Built to Move – by Kelly starrett & Juliet Starrett
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In our everyday lives, for most of us anyway, it’s not too important to be able to run a marathon or leg-press a car. Rather more important, however, are such things as:
- being able to get up from the floor comfortably
- reach something on a high shelf without twinging a shoulder
- being able to put our socks on without making a whole plan around this task
- get accidentally knocked by an energetic dog or child and not put our back out
- etc
Starrett and Starrett, of “becoming a supple leopard” fame, lay out for us how to make sure our mobility stays great. And, if it’s not already where it needs to be, how to get there.
The “ten essential habits” mentioned in the subtitle “ten essential habits to help you move freely and live fully”, in fact also come with ten tests. No, not in the sense of arduous trials, but rather, mobility tests.
For each test, it’s explained to us how to score it out of ten (this is an objective assessment, not subjective). It’s then explained how to “level up” whatever score we got, with different advices for different levels of mobility or immobility. And if we got a ten, then of course, we just build the appropriate recommended habit into our daily life, to keep it that way.
The writing style is casual throughout, and a strong point of the book is its very clear illustrations, too.
Bottom line: if you’d like to gain/maintain good mobility (at any age), this book gives a very reliable outline for doing so.
Click here to check out Built to Move, and take care of your body!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Your Metabolism Says About How Aggressive Breast Cancer Is Likely To Be For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ll get straight to it:
More than 120 million Americans have diabetes or pre-diabetes, and Triple-Negative Breast Cancer (TNBC)* is the most aggressive breast cancer form.
These may seem like unrelated statements, until we consider that patients with obesity-driven** diabetes have much worse TNBC outcomes.
*The “triple-negative” refers to:
- the cancer cells don’t have estrogen receptors
- the cancer cells don’t have progesterone receptors
- the cancer cells don’t make the protein HER2, or at least not in clinically relevant amounts.
**with regard to “obesity-driven”, that is what it is called, and the presence of excess fat does play an important role as we will see, but the fundamental culprit is insulin resistance, as we will also see.
The connection
Superficially, the connection between obesity-driven diabetes and worse TNBC outcomes could be put down to “a person who is already unhealthy will generally fare worse in most health things than an otherwise healthy person”. And, in and of itself, that’s a fair point. Comorbidities certainly do tend to flock together and make each other worse.
On the flipside, this does also mean that the more points of good health we have in our favor, the greater our chances of faring better if something (such as a cancer) does strike us regardless. So, there’s a fair motivation to always keep on top of all aspects of health, so far as reasonably possible.
However, there’s more to it than that.
Dr. Naomi Ko et al., a team of researchers at Boston University, found that diabetes alters breast cancer biology, making TNBC more aggressive and increasing the risk of brain metastasis (i.e., the cancer spreading to the brain).
Specifically, exosomes from fat cells carry microRNAs that worsen TNBC behavior, enhancing the cancer’s:
- cell growth
- movement
- survival under stress
- brain colonization
This also means that certain microRNA patterns predict breast cancer progression and/or survival.
You can find the paper itself here:
Insulin Resistance Increases TNBC Aggressiveness and Brain Metastasis via Adipocyte-derived Exosomes
Why this matters
The researchers argue that their findings suggest the need for special monitoring and treatment for TNBC patients with metabolic disorders like diabetes, and that treating underlying conditions (such as diabetes) alongside cancer is likely to improve outcomes.
On an individual level rather than systemic (assuming you, dear reader, to be a private individual who is not, for example, in charge of health policy for a region, or something like that), what this means is:
We must avoid carrying too much excess fat yes, and/but we must also particularly focus on avoiding/reversing insulin resistance, which can be a silent killer even without excess adiposity, because the noticeable signs and symptoms (including blood sugar irregularities) occur only well into insulin resistance, when the poor overworked pancreas can no longer crank out enough insulin to keep things ticking over.
With that in mind, do check out in particular the two following articles:
How To Lose Weight (Healthily!) ← if applicable. If on the other hand you’re already in the “healthy” body fat percentage range of 20–25% for women or 15–20% for men, then losing what fat you have will not be beneficial, and may even be harmful, depending on other factors.
How To Avoid & Reverse Insulin Resistance ← this one’s super-important!
And of course:
How To Triple Your Breast Cancer Survival Chances
And if you want to get really well-informed, then we highly recommend checking out:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Share This Post
-
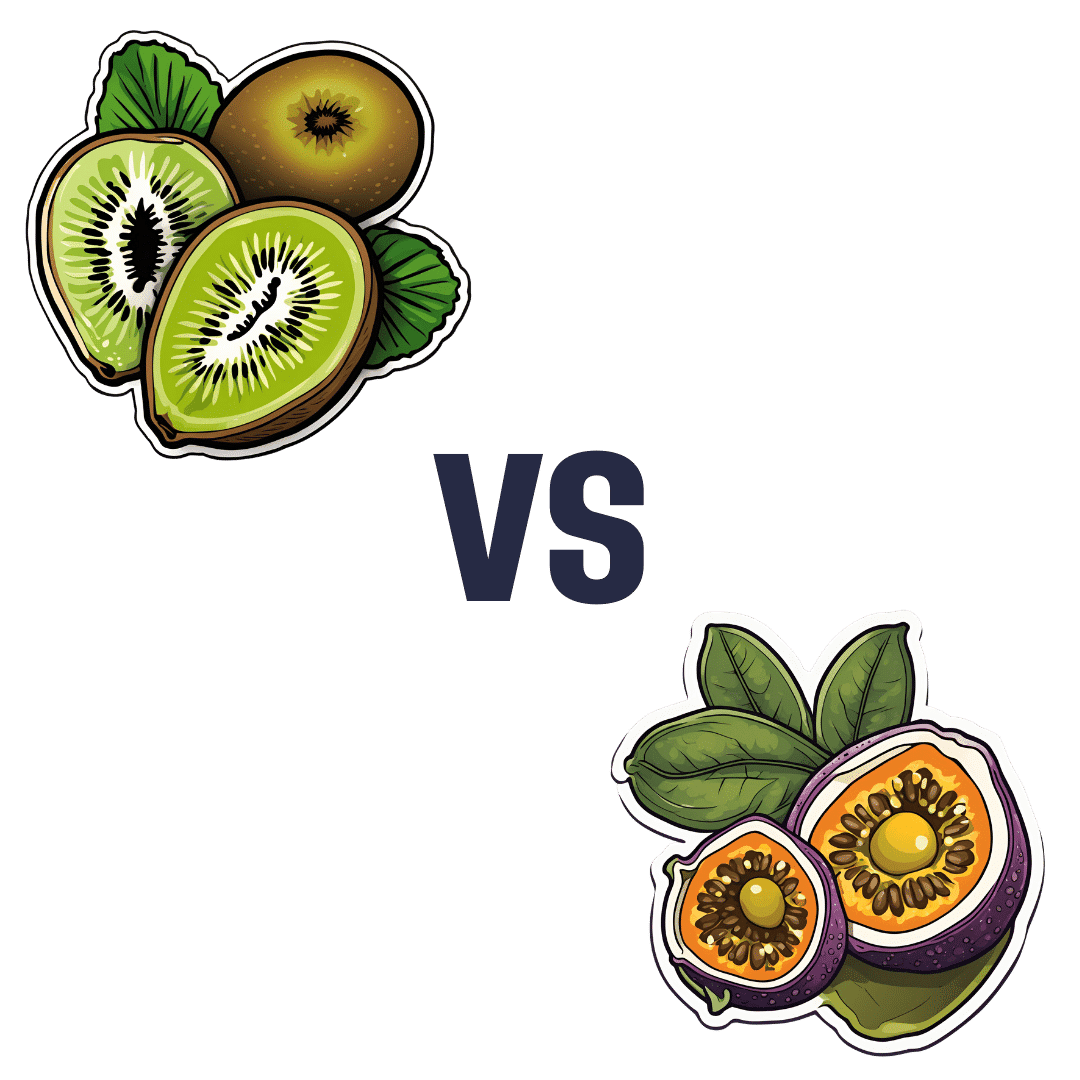
Kiwi vs Passion Fruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to passion fruit, we picked the passion fruit.
Why?
This fruit is so passionate about delivery nutrient-dense goodness, that at time of writing, nothing has beaten it yet!
In terms of macros, passion fruit has a little more protein, as well as 50% more carbs, and/but more than 3x the fiber. That last stat is particularly impressive, and also results in passion fruit having a much lower glycemic index, too. In short, a clear win for passion fruit in the macros category.
In the category of vitamins, kiwi has more of vitamins B9, C, E, and K, while passion fruit has more of vitamins A, B2, B3, and B6, making for a tie this time.
As for minerals, kiwi has more calcium, copper, manganese, and zinc, while passion fruit has more iron, magnesium, phosphorus, potassium, and selenium, resulting in a modest, marginal win for passion fruit in this category.
Adding up the categories gives a convincing win for passion fruit, but by all means enjoy either or both; diversity is good! And kiwi has its merits too (for example, it’s particularly high in vitamin K, appropriately enough).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Share This Post
-
Beyond Burger vs Beef Burger – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing the Beyond Burger to a grass-fed beef burger, we picked the Beyond Burger—but it was very close.
Why?
The macronutrient profiles of the two are almost identical, including the amount of protein, the amount of fat, and the amount of that fat that’s saturated.
Where they stand apart is in two ways:
1) Red meat is classed as a group 2A carcinogen
2) The Beyond Burger contains more sodium (about 1/5 of the daily allowance according to the AHA, or 1/4 of the daily allowance according to the WHO)Neither of those things are great, so how to decide which is worse?
• Cancer and heart disease are both killers, with heart disease claiming more victims.
• However, we do need some sodium to live, whereas we don’t need carcinogens to live.Tie-breaker: the sodium content in the Beyond Burger is likely to be offset by the fact that it’s a fully seasoned burger and will be eaten as-is, whereas the beef burger will doubtlessly have seasonings added before it’s eaten—which may cause it to equal or even exceed the salt content of the Beyond Burger.
The cancer risk for the beef burger, meanwhile, stays one-sided.
One thing’s for sure though: neither of them are exactly a cornerstone of a healthy diet, and either are best enjoyed as an occasional indulgence.
Some further reading:
• Lesser-Known Salt Risks
• Food Choices And Cancer Risk
• Hypertension: Factors Far More Relevant Than SaltShare This Post
Related Posts
-
Ridged Nails: What Are They Telling You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Yaseen Arsalan, a Doctor of Pharmacy, has advice on the “nutraceutical” side of things:
Onychorrhexis
Sounds like the name of a dinosaur, but it’s actually the condition that creates the vertical ridges that sometimes appear on nails. It’s especially likely in the case of thinner nails, and/or certain nutritional deficiencies. Overuse of certain chemicals (including nail polish remover, hair products that get on your hands a lot, and cleaning fluids) can also cause it. It can also be worsened by various conditions, including eczema, psoriasis, hypothyroidism, anemia, and amyloidosis, but it won’t usually be outright caused by those alone.
There are two main kinds of ridges on nails:
- Vertical ridges: associated with hypothyroidism, anemia, and aging. Often an indicator of low iron.
- Horizontal ridges (Beau’s lines): caused by interrupted nail growth, brute force trauma, chemotherapy, acrylic nails, and gel nail polishes. Can also be an indicator of low zinc.
There are an assortment of medical treatments available, which Dr. Arsalan discusses in the video, but for home remedy treatment, he recommends:
- Nail-strengthening creams (look for coconut oil, shea butter, beeswax, vitamin E)
- Hydration (this is about overall hydration e.g. water intake)
- Careful nail trimming (fingernails with a curved shape and toenails straight across)
- Nail ridge filler (he recommends the brand Barrielle, for not containing formaldehyde or formalin)
- Moisturization (with cuticle oil or hand creams, because that hydration we talked about earlier is important, and we want it to stay inside the nail)
For more on those things, plus the medical treatments plus other “how to avoid this” measures, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Counterintuitive Dos and Don’ts of Nail Health
- Regular Nail Polish vs Gel Nail Polish – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do You Know Which Supplements You Shouldn’t Take Together? (10 Pairs!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. LeGrand Peterson wants us to get the most out of our supplements, so watch out for these…
Time to split up some pairs…
In most cases these are a matter of competing for absorption; sometimes to the detriment of both, sometimes to the detriment of one or the other, and sometimes, the problem is entirely different and they just interact in a way that could potentially cause other problems. Dr. Peterson advises as follows:
- Vitamin C and vitamin B12: taking these together can reduce the absorption of Vitamin B12, as vitamin C can overpower it.
- Vitamin C and copper: high amounts of vitamin C can decrease copper absorption, especially in those who are severely copper deficient.
- Magnesium and calcium: these two minerals compete for absorption in the intestines, potentially reducing the effectiveness of both.
- Calcium and iron: calcium can decrease iron absorption, so they should not be taken together, especially if you are iron deficient.
- Calcium and zinc: calcium also competes with zinc, reducing zinc absorption; they should be taken at different times.
- Zinc and copper: zinc and copper compete for absorption, so they should be taken at separate times.
- Iron and zinc: iron can decrease zinc absorption, and thus, they should not be taken together.
- Iron and green tea: perhaps a surprising one, but green tea can reduce iron absorption, so they should not be taken simultaneously.
- Vitamin E and vitamin K: vitamin E increases bleeding risk, while vitamin K promotes clotting, making them opposites and risky to take together.
- Fish oil and ginkgo biloba: both are anticoagulants and can increase the risk of bleeding, especially if taken with blood thinners like warfarin.
If you need to take supplements that compete (or conflict or otherwise potentially adversely interact) with each other, it’s recommended to separate them by at least 4 hours, or better yet, take one in the morning and the other at night. If in doubt, do speak with your pharmacist or doctor for personalized advice
You may be thinking: half my foods contain half of these nutrients! And yes, assuming you have a nutritionally dense diet, this is probably the case. Foods typically release nutrients more slowly than supplements, and unlike supplements, do not usually contain megadoses (although they can, such as the selenium content of Brazil nuts, or vitamin A in carrots). Basically, food is in most cases safer and gentler than supplements. If concerned, do speak with your nutritionist or doctor for personalized advice.
For more information on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Do We Need Supplements, And Do They Work?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lower Your Cortisol! (Here’s Why & How)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cortisol, or “the stress hormone” to its friends, is produced by your adrenal glands, and is generally considered “not fun”.
It does serve a purpose, of course, just like almost everything else our body does. It serves as part of the “fight or flight” response, for example, and helps you to wake up in the morning.
While you do need some cortisol (and a small percentage of people have too little), most of us have too much.
Why? Simply put, modern life is not what 200,000* years of human evolution prepared us for:
- Agriculture (which allowed us to settle down and cease being nomadic) happened during the last 6% of those 200,000 years.
- The Industrial Revolution and the onset of modern capitalism happened during only during the last 0.1% of those 200,000 years.
*the 200,000 years figure is conservative and doesn’t take into account the 200,000,000 years of pre-hominid mammalian evolution. Doing so, on the basis of the mammalian brain & physiology being what’s important here, means our modern stressors have been around for <0.0001% of the time we have.
So guess what, our bodies haven’t caught up. As far as our bodies are concerned, we are supposed to be enjoying the sunshine of grassy plains and the shade of woodland while eating fruit.
- When the alarm clock goes off, our body panics and prepares us to either flee or help fight the predator, because why else would we have been woken so?
- When we have a pressing deadline for work, our brain processes this as “if we don’t do this, we will literally starve and die”.
- When people are upset or angry with us, there’s a part of our brain that fears exile from the tribe and resultant death.
…and so on.
Health Risks of High Cortisol
The long-term stressors are the biggest issue for health. Unless you have a heart condition or other relevant health problem, almost anyone can weather a brief unpleasant surprise. But if something persists? That prompts the body to try to protect you, bless it. The body’s attempts backfire, because…
- One way it does this by making sure to save as much food as possible in the form of body fat
- It’ll also increase your appetite, to make sure you eat anything you can while you still can
- It additionally tries to protect you by keeping you on the brink of fight-or-flight readiness, e.g:
- High blood pressure
- High blood sugar levels
- Rapid mood changes—gotta be able to do those heel-turns as necessary and react quickly to any possible threat!
Suffice it to say, these things are not good for your long-term health.
That’s the “Why”—now here’s the “How”:
Lowering your cortisol levels mostly means lowering your stress and/or lowering your stress response. We previously gave some powerful tools for lowering anxiety, which for these purposes amounts to the same thing.
However, we can also make nutritional and lifestyle changes that will reduce our cortisol levels, for example:
- Reduce (ideally: eliminate from your lifestyle) caffeine
- Reduce (ideally: eliminate from your lifestyle) alcohol
- Yes, really. While many understandably turn to alcohol specifically to help manage stress, it only makes it worse long-term.
- Additionally, alcohol directly stimulates cortisol production, counterintuitive as that may be.
Read: Alcohol, Aging, and the Stress Response ← full article (with 37 sources of its own) from the NYMC covering how alcohol stimulates cortisol production and what that means for us
As well as reductions/eliminations, are some things you can add into your lifestyle that will help!
We’ve written previously about some:
Read: Ashwagandha / Read: L-Theanine / Read: CBD Oil
Other things include, no surprises here:
- The Mediterranean diet (nutritious and delicious): https://10almonds.com/mediterranean-diet
- Get 7–9 hours (good quality!) sleep per night: https://10almonds.com/time-pillow-talk
- Get regular exercise (the regularity matters most!): https://10almonds.com/keep-on-keeping-on
Progressive Relaxation
We’ll give this one its own section because we’ve not talked about it before. Maybe you’re familiar. If not, then in a nutshell: progressive relaxation means progressively tensing and then relaxing each part of your body in turn.
Why does this work? Part of it is just a physical trick involving biofeedback and the natural function of muscles to contract and relax in turn, but the other part is even cleverer:
It basically tricks the most primitive part of your brain, the limbic system, into thinking you had a fight and won, telling it “thank you very much for the cortisol but we don’t need it anymore”.
Take a Hike! Or a Stroll… You Do You!
Last but not least: go connect with your roots. Spend time in the park, or at least the garden. Have a picnic, if the weather suits. Go somewhere you can spend time around leafy green things under a blue sky (we realize the blue sky may be subject to availability in some locations, but do what you can!).
Remember also: just as your body’s responses will be tricked by the alarm clock or the housework, they will also be easily tricked by blue and green stuff around you. If a sunny garden isn’t available in your location, a picture of one as your desktop background is the next best thing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: