching and hoping for the best. Here’s a 3-step method that will transform your flexibility:
As easy as 1-2-3
Only one part actually involves stretching:
Step 1: reciprocal inhibition
- Concept: when one muscle contracts, the opposing muscle relaxes—which is what we need.
- Goal: engage hip flexors to encourage hamstring relaxation.
- Method:
- Kneeling hamstring stretch position with one leg forward.
- Support with yoga blocks or a chair; use a cushion for comfort.
- Maintain a slight arch in the lower back and hinge forward slightly.
- Attempt to lift the foot off the floor, even if it doesn’t move.
- Hold for around 10 seconds.
Step 2: engaging more muscle fibers
- Concept: our muscles contain a lot of fibers, and often not all of them come along for the ride when we do something (exercising, stretching, etc), and those fibers that weren’t engaged will hold back the whole process.
- Goal: activate more fibers in the hamstring for a deeper stretch.
- Method:
- Same kneeling position, slight back arch, and forward hinge.
- Drive the heel into the floor as if trying to dent it.
- Apply significant effort but hold for only 10 seconds.
- A small bend in the knee is acceptable.
Step 3: manipulating the nervous system
- Concept: the nervous system often limits flexibility due to safety signals (causing sensations of discomfort to tell us to stop a lot sooner than we really need to).
- Goal: passive stretching to reduce nervous system resistance.
- Method:
- Avoid muscle engagement or movement—stay completely relaxed.
- Focus on calmness, with slow, steady breaths.
- Avoid signs of tension (e.g. clenched fists, short/sharp breathing). While your nervous system is trying to communicate to you that you are in danger, you need to communicate to your nervous system that this is fine actually, so in order to reassure your nervous system you need to avoid signs that will tip it off that you’re worried too.
- Don’t overstretch; prioritize a relaxed, safe feeling.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Tight Hamstrings? Here’s A Test To Know If It’s Actually Your Sciatic Nerve
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s Sex Differences May Not Be What They Appear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alzheimer’s Sex Differences May Not Be What They Appear
Women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
So… Why?
There are many potential things to look at, but four stand out for quick analysis:
- Chromosomes: women usually have XX chromosomes, to men’s usual XY. There are outliers to both groups, people with non-standard combinations of chromosomes, but not commonly enough to throw out the stats.
- Hormones: women usually have high estrogen and low testosterone, compared to men. Again there are outliers and this is a huge oversimplification that doesn’t even look at other sex hormones, but broadly speaking (which sounds vague, but is actually what is represented in epidemiological studies), it will be so.
- Anatomy: humans have some obvious sexual dimorphism (again, there are outliers, but again, not enough to throw out the stats); this seems least likely to be relevant (Alzheimer’s is probably not stored in the breasts, for examples), though average body composition (per muscle:fat ratio) could admittedly be a factor.
- Social/lifestyle: once again, #NotAllWomen etc, but broadly speaking, women and men often tend towards different social roles in some ways, and as we know, of course lifestyle can play a part in disease pathogenesis.
As a quick aside before we continue, if you’re curious about those outliers, then a wiki-walk into the fascinating world of intersex conditions, for example, could start here. But by and large, this won’t affect most people.
So… Which parts matter?
Back in 2018, Dr. Maria Teresa Ferretti et al. kicked up some rocks in this regard, looking not just at genes (as much research has focussed on) or amyloid-β (again, well-studied) but also at phenotypes and metabolic and social factors—bearing in mind that all three of those are heavily influenced by hormones. Noting, for example, that (we’ll quote directly here):
- Men and women with Alzheimer disease (AD) exhibit different cognitive and psychiatric symptoms, and women show faster cognitive decline after diagnosis of mild cognitive impairment (MCI) or AD dementia.
- Brain atrophy rates and patterns differ along the AD continuum between the sexes; in MCI, brain atrophy is faster in women than in men.
- The prevalence and effects of cerebrovascular, metabolic and socio-economic risk factors for AD are different between men and women.
See: Sex differences in Alzheimer disease—the gateway to precision medicine
So, have scientists controlled for each of those factors?
Mostly not! But they have found clues, anyway, while noting the limitations of the previous way of conducting studies. For example:
❝Women are more likely to develop Alzheimer’s disease and experience faster cognitive decline compared to their male counterparts. These sex differences should be accounted for when designing medications and conducting clinical trials❞
~ Dr. Feixiong Cheng
Read: Research finds sex differences in immune response and metabolism drive Alzheimer’s disease
Did you spot the clue?
It was “differences in immune response and metabolism”. These things are both influenced by (not outright regulated by, but strongly influenced by) sex hormones.
❝As [hormonal] sex influences both the immune system and metabolic process, our study aimed to identify how all of these individual factors influence one another to contribute to Alzheimer’s disease❞
~ Dr. Justin Lathia
Ignoring for a moment progesterone’s role in metabolism, estrogen is an immunostimulant and testosterone is an immunosuppressant. These thus both also have an effect in inflammation, which yes, includes neuroinflammation.
But wait a minute, shouldn’t that mean that women are more protected, not less?
It should! Except… Alzheimer’s is an age-related disease, and in the age-bracket that generally gets Alzheimer’s (again, there are outliers), menopause has been done and dusted for quite a while.
Which means, and this is critical: post-menopausal women not on HRT are essentially left without the immune boost usually directed by estrogen, while men of the same age will be ticking over with their physiology that (unlike that of the aforementioned women) was already adapted to function with negligible estrogen.
Specifically:
❝The metabolic consequences of estrogen decline during menopause accelerate neuropathology in women❞
~ Dr. Rasha Saleh
Critical idea to take away from all this:
Alzheimer’s research is going to be misleading if it doesn’t take into account sex differences, and not just that, but also specifically age-relevant sex differences—because that can flip the narrative. If we don’t take age into account, we could be left thinking estrogen is to blame, when in fact, it appears to be the opposite.
In the meantime, if you’re a woman of a certain age, you might talk with a doctor about whether HRT could be beneficial for you, if you haven’t already:
❝Women at genetic risk for AD (carrying at least one APOE e4 allele) seem to be particularly benefiting from MHT❞
(MHT = Menopausal Hormone Therapy; also commonly called HRT, which is the umbrella term for Hormone Replacement Therapies in general)
~ Dr. Herman Depypere
Source study: Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease
Pop-sci press release version: HRT could ward off Alzheimer’s among at-risk women
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: