You could be stress eating these holidays – or eating your way to stress. 5 tips for the table
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The holiday season can be a time of joy, celebration, and indulgence in delicious foods and meals. However, for many, it can also be an emotional and stressful period.
This stress can manifest in our eating habits, leading to what is known as emotional or stress eating.
There are certain foods we tend to eat more of when we’re stressed, and these can affect our health. What’s more, our food choices can influence our stress levels and make us feel worse. Here’s how.

Why we might eat more when stressed
The human stress response is a complex signalling network across the body and brain. Our nervous system then responds to physical and psychological events to maintain our health. Our stress response – which can be subtle or trigger a fight-or-flight response – is essential and part of daily life.
The stress response increases production of the hormones cortisol and insulin and the release of glucose (blood sugars) and brain chemicals to meet demand. Eating when we experience stress is a normal behaviour to meet a spike in energy needs.
But sometimes our relationship with food becomes strained in response to different types of stress. We might attach shame or guilt to overeating. And anxiety or insecurity can mean some people under-eat in stressful times.
Over time, people can start to associate eating with negative emotions – such as anger, sadness, fear or worry. This link can create behavioural cycles of emotional eating. “Emotional eaters” may go on to develop altered brain responses to the sight or smell of food.
What stress eating can do to the body
Stress eating can include binge eating, grazing, eating late at night, eating quickly or eating past the feeling of fullness. It can also involve craving or eating foods we don’t normally choose. For example, stressed people often reach for ultra-processed foods. While eating these foods is not necessarily a sign of stress, having them can activate the reward system in our brain to alleviate stress and create a pattern.
Short-term stress eating, such as across the holiday period, can lead to symptoms such as acid reflux and poor sleep – particularly when combined with drinking alcohol.
In the longer term, stress eating can lead to weight gain and obesity, increasing the risks of cancer, heart diseases and diabetes.
While stress eating may help reduce stress in the moment, long-term stress eating is linked with an increase in depressive symptoms and poor mental health.

What we eat can make us more or less stressed
The foods we choose can also influence our stress levels.
Diets high in refined carbohydrates and sugar (such as sugary drinks, sweets, crackers, cakes and most chocolates) can make blood sugar levels spike and then crash.
Diets high in unhealthy saturated and trans fats (processed foods, animal fats and commercially fried foods) can increase inflammatory responses.
Rapid changes in blood sugar and inflammation can increase anxiety and can change our mood.
Meanwhile, certain foods can improve the balance of neurotransmitters in the brain that regulate stress and mood.
Omega-3 fatty acids, found in fish and flaxseeds, are known to reduce inflammation and support brain health. Magnesium, found in leafy greens and nuts, helps regulate cortisol levels and the body’s stress response.
Vitamin Bs, found in whole grains, nuts, seeds, beans and animal products (mostly B12), help maintain a healthy nervous system and energy metabolism, improving mood and cognitive performance.
5 tips for the holiday table and beyond
Food is a big part of the festive season, and treating yourself to delicious treats can be part of the fun. Here are some tips for enjoying festive foods, while avoiding stress eating:
1. slow down: be mindful about the speed of your eating. Slow down, chew food well and put down your utensils after each bite
2. watch the clock: even if you’re eating more food than you normally would, sticking to the same timing of eating can help maintain your body’s response to the food. If you normally have an eight-hour eating window (the time between your first meal and last meal of the day) then stick to this even if you’re eating more
3. continue other health behaviours: even if we are eating more food or different food during the festive season, try to keep up other healthy behaviours, such as sleep and exercise
4. stay hydrated: make sure to drink plenty of fluids, especially water. This helps our body function and can help with feelings of hunger. When our brain gets the message something has entered the stomach (what we drink) this can provide a temporary reduction in feelings of hunger
5. don’t restrict: if we have a big day of eating, it can be tempting to restrict eating in the days before or after. But it is never a good idea to overly constrain food intake. It can lead to more overeating and worsen stress.

Plus 3 bonus tips to manage holiday stress
1. shift your thinking: try reframing festive stress. Instead of viewing it as “something bad”, see it as “providing the energy” to reach your goals, such as a family gathering or present shopping
2. be kind to yourself and others: practise an act of compassion for someone else or try talking to yourself as you would a friend. These actions can stimulate our brains and improve wellbeing
3. do something enjoyable: being absorbed in enjoyable activities – such as crafting, movement or even breathing exercises – can help our brains and bodies to return to a more relaxed state, feel steady and connected.
For support and more information about eating disorders, contact the Butterfly Foundation on 1800 33 4673 or Kids Helpline on 1800 551 800. If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14. In an emergency, call 000.
Saman Khalesi, Senior Lecturer and Discipline Lead in Nutrition, School of Health, Medical and Applied Sciences, CQUniversity Australia; Charlotte Gupta, Senior Postdoctoral Research Fellow, Appleton Institute, HealthWise research group, CQUniversity Australia, and Talitha Best, Professor of Psychology, NeuroHealth Lab, Appleton Institute, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 7 Approaches To Pain Management
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More Than One Way To Kill Pain
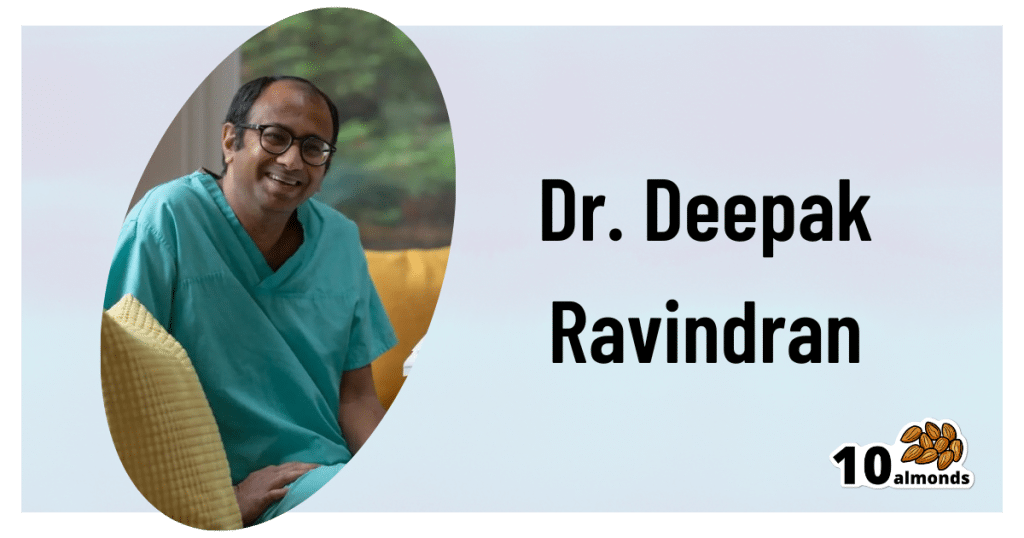
This is Dr. Deepak Ravindran (MD, FRCA. FFPMRCA, EDRA. FIPP, DMSMed). He has decades of experience and is a specialist in acute and chronic pain management, anesthesia, musculoskeletal medicine, and lifestyle medicine.
A quick catch-up, first:
We’ve written about chronic pain management before:
Managing Chronic Pain (Realistically!)
As well as:
Science-Based Alternative Pain Relief
Dr. Ravindran’s approach
Dr. Ravindran takes a “trauma-informed care” approach to his professional practice, and recommends the same for others.
In a nutshell, this means starting from a position of not “what’s wrong with you?”, but rather “what happened to you?”.
This seemingly subtle shift is important, because it means actually dealing with a person’s issues, instead of “take one of these and call my secretary next month”. Read more:
Pain itself can be something of a many-headed hydra. Dr. Ravindran’s approach is equally many-headed; specifically, he has a 7-point plan:
Medications
Dr. Ravindran sees painkillers (and a collection of other drugs, like antidepressants and muscle relaxants) as a potential means to an end worth exploring, but he doesn’t expect them to be the best choice for everyone, and nor does he expect them to be a cure-all. Neither should we. He also advises being mindful of the drawbacks and potential complications of these drugs, too.
Interventions
Sometimes, surgery is the right choice. Sometimes it isn’t. Often, it will change a life—one way or the other. Similar to with medications, Dr. Ravindran is very averse to a “one size fits all” approach here. See also:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Neuroscience and stress management
Often a lot of the distress of pain is not just the pain itself, but the fear associated with it. Will it get worse if I move wrong or eat the wrong thing? How long will it last? Will it ever get better? Will it get worse if I do nothing?. Dr. Ravindran advises tackling this, with the same level of importance as the pain itself. Here’s a good start:
Stress, And Building Psychological Resilience
Diet and the microbiome
Many chronic illnesses are heavily influenced by this, and Dr. Ravindran’s respect for lifestyle medicine comes into play here. While diet might not fix all our ills, it certainly can stop things from being a lot worse. Beyond the obvious “eat healthily” (Mediterranean diet being a good starting point for most people), he also advises doing elimination tests where appropriate, to screen out potential flare-up triggers. You also might consider:
Four Ways To Upgrade The Mediterranean Diet
Sleep
“Get good sleep” is easy advice for those who are not in agonizing pain that sometimes gets worse from staying in the same position for too long. Nevertheless, it is important, and foundational to good health. So it’s important to explore—whatever limitations one might realistically have—what can be done to improve it.
If you can only sleep for a short while at a time, you may get benefit from this previous main feature of ours:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Exercise and movement
The trick here is to move little and often; without overdoing it, but without permitting loss of mobility either. See also:
The Doctor Who Wants Us To Exercise Less, And Move More
Therapies of the mind and body
This is about taking a holistic approach to one’s wellness. In Dr. Ravindran’s words:
❝Mind-body therapies are often an extremely sensitive topic about which people hold very strong opinions and sometimes irrational beliefs.
Some, like reiki and spiritual therapy and homeopathy, have hardly any scientific evidence to back them up, while others like yoga, hypnosis, and meditation/mindfulness are mainstream techniques with many studies showing the benefits, but they all work for certain patients.❞
In other words: evidence-based is surely the best starting point, but if you feel inclined to try something else and it works for you, then it works for you. And that’s a win.
Want to know more?
You might like his book…
The Pain-Free Mindset: 7 Steps to Taking Control and Overcoming Chronic Pain
He also has a blog and a podcast.
Take care!
Share This Post
-
80-Year-Olds Share Their Biggest Regrets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the title, some of these people are a little younger than 80, but this adds to the interest a little as we see the different regrets / learned wisdoms at different stages of later life!
If we could turn back the time…
There are dozens of life regrets / wishes / retroactive advices shared in this video; here are some highlights:
- “My regret was I had a dysfunctional family and I wish I would have learned not to take responsibility.”
- “In my 30s, when I started drinking very heavily, I wish I hadn’t done that because it escalated to drug abuse.”
- “When my parents were old ages, I was working very hard… I didn’t have time to take care of them, not even spend the time with them. That’s my biggest regret.”
- “Live life to the fullest because none of us have any assurance on how old we’re going to be when we’re going to die.”
- “If I could do it over, I would have called home more and realized what my brother was going through.”
- “Spent a lot of years being concerned about what other people thought of me.”
- “You got to be careful what you say to your children because it means a lot.”
For the rest, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Managing Your Mortality Without Regrets
- How To Avoid Carer Burnout (Without Dropping Care)
- Managing Sibling Relationships In Adult Life
- Family Estrangment & How To Fix It
Take care!
Share This Post
-
Pumpkin Protein Crackers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ten of these (give or take what size you make them) will give you the 20g protein that most people’s body’s can use at a time. Five of these plus some of one of the dips we list at the bottom will also do it:
You will need
- 1 cup chickpea flour (also called gram flour or garbanzo bean flour)
- 2 tbsp pumpkin seeds
- 1 tbsp chia seeds
- 1 tsp baking powder
- ¼ tsp MSG or ½ tsp low-sodium salt
- 2 tbsp extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Combine the dry ingredients in a mixing bowl, and mix thoroughly.
3) Add the oil, and mix thoroughly.
4) Add water, 1 tbsp at a time, mixing thoroughly until the mixture comes together and you have a dough ball. You’ll probably need 3–4 tbsp in total, but do add them one at a time.
5) Roll out the dough as thinly and evenly as you can between two sheets of baking paper. Remove the top layer of the paper, and slice the dough into squares or triangles. You could use a cookie-cutter to make other shapes if you like, but then you’ll need to repeat the rolling to use up the offcuts. So we recommend squares or triangles at least for your first go.
6) Bake them in the oven for 12–15 minutes or until golden and crispy. Enjoy immediately or keep in an airtight container.
Enjoy!
Want to learn more?
For those interested in some things to go with what we have going on today:
- Muhammara ← this is a very nutritionally-dense dip (not to mention tasty; seriously, check out these flavors)
- Hero Homemade Hummus ← a classic
- Plant-Based Healthy Cream Cheese ← also a very respectable option
Take care!
Share This Post
Related Posts
-
What happens to your vagina as you age?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The vagina is an internal organ with a complex ecosystem, influenced by circulating hormone levels which change during the menstrual cycle, pregnancy, breastfeeding and menopause.
Around and after menopause, there are normal changes in the growth and function of vaginal cells, as well as the vagina’s microbiome (groups of bacteria living in the vagina). Many women won’t notice these changes. They don’t usually cause symptoms or concern, but if they do, symptoms can usually be managed.
Here’s what happens to your vagina as you age, whether you notice or not.
Let’s clear up the terminology
We’re focusing on the vagina, the muscular tube that goes from the external genitalia (the vulva), past the cervix, to the womb (uterus). Sometimes the word “vagina” is used to include the external genitalia. However, these are different organs and play different roles in women’s health.
What happens to the vagina as you age?
Like many other organs in the body, the vagina is sensitive to female sex steroid hormones (hormones) that change around puberty, pregnancy and menopause.
Menopause is associated with a drop in circulating oestrogen concentrations and the hormone progesterone is no longer produced. The changes in hormones affect the vagina and its ecosystem. Effects may include:
- less vaginal secretions, potentially leading to dryness
- less growth of vagina surface cells resulting in a thinned lining
- alteration to the support structure (connective tissue) around the vagina leading to less elasticity and more narrowing
- fewer blood vessels around the vagina, which may explain less blood flow after menopause
- a shift in the type and balance of bacteria, which can change vaginal acidity, from more acidic to more alkaline.
What symptoms can I expect?
Many women do not notice any bothersome vaginal changes as they age. There’s also little evidence many of these changes cause vaginal symptoms. For example, there is no direct evidence these changes cause vaginal infection or bleeding in menopausal women.
Some women notice vaginal dryness after menopause, which may be linked to less vaginal secretions. This may lead to pain and discomfort during sex. But it’s not clear how much of this dryness is due to menopause, as younger women also commonly report it. In one study, 47% of sexually active postmenopausal women reported vaginal dryness, as did around 20% of premenopausal women.
Other organs close to the vagina, such as the bladder and urethra, are also affected by the change in hormone levels after menopause. Some women experience recurrent urinary tract infections, which may cause pain (including pain to the side of the body) and irritation. So their symptoms are in fact not coming from the vagina itself but relate to changes in the urinary tract.
Not everyone has the same experience
Women vary in whether they notice vaginal changes and whether they are bothered by these to the same extent. For example, women with vaginal dryness who are not sexually active may not notice the change in vaginal secretions after menopause. However, some women notice severe dryness that affects their daily function and activities.
In fact, researchers globally are taking more notice of women’s experiences of menopause to inform future research. This includes prioritising symptoms that matter to women the most, such as vaginal dryness, discomfort, irritation and pain during sex.
If symptoms bother you
Symptoms such as dryness, irritation, or pain during sex can usually be effectively managed. Lubricants may reduce pain during sex. Vaginal moisturisers may reduce dryness. Both are available over-the-counter at your local pharmacy.
While there are many small clinical trials of individual products, these studies lack the power to demonstrate if they are really effective in improving vaginal symptoms.
In contrast, there is robust evidence that vaginal oestrogen is effective in treating vaginal dryness and reducing pain during sex. It also reduces your chance of recurrent urinary tract infections. You can talk to your doctor about a prescription.
Vaginal oestrogen is usually inserted using an applicator, two to three times a week. Very little is absorbed into the blood stream, it is generally safe but longer-term trials are required to confirm safety in long-term use beyond a year.
Women with a history of breast cancer should see their oncologist to discuss using oestrogen as it may not be suitable for them.
Are there other treatments?
New treatments for vaginal dryness are under investigation. One avenue relates to our growing understanding of how the vaginal microbiome adapts and modifies around changes in circulating and local concentrations of hormones.
For example, a small number of reports show that combining vaginal probiotics with low-dose vaginal oestrogen can improve vaginal symptoms. But more evidence is needed before this is recommended.
Where to from here?
The normal ageing process, as well as menopause, both affect the vagina as we age.
Most women do not have troublesome vaginal symptoms during and after menopause, but for some, these may cause discomfort or distress.
While hormonal treatments such as vaginal oestrogen are available, there is a pressing need for more non-hormonal treatments.
Dr Sianan Healy, from Women’s Health Victoria, contributed to this article.
Louie Ye, Clinical Fellow, Department of Obstetrics and Gynecology, The University of Melbourne and Martha Hickey, Professor of Obstetrics and Gynaecology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Spectrum of Hope – by Dr. Gayatri Devi
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about Dr. Devi’s work (See: “Alzheimer’s: The Bad News And The Good“) but she has plenty more to say than we could fit in an article.
The book is written for patients, family/carers, and clinicians—without getting deep into the science, which it is assumed clinicians will know. the general style of the book is pop-science, and it’s more about addressing the misconceptions around Alzheimer’s, rather than focusing on neurological features such as beta amyloid plaques and tau proteins and the like.
Dr. Devi explains a lot about the experience of Alzheimer’s—what to expect, or rather, what to know about in advance. Because, as she explains, there are a lot of different manifestations of Alzheimer’s that are all lumped under the same umbrella.
This means that a person could have negligible memory but perfect language and reasoning skills, or the other way around, or some other combination of symptoms showing up or not.
Which means that any plan for managing one’s Alzheimer’s needs to be adaptable and personalized, which is something Dr. Devi talks us through, too.
Bottom line: if you are a loved one has Alzheimer’s, or you just like to be prepared, this is a great book to prepare anybody for just that.
Click here to check out The Spectrum of Hope, and hold onto that hope!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hope: A research-based explainer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This year, more than 60 countries, representing more than 4 billion people, will hold major elections. News headlines already are reporting that voters are hanging on to hope. When things get tough or don’t go our way, we’re told to hang on to hope. HOPE was the only word printed on President Barack Obama’s iconic campaign poster in 2008.
Research on hope has flourished only in recent decades. There’s now a growing recognition that hope has a role in physical, social, and mental health outcomes, including promoting resilience. As we embark on a challenging year of news, it’s important for journalists to learn about hope.
So what is hope? And what does the research say about it?
Merriam-Webster defines hope as a “desire accompanied by expectation of or belief in fulfillment.” This definition highlights the two basic dimensions of hope: a desire and a belief in the possibility of attaining that desire.
Hope is not Pollyannaish optimism, writes psychologist Everett Worthington in a 2020 article for The Conversation. “Instead, hope is a motivation to persevere toward a goal or end state, even if we’re skeptical that a positive outcome is likely.”
There are several scientific theories about hope.
One of the first, and most well-known, theories on hope was introduced in 1991 by American psychologist Charles R. Snyder.
In a paper published in the Journal of Personality and Social Psychology, Snyder defined hope as a cognitive trait centered on the pursuit of goals and built on two components: a sense of agency in achieving a goal, and a perceived ability to create pathways to achieve that goal. He defined hope as something individualistic.
Snyder also introduced the Hope Scale, which continues to be used today, as a way to measure hope. He suggested that some people have higher levels of hope than others and there seem to be benefits to being more hopeful.
“For example, we would expect that higher as compared with lower hope people are more likely to have a healthy lifestyle, to avoid life crises, and to cope better with stressors when they are encountered,” they write.
Others have suggested broader definitions.
In 1992, Kaye Herth, a professor of nursing and a scholar on hope, defined hope as “a multidimensional dynamic life force characterized by a confident yet uncertain expectation of achieving good, which to the hoping person, is realistically possible and personally significant.” Herth also developed the Herth Hope Index, which is used in various settings, including clinical practice and research.
More recently, others have offered an even broader definition of hope.
Anthony Scioli, a clinical psychologist and author of several books on hope, defines hope “as an emotion with spiritual dimensions,” in a 2023 review published in Current Opinion in Psychology. “Hope is best viewed as an ameliorating emotion, designed to fill the liminal space between need and reality.”
Hope is also nuanced.
“Our hopes may be active or passive, patient or critical, private or collective, grounded in the evidence or resolute in spite of it, socially conservative or socially transformative,” writes Darren Webb in a 2007 study published in History of the Human Sciences. “We all hope, but we experience this most human of all mental feelings in a variety of modes.”
To be sure, a few studies have shown that hope can have negative outcomes in certain populations and situations. For example, one study highlighted in the research roundup below finds that Black college students who had higher levels of hope experienced more stress due to racial discrimination compared with Black students who had lower levels of hope.
Today, hope is one of the most well-studied constructs within the field of positive psychology, according to the journal Current Opinion in Psychology, which dedicated its August 2023 issue to the subject. (Positive psychology is a branch of psychology focused on characters and behaviors that allow people to flourish.)
We’ve gathered several studies below to help you think more deeply about hope and recognize its role in your everyday lives.
Research roundup
The Role of Hope in Subsequent Health and Well-Being For Older Adults: An Outcome-Wide Longitudinal Approach
Katelyn N.G. Long, et al. Global Epidemiology, November 2020.The study: To explore the potential public health implications of hope, researchers examine the relationship between hope and physical, behavioral and psychosocial outcomes in 12,998 older adults in the U.S. with a mean age of 66.
Researchers note that most investigations on hope have focused on psychological and social well-being outcomes and less attention has been paid to its impact on physical and behavioral health, particularly among older adults.
The findings: Results show a positive association between an increased sense of hope and a variety of behavioral and psychosocial outcomes, such as fewer sleep problems, more physical activity, optimism and satisfaction with life. However, there wasn’t a clear association between hope and all physical health outcomes. For instance, hope was associated with a reduced number of chronic conditions, but not with stroke, diabetes and hypertension.
The takeaway: “The later stages of life are often defined by loss: the loss of health, loved ones, social support networks, independence, and (eventually) loss of life itself,” the authors write. “Our results suggest that standard public health promotion activities, which often focus solely on physical health, might be expanded to include a wider range of factors that may lead to gains in hope. For example, alongside community-based health and nutrition programs aimed at reducing chronic conditions like hypertension, programs that help strengthen marital relations (e.g., closeness with a spouse), provide opportunities to volunteer, help lower anxiety, or increase connection with friends may potentially increase levels of hope, which in turn, may improve levels of health and well-being in a variety of domains.”
Associated Factors of Hope in Cancer Patients During Treatment: A Systematic Literature Review
Corine Nierop-van Baalen, Maria Grypdonck, Ann van Hecke and Sofie Verhaeghe. Journal of Advanced Nursing, March 2020.The study: The authors review 33 studies, written in English or Dutch and published in the past decade, on the relationship between hope and the quality of life and well-being of patients with cancer. Studies have shown that many cancer patients respond to their diagnosis by nurturing hope, while many health professionals feel uneasy when patients’ hopes go far beyond their prognosis, the authors write.
The findings: Quality of life, social support and spiritual well-being were positively associated with hope, as measured with various scales. Whereas symptoms, psychological distress and depression had a negative association with hope. Hope didn’t seem to be affected by the type or stage of cancer or the patient’s demographics.
The takeaway: “Hope seems to be a process that is determined by a person’s inner being rather than influenced from the outside,” the authors write. “These factors are typically given meaning by the patients themselves. Social support, for example, is not about how many patients experience support, but that this support has real meaning for them.”
Characterizing Hope: An Interdisciplinary Overview of the Characteristics of Hope
Emma Pleeging, Job van Exel and Martijn Burger. Applied Research in Quality of Life, September 2021.The study: This systematic review provides an overview of the concept of hope based on 66 academic papers in ten academic fields, including economics and business studies, environmental studies, health studies, history, humanities, philosophy, political science, psychology, social science, theology and youth studies, resulting in seven themes and 41 sub-themes.
The findings: The authors boil down their findings to seven components: internal and external sources, the individual and social experience of hope, internal and external effects, and the object of hope, which can be “just about anything we can imagine,” the authors write.
The takeaway: “An important implication of these results lies in the way hope is measured in applied and scientific research,” researchers write. “When measuring hope or developing instruments to measure it, researchers could be well-advised to take note of the broader understanding of the topic, to prevent that important characteristics might be overlooked.”
Revisiting the Paradox of Hope: The Role of Discrimination Among First-Year Black College Students
Ryon C. McDermott, et al. Journal of Counseling Psychology, March 2020.The study: Researchers examine the moderating effects of hope on the association between experiencing racial discrimination, stress and academic well-being among 203 first-year U.S. Black college students. They build on a small body of evidence that suggests high levels of hope might have a negative effect on Black college students who experience racial discrimination.
The authors use data gathered as part of an annual paper-and-pencil survey of first-year college students at a university on the Gulf Coast, which the study doesn’t identify.
The findings: Researchers find that Black students who had higher levels of hope experienced more stress due to racial discrimination compared with students who had lower levels of hope. On the other hand, Black students with low levels of hope may be less likely to experience stress when they encounter discrimination.
Meanwhile, Black students who had high levels of hope were more successful in academic integration — which researchers define as satisfaction with and integration into the academic aspects of college life — despite facing discrimination. But low levels of hope had a negative impact on students’ academic well-being.
“The present study found evidence that a core construct in positive psychology, hope, may not always protect Black students from experiencing the psychological sting of discrimination, but it was still beneficial to their academic well-being,” the authors write.
The takeaway: “Our findings also highlight an urgent need to reduce discrimination on college campuses,” the researchers write. “Reducing discrimination could help Black students (and other racial minorities) avoid additional stress, as well as help them realize the full psychological and academic benefits of having high levels of hope.”
Additional reading
Hope Across Cultural Groups Lisa M. Edwards and Kat McConnell. Current Opinion in Psychology, February 2023.
The Psychology of Hope: A Diagnostic and Prescriptive Account Anthony Scioli. “Historical and Multidisciplinary Perspectives on Hope,” July 2020.
Hope Theory: Rainbows in the Mind C.R. Snyder. Psychological Inquiry, 2002
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: