What To Leave Off Your Table (To Stay Off This Surgeon’s)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why we eat too much (and how we can fix that)
This is Dr. Andrew Jenkinson. He’s a Consultant Surgeon specializing in the treatment of obesity, gallstones, hernias, heartburn and abdominal pain. He runs regular clinics in both London and Dubai. What he has to offer us today, though, is insight as to what’s on our table that puts us on his table, and how we can quite easily change that up.
So, why do we eat too much?
First things first: some metabolic calculations. No, we’re not going to require you to grab a calculator here… Your body does it for you!
Our body’s amazing homeostatic system (the system that does its best to keep us in the “Goldilocks Zone” of all our bodily systems; not too hot or too cold, not dehydrated or overhydrated, not hyperglycemic or hypoglycemic, blood pressure not too high or too low, etc, etc) keeps track of our metabolic input and output.
What this means: if we increase or decrease our caloric consumption, our body will do its best to increase or decrease our metabolism accordingly:
- If we don’t give it enough energy, it will try to conserve energy (first by slowing our activities; eventually by shutting down organs in a last-ditch attempt to save the rest of us)
- If we give it too much energy, it will try to burn it off, and what it can’t burn, it will store
In short: if we eat 10% or 20% more or less than usual, our body will try to use 10% to 20% more or less than usual, accordingly.
So… How does this get out of balance?
The problem is in how our system does that, and how we inadvertently trick it, to our detriment.
For a system to function, it needs at its most base level two things—a sensor and a switch:
- A sensor: to know what’s going on
- A switch: to change what it’s doing accordingly
Now, if we eat the way we’re evolved to—as hunter-gatherers, eating mostly fruit and vegetables, supplemented by animal products when we can get them—then our body knows exactly what it’s eating, and how to respond accordingly.
Furthermore, that kind of food takes some eating! Most fruit these days is mostly water and fiber; in those days it often had denser fiber (before agricultural science made things easier to eat), but either way, our body knows when we are eating fruit and how to handle that. Vegetables, similarly. Unprocessed animal products, again, the gut goes “we know what this is” and responds accordingly.
But modern ultra-processed foods with trans-fatty acids, processed sugar and flour?
These foods zip calories straight into our bloodstream like greased lightning. We get them so quickly so easily and in such great caloric density, that our body doesn’t have the chance to count them on the way in!
What this means is: the body has no idea what it’s just consumed or how much or what to do with it, and doesn’t adjust our metabolism accordingly.
Bottom line:
Evolutionarily speaking, your body has no idea what ultra-processed food is. If you skip it and go for whole foods, you can, within the bounds of reason, eat what you like and your body will handle it by adjusting your metabolism accordingly.
Now, advising you “avoid ultra-processed foods and eat whole foods” was probably not a revelation in and of itself.
But: sometimes knowing a little more about the “why” makes the difference when it comes to motivation.
Want to know more about Dr. Jenkinson’s expert insights on this topic?
If you like, you can check out his website here—he has a book too
Why We Eat (Too Much) – Dr. Andrew Jenkinson on the Science of Appetite
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 10 Causes Of High Blood Pressure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As Dr. Frita Fisher explains, these are actually the top 10 known causes of high blood pressure. Number zero on the list would be “primary hypertension”, which means high blood pressure with no clear underlying cause.
Superficially, this feels a little like the sometime practice of writing the catch-all “heart failure” as the cause of death on a death certificate, because yes, that heart sure did stop beating. But in reality, primary hypertension is most likely often caused by such things as unmanaged chronic stress—something that doesn’t show up on most health screenings.
Dr. Fisher’s Top 10
- Thyroid disease: both hyperthyroidism and hypothyroidism can cause high blood pressure.
- Obstructive sleep apnea: characterized by snoring, daytime sleepiness, and headaches, this condition can lead to hypertension.
- Chronic kidney disease: diseases ranging from diabetic nephropathy to renal vascular disease can cause high blood pressure.
- Elevated cortisol levels: conditions like Cushing’s syndrome or disease, which involve high cortisol levels, can lead to hypertension—as can a lifestyle with a lot of chronic stress, but that’s less readily diagnosed as such than something one can tell from a blood test.
- Elevated aldosterone levels: excess aldosterone from the adrenal glands causes the body to retain salt and water, increasing blood pressure, because more stuff = more pressure.
- Brain tumor: tumors that increase intracranial pressure can cause a rise in blood pressure to ensure adequate brain perfusion. In these cases, the hypertension is keeping you alive—unless it kills you first. If this seems like a strange bodily response, remember that our bodily response to an infection is often fever, to kill off the infection which can’t survive at such high temperatures (but neither can we, so it becomes a game of chicken with our life on the line), so sometimes our body does kill us with one thing while trying to save us from another.
- Coarctation of the aorta: this congenital heart defect results in narrowing of the aorta, leading to hypertension, especially in the upper body.
- Pregnancy: pregnancy can either induce or worsen existing hypertension.
- Obesity: excess weight increases blood flow and pressure on arteries, raising the risk of hypertension and associated conditions, e.g. diabetes etc.
- Drugs: certain medications and recreational drugs (including, counterintuitively, alcohol!) can elevate blood pressure.
For more information on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Hypertension: Factors Far More Relevant Than Salt
Take care!
Share This Post
-
Don’t Do *This* If You’re Over 50 (And Want Better Sleep)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, sleep specialist, explains:
Don’t make these mistakes
Dr. Breus recommends avoiding…
- Misusing magnesium: magnesium is a helpful sleep aid but must be carefully monitored. Recommended doses are 250mg for women and 300–350 mg for men, with slight adjustments for hot climates or active lifestyles. Overdosing can cause stomach issues, diarrhea, and dehydration, disrupting sleep. He recommends starting with magnesium glycinate for fewer stomach issues, and later mix with magnesium citrate. Always check supplements to avoid excessive magnesium intake.
- Misusing melatonin: melatonin production declines after age 55–60, making low-dose supplementation (0.5–1 mg) beneficial. He recommends, however, avoiding high doses (3–10mg), and he recommends to take it 90 minutes before bedtime. Melatonin interacts with some medications (including some meds for blood pressure or depression), so consult a pharmacist before use to avoid risks like serotonin syndrome.
- Going to bed too early: going to bed too early disrupts circadian rhythms and reduces sleep drive, causing earlier waking. Now, being an “early bird” is a generally healthy thing, but if you’re already getting up at 5am, say, you probably want your schedule to not continue to creep further forwards until you become nocturnal. Set a consistent wake-up time and count 7.5 hours backward (plus a set time to fall asleep, e.g. 20 minutes, but you’ll know what it is for you) to determine bedtime.
- Excessive caffeine consumption: from the heading, it may seem like a no-brainer, but older adults metabolize caffeine 33% slower on average, prolonging its effects. Dr. Breus recommends to reduce intake with “caffeine fading,” switching to half-caffeinated coffee for a while and then considering transitioning to decaf. He also suggests enjoying increasingly lower-caffeine teas, like black tea in the morning, matcha in the afternoon, and herbal tea at night to reduce caffeine’s impact on sleep.
- Falling foul of serotonin: avoid taking 5-HTP supplements with SSRI antidepressants like Prozac or Zoloft due to the risk of serotonin syndrome.
- Consider checking for physical problems: if you regularly wake up tired and/or groggy (despite having ostensibly had enough sleep, and there not being a pharmaceutical explanation for your grogginess), consider screening for sleep apnea. Home sleep tests are a convenient way to identify and treat this common but often undiagnosed condition.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How to Fall Asleep Faster: CBT-Insomnia Treatment
Take care!
Share This Post
-
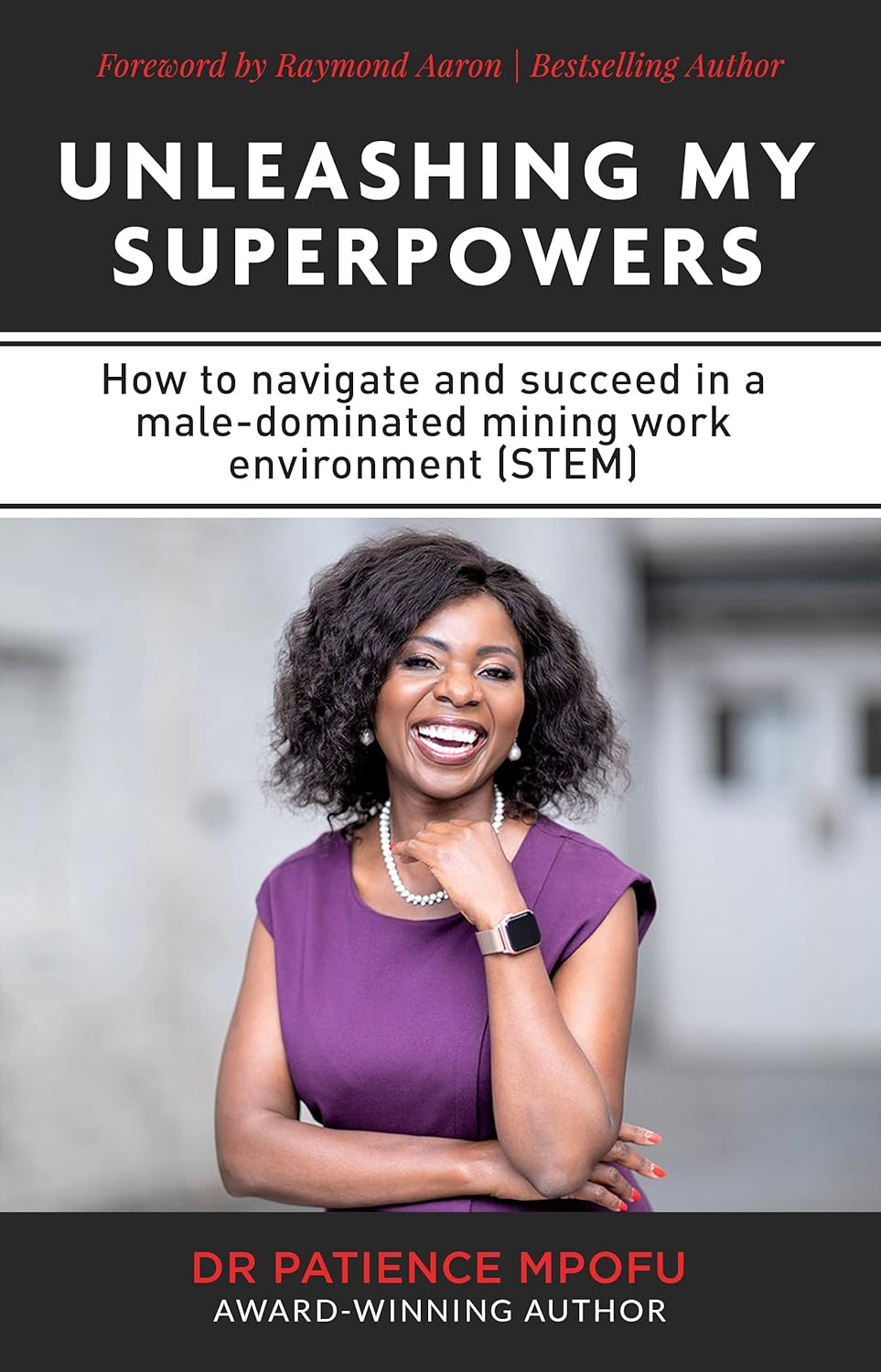
Unleashing My Superpowers – by Dr. Patience Mpofu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Patience Mpofu is on a mission to provide women and girls with the inside-information, knowledge, resources, and strategies to break through the glass ceiling. She writes from her experience in STEM, but her lessons are applicable in any field.
Her advices range from the internal (how to deal with imposter syndrome) to the external (how to overcome cultural biases); she also explains and illustrates the importance of both role models and mentors.
While a lot of the book is half instruction manual, half memoir of her incredible life and career (to illustrate her points), and is well-worth reading—and/or perhaps worth gifting to a girl you know with ambitions in STEM?
Share This Post
Related Posts
-
Tasty Versatile Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the nearish future, we’re going to do some incredible rice dishes, but first we need to make sure we’re all on the same page about cooking rice, so here’s a simple recipe first, to get technique down and work in some essentials. We’ll be using wholegrain basmati rice, because it has a low glycemic index, lowest likelihood of heavy metal contamination (a problem for some kinds of rice), and it’s one of the easiest rices to cook well.
You will need
- 1 cup wholegrain basmati rice (it may also be called “brown basmati rice“; this is the same)
- 1 1/2 cups vegetable stock (ideally you have made this yourself from vegetable offcuts that you saved in the freezer, then it will be healthiest and lowest in sodium; failing that, low-sodium vegetable stock cubes can be purchased at most large supermarkets. and then made up at home with hot water)
- 1 tbsp extra virgin olive oil
- 1 tbsp chia seeds
- 1 tbsp black pepper, coarse ground
- 1 tsp turmeric powder (this small quantity will not change the flavor, but it has important health benefits, and also makes the rice a pleasant golden color)
- 1 tsp garlic powder
- 1 tsp yeast extract (this gently improves the savory flavor and also adds vitamin B12)
- Optional small quantity of green herbs for garnish. Cilantro is good (unless you have the soap gene); parsley never fails.
This is the ingredients list for a super-basic rice that will go with anything rice will go with; another day we can talk more extensive mixes of herbs and spice blends for different kinds of dishes (and different health benefits!), but for now, let’s get going!
Method
(we suggest you read everything at least once before doing anything)
1) Wash the rice thoroughly. We recommend using a made-for-purpose rice-washing bowl (like this one, for example), but failing that, simply rinse it thoroughly with cold water using a bowl and a sieve. You will probably need to rinse it 4–5 times, but with practice, it will only take a few seconds per rinse, and the water will be coming up clear.
2) Warm the pan. It doesn’t matter for the moment whether you’re using an electronic rice cooker, a stovetop pressure cooker, electronic pressure cooker, or just a sturdy pan with a heavy lid available, aside from that if it’s something non-stovetop, you now want it to be on low to warm up already.
3) Separately in a saucepan, bring your stock to a simmer
4) Put the tbsp of olive oil into the pan (even if you’re confident the rice won’t stick; this isn’t entirely about that) and turn up the heat (if it’s a very simple rice cooker, most at least have a warm/cook differentiation; if so, turn it to “cook”). You don’t want the oil to get to the point of smoking, so, to test the temperature as it heats, flick a single drop of water from your fingertip (you did wash your hands first, right? We haven’t been including that step, but please do wash your hands before doing kitchen things) into the pan. If it sizzles, the pan is hot enough now for the next step.
5) Put the rice into the pan. That’s right, with no extra liquid yet; we’re going to toast it for a moment. Stir it a little, for no more than a minute; keep it moving; don’t let it burn! If you try this several times and fail, it could be that you need a better pan. Treat yourself to one when you get the opportunity; until then, skip the toasting part if necessary.
6) Add the chia seeds and spices, followed by the stock, followed by the yeast extract. Why did we do the stock before the yeast extract? It’s because hot liquid will get all the yeast extract off the teaspoon 🙂
7) Put the lid on/down (per what kind of pan or rice cooker you are using), and turn up the heat (if it is a variable heat source) until a tiny bit of steam starts making its way out. When it does, turn it down to a simmer, and let the rice cook. Don’t stir it, don’t jiggle it; trust the process. If you stir or jiggle it, the rice will cook unevenly and, paradoxically, probably stick.
8) Do keep an eye on it, because when steam stops coming out, it is done, and needs taking off the heat immediately. If using an automatic rice cooker, you can be less attentive if you like, because it will monitor this for you.
Note: if you are using a simple pan with a non-fastening lid (any other kind of rice cooking setup is better), more steam will escape than the other methods, and it’s possible that it might run out of steam (literally) before the rice is finished. If the steam stops and you find the rice isn’t done, add a splash of water as necessary (the rice doesn’t need to be submerged, it just needs to have liquid; the steam is part of the cooking process), and make a note of how much you had to add (so that next time you can just add it at the start), and put it back on the heat until it is done.
9) Having taken it off the heat, let it sit for 5 minutes (with the lid still on) before doing any fluffing-up. Then you can fluff-up and serve, adding the garnish if you want one.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Should You Go Light Or Heavy On Carbs?
- Chia: The Tiniest Seeds With The Most Value
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Why Curcumin (Turmeric) Is Worth Its Weight In Gold
- The Many Health Benefits Of Garlic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Much Can Hypnotherapy Really Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sit Back, Relax, And…
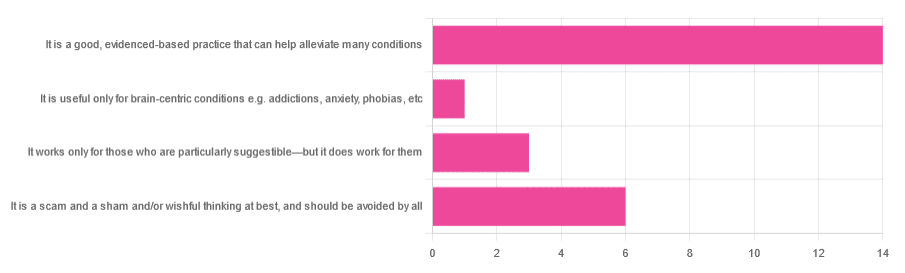
In Tuesday’s newsletter, we asked you for your opinions of hypnotherapy, and got the above-depicted, below-described, set of responses:
- About 58% said “It is a good, evidenced-based practice that can help alleviate many conditions”
- Exactly 25% said “It is a scam and sham and/or wishful thinking at best, and should be avoided by all”
- About 13% said “It works only for those who are particularly suggestible—but it does work for them”
- One (1) person said “It is useful only for brain-centric conditions e.g. addictions, anxiety, phobias, etc”
So what does the science say?
Hypnotherapy is all in the patient’s head: True or False?
True! But guess which part of your body controls much of the rest of it.
So while hypnotherapy may be “all in the head”, its effects are not.
Since placebo effect, nocebo effect, and psychosomatic effect in general are well-documented, it’s quite safe to say at the very least that hypnotherapy thus “may be useful”.
Which prompts the question…
Hypnotherapy is just placebo: True or False?
False, probably. At the very least, if it’s placebo, it’s an unusually effective placebo.
And yes, even though testing against placebo is considered a good method of doing randomized controlled trials, some placebos are definitely better than others. If a placebo starts giving results much better than other placebos, is it still a placebo? Possibly a philosophical question whose answer may be rooted in semantics, but happily we do have a more useful answer…
Here’s an interesting paper which: a) begins its abstract with the strong, unequivocal statement “Hypnosis has proven clinical utility”, and b) goes on to examine the changes in neural activity during hypnosis:
Brain Activity and Functional Connectivity Associated with Hypnosis
It works only for the very suggestible: True or False?
False, broadly. As with any medical and/or therapeutic procedure, a patient’s expectations can affect the treatment outcome.
And, especially worthy of note, a patient’s level of engagement will vastly affect it treatment that has patient involvement. So for example, if a doctor prescribes a patient pills, which the patient does not think will work, so the patient takes them intermittently, because they’re slow to get the prescription refilled, etc, then surprise, the pills won’t get as good results (since they’re often not being taken).
How this plays out in hypnotherapy: because hypnotherapy is a guided process, part of its efficacy relies on the patient following instructions. If the hypnotherapist guides the patient’s mind, and internally the patient is just going “nope nope nope, what a lot of rubbish” then of course it will not work, just like if you ask for directions in the street and then ignore them, you won’t get to where you want to be.
For those who didn’t click on the above link by the way, you might want to go back and have a look at it, because it included groups of individuals with “high/low hypnotizability” per several ways of scoring such.
It works only for brain-centric things, e.g. addictions, anxieties, phobias, etc: True or False?
False—but it is better at those. Here for example is the UK’s Royal College of Psychiatrists’ information page, and if you go to “What conditions can hypnotherapy help to treat”, you’ll see two broad categories; the first is almost entirely brain-stuff; the second is more varied, and includes pain relief of various kinds, burn care, cancer treatment side effects, and even menopause symptoms. Finally, warts and other various skin conditions get their own (positive) mention, per “this is possible through the positive effects hypnosis has on the immune system”:
RCPsych | Hypnosis And Hypnotherapy
Wondering how much psychosomatic effect can do?
You might like this previous article; it’s not about hypnotherapy, but it is about the difference the mind can make on physical markers of aging:
Aging, Counterclockwise: When Age Is A Flexible Number
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Celery vs Radish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to radish, we picked the celery.
Why?
It was very close! And yes, surprising, we know. Generally speaking, the more colorful/pigmented an edible plant is, the healthier it is. Celery is just one of those weird exceptions (as is cauliflower, by the way).
Macros-wise, these two are pretty much the same—95% water, with just enough other stuff to hold them together. The proportions of “other stuff” are also pretty much equal.
In the category of vitamins, celery has more vitamin K while radish has more vitamin C; the other vitamins are pretty close to equal. We’ll call this one a minor win for celery, as vitamin K is found in fewer foods than vitamin C.
When it comes to minerals, celery has more calcium, manganese, phosphorus, and potassium, while radish has more copper, iron, selenium, and zinc. We’ll call this a minor win for radish, as the margins are a little wider for its minerals.
So, that makes the score 1–1 so far.
Both plants have an assortment of polyphenols, of which, when we add up the averages, celery comes out on top by some way. Celery also comes out on top when we do a head-to-head of the top flavonoid of each; celery has 5.15mg/100g of apigenin to radish’s 0.63mg/100g kaempferol.
Which means, both are great healthy foods, but celery wins the day.
Want to learn more?
You might like to read:
Celery vs Cucumber – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: