Vitamin C (Drinkable) vs Vitamin C (Chewable) – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing vitamin C (drinkable) to vitamin C (chewable), we picked the drinkable.
Why?
First let’s look at what’s more or less the same in each:
- The usable vitamin C content is comparable
- The bioavailability is comparable
- The additives to hold it together are comparable
So what’s the difference?
With the drinkable, you also drink a glass of water
If you’d like to read more about how to get the most out of the vitamins you take, you can do so here:
Are You Wasting Your Vitamins? Maybe, But You Don’t Have To
If you’d like to get some of the drinkable vitamin C, here’s an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Over-50s Physio: What My 5 Oldest Patients (Average Age 92) Do Right
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oftentimes, people of particularly advanced years will be asked their secret to longevity, and sometimes the answers aren’t that helpful because they don’t actually know, and ascribe it to some random thing. Will Harlow, the over-50s specialist physio, talks about the top 5 science-based things that his 5 oldest patients do, that enhances the healthy longevity that they are enjoying:
The Top 5’s Top 5
Here’s what they’re doing right:
Daily physical activity: all five patients maintain a consistent habit of daily exercise, which includes activities like exercise classes, home workouts, playing golf, or taking daily walks. They prioritize movement even when it’s difficult, rarely skipping a day unless something serious happened. A major motivator was the fear of losing mobility, as they had seen spouses, friends, or family members stop exercising and never start again.
Stay curious: a shared trait among the patients was their curiosity and eagerness to learn. They enjoy meeting new people, exploring new experiences, and taking on new challenges. Two of them attended the University of the Third Age to learn new skills, while another started playing bridge as a new hobby. The remaining two have recently made new friends. They all maintain a playful attitude, a good sense of humor, and aren’t afraid to fail or laugh at themselves.
Prioritize sleep (but not too much): the patients each average seven hours of sleep per night, aligning with research suggesting that 7–9 hours of sleep is ideal for health. They maintain consistent sleep and wake-up times, which contributes to their well-being. While they allow themselves short naps when needed, they avoid long afternoon naps to avoid disrupting their sleep patterns.
Spend time in nature: spending time outdoors is a priority for all five individuals. Whether through walking, gardening, or simply sitting on a park bench, they make it a habit to connect with nature. This aligns with studies showing that time spent in natural environments, especially near water, significantly reduces stress. When water isn’t accessible, green spaces still provide a beneficial boost to mental health.
Stick to a routine: the patients all value simple daily routines, such as enjoying an evening cup of tea, taking a daily walk, or committing to small gardening tasks. These routines offer mental and physical grounding, providing stability even when life becomes difficult sometimes. They emphasized the importance of keeping routines simple and manageable to ensure they could stick to them regardless of life’s challenges.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Top 8 Habits Of The Top 1% Healthiest Over-50s ← another approach to the same question, this time with a larger sample size, and/but many younger (than 90s) respondents.
Take care!
Share This Post
-
Yoga that Helps You on the Loo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How This Video Helps You Poo
When you’re feeling a bit bloated, Yoga With Bird’s 10-minute yoga routine promises to help you release…your gas. And, perhaps, more.
From a tabletop flow to soothing twists, each pose allows you to sync your breath with movement, helping to promote organic relief.
With options to modify with pillows for extra support, this video (below) caters to everyone needing a digestive reset.
Other Toilet Tricks
If yoga isn’t your thing, or you’re interested in trying to use different methods to make your visits to the bathroom a bit easier, we’ve spoken about the ways to manage gut health, and use of probiotics or fiber, and even the prevention of hemorrhoids.
Namaste and goodbye to bloat!
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
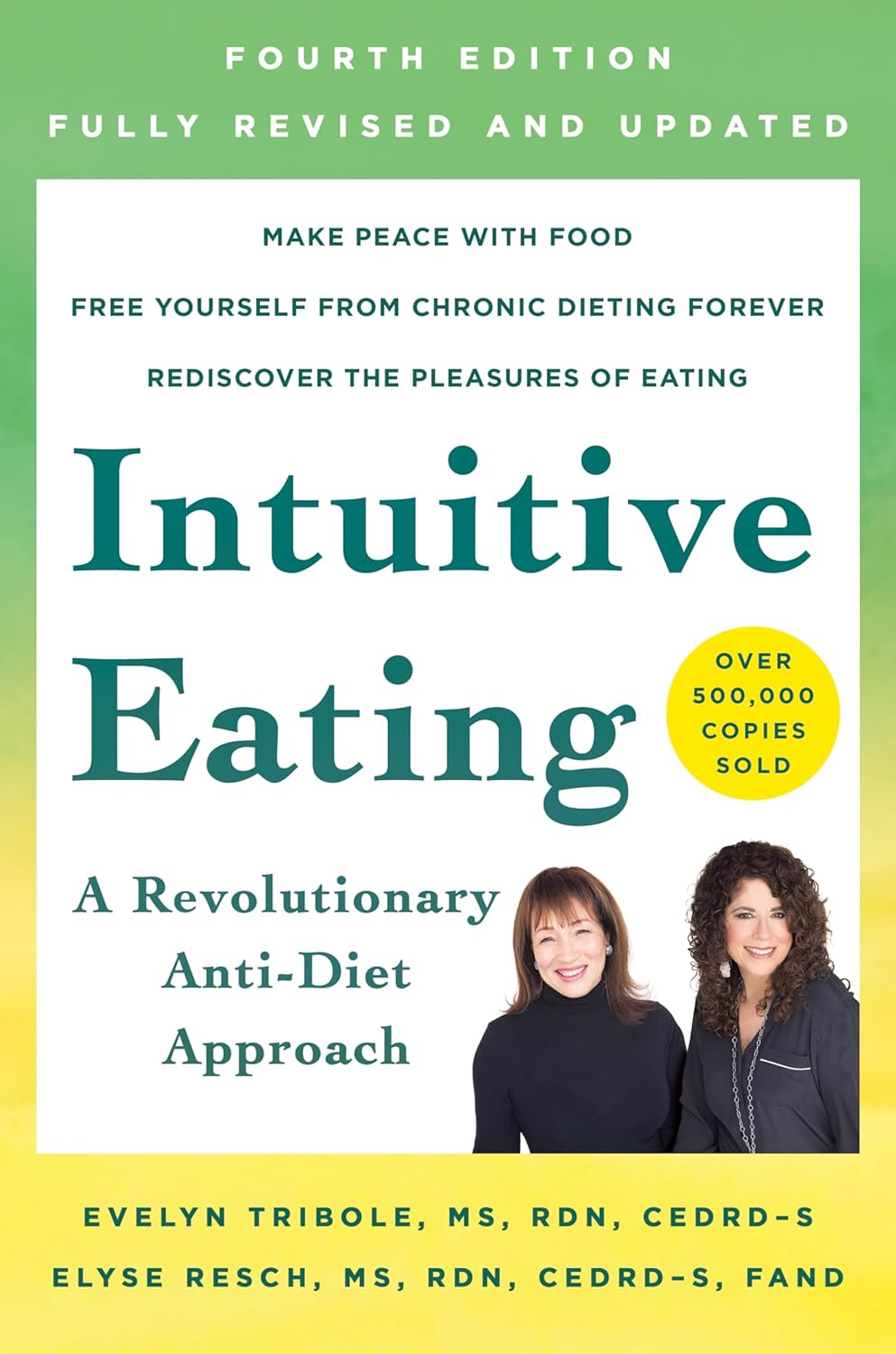
Intuitive Eating – by Evelyn Tribole and Elyse Resch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be given to wonder: if this is about intuitive eating, and an anti-diet approach, why a whole book?
There’s a clue in the other part of the title: “4th Edition”.
The reason there’s a 4th edition (and before it, a 3rd and 2nd edition) is because this book is very much full of science, and science begets more science, and the evidence just keeps on rolling in.
While neither author is a doctor, each has a sizeable portion of the alphabet after their name (more than a lot of doctors), and this is an incredibly well-evidenced book.
The basic premise from many studies is that restrictive dieting does not work well long-term for most people, and instead, better is to make use of our bodies’ own interoceptive feedback.
You see, intuitive eating is not “eat randomly”. We do not call a person “intuitive” because they speak or act randomly, do we? Same with diet.
Instead, the authors give us ten guiding principles (yes, still following the science) to allow us a consistent “finger on the pulse” of what our body has to say about what we have been eating, and what we should be eating.
Bottom line: if you want to be a lot more in tune with your body and thus better able to nourish it the way it needs, this book is literally on the syllabus for many nutritional science classes, and will stand you in very good stead!
Share This Post
Related Posts
-
Burn! How To Boost Your Metabolism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s burn! Metabolic tweaks and hacks
Our metabolism is, for as long as we live, a constantly moving thing. And it’s not a monolith either; there are parts of our metabolism that can speed up or slow down independently of others.
If we talk about metabolism without clarifying context, though, this is usually about one’s “basal metabolic rate”, that is, how many calories we burn just by being alive.
Why do we want to speed it up? Might we ever want to slow it down?
We might want to slow our metabolism down in survival circumstances, but generally speaking, a faster metabolism is a better one.
Yes, even when it comes to aging. Because although metabolism comes with metabolizing oxygen (which, ironically, tends to kill us eventually, since this is a key part of cellular aging), it is still beneficial to replace cells sooner rather than later. The later we replace a given cell (ie, the longer the cell lives), the more damaged it gets, and then the copy is damaged from the start, because the damage was copied along with it. So, best to have a fast metabolism to replace cells quickly when they are young and healthy.
A quick metabolism helps the body to do this.
Most people, of course, are interested in a fast metabolism to burn off fat, but beware: if you increase your metabolism without consideration to how and when you consume calories, you will simply end up eating more to compensate.
One final quick note before we begin:
Limitations
There’s a lot we can do to change our metabolism, but there are some things that may be outside of our control. They include:
- Age—we can influence our biological age, but we cannot (yet!) halt aging, so this will happen
- Body size—and yes we can change this a bit, but we all have our own “basic frame” to work with. Someone who is 6’6” is never going to be able to have the same lower-end-of-scale body mass of someone who is 5’0”, say.
- Sex—this is about hormones, and HRT is a thing, but for example, broadly speaking, men will have faster metabolisms than women, because of hormonal differences.
- Medical conditions—often also related to other hormones, but for example someone with Type 1 Diabetes is going to have a very different relationship with their metabolism than someone without, and someone with a hypo- or hyperactive thyroid will again have a very different metabolism in a way that that lifestyle factors can’t completely compensate for.
The tips and tricks
Intermittent fasting
Intermittent fasting has been found to, amongst other things, promote healthy apoptosis and autophagy (in other words: early programmed cell death and recycling—these are good things).
It also has anti-inflammatory benefits and decreases the risk of insulin resistance. In other words, intermittent fasting boosts the metabolism while simultaneously guarding against some of the dangers of a faster metabolism (harms you’d get if you instead increased your metabolism by doing intense exercise and then eating a mountain of convenience food to compensate)
Read the science: Intermittent Fasting: Is the Wait Worth the Weight?
Read our prior article: Fasting Without Crashing? We Sort The Science From The Hype
Enjoy plenty of protein
This one won’t speed your metabolism up, so much as help it avoid slowing down as a result of fat loss.
Because of our body’s marvelous homeostatic system trying to keep our body from changing status at any given time, often when we lose fat, our body drops our metabolism to compensate, thinking we are in an ongoing survival situation and food is scarce so we’d better conserve energy (as fat). That’s a pain for would-be weight-loss dieters!
Eating protein can let our body know that we’re perfectly safe and not starving, so it will keep the metabolism ticking over nicely, without putting on fat.
Read the science: The role of protein in weight loss and maintenance
Stay hydrated
People think of drinking water as part of a weight loss program being just about filling oneself up, and that is a thing, but it also has a role to play in our metabolism. Specifically, lipolysis (the process of removing fat).
Because, we are mostly water. Not only is it the main content of our various body tissue cells, but also, of particular note, our blood (the means by which everything is transported around our body) is mostly water, too.
It’s hard for the body to keep everything ticking over like a well-oiled machine if its means of transportation is sluggish!
Check it out: Increased Hydration Can Be Associated with Weight Loss
Take a stand
That basal metabolic rate we talked about?
- If you’re lying down at rest, that’s what your metabolism will be like.
- If you’re sitting up, it’ll be a little quicker, but not much.
- If you’re standing, suddenly half your body is doing things, and you don’t even notice them because they’re just stabilizing muscles and the like, but on a cellular level, your body gets very busy.
Read all about it: Cardiometabolic impact of changing sitting, standing, and stepping in the workplace
Time to invest in a standing desk? Or a treadmill in front of the TV?
The spice of life
Capsaicin, the compound in many kinds of pepper that give them their spicy flavor, boosts the metabolism. In the words of Tremblay et al for the International Journal of Obesity:
❝[Capsaicin] stimulates the sympathoadrenal system that mediates the thermogenic and anorexigenic effects of capsaicinoids.
Capsaicinoids have been found to accentuate the impact of caloric restriction on body weight loss.
Some studies have also shown that capsinoids increase energy expenditure.
Capsaicin supplementation attenuates or even prevents the increase in hunger and decrease in fullness as well as the decrease in energy expenditure and fat oxidation, which normally result from energy restriction❞
Read for yourself: Capsaicinoids: a spicy solution to the management of obesity?
You snooze, you lose (fat)
While exercising is generally touted as the road to weight loss, and certainly regular exercise does have a part to play, doing so without good rest will have bad results.
In fact, even if you’re not exercising, if you don’t get enough sleep your metabolism will get sluggish to try to slow you down and encourage you to sleep.
So, be proactive, and make getting enough good quality sleep a priority.
Eat for metabolic health
Aside from the chilli peppers we mentioned, there are other foods associated with good metabolic health. We don’t have room to go into the science of each of them here, but here’s a well-researched, well-sourced standalone article listing some top choices:
The 12 Best Foods to Boost Your Metabolism
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anti-Inflammatory Brownies
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Brownies are usually full of sugar, butter, and flour. These ones aren’t! Instead, they’re full of fiber (good against inflammation), healthy fats, and anti-inflammatory polyphenols:
You will need
- 1 can chickpeas (keep half the chickpea water, also called aquafaba, as we’ll be using it)
- 4 oz of your favorite nut butter (substitute with tahini if you’re allergic to nuts)
- 3 oz rolled oats
- 2 oz dark chocolate chips (or if you want the best quality: dark chocolate, chopped into very small pieces)
- 3 tbsp of your preferred plant milk (this is an anti-inflammatory recipe and unfermented dairy is inflammatory)
- 2 tbsp cocoa powder (pure cacao is best)
- 1 tbsp glycine (if unavailable, use 2 tbsp maple syrup, and skip the aquafaba)
- 2 tsp vanilla extract
- ½ tsp baking powder
- ¼ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃, and line a 7″ cake tin with baking paper.
2) Blend the oats in a food processor, until you have oat flour.
3) Add all the remaining ingredients except the dark chocolate chips, and process until the mixture resembles cookie dough.
3) Transfer to a bowl, and fold in the dark chocolate chips, distributing evenly.
4) Add the mixture to the cake tin, and smooth the surface down so that it’s flat and even. Bake for about 25 minutes, and let them cool in the tin for at least 10 minutes, but longer is better, as they will firm up while they cool. Cut into cubes when ready to serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Cacao vs Carob – Which is Healthier?
- Keep Inflammation At Bay
- The Sweet Truth About Glycine
- The Best Kind Of Fiber For Overall Health?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Four Habits That Drastically Improve Mobility
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mobility is critical for health living, but stretching isn’t the entire story:
Beyond just stretching
Liv Townsend, of LivInLeggings fames, recommends these four habits:
- Sit less: prolonged sitting affects hip and shoulder mobility. Specifically, it affects it negatively. It is also a bringer of woe in many other ways beyond the scope of what we’re doing here today, but the important thing for mobility is to sit less. So, if you spent a lot of time at a desk, invest in a standing desk (writer’s note: I dearly love mine, which is technically a sit-stand converter like this one on Amazon but I just keep it in the up position all the time, so it’s easy to forget it has multiple settings. Anyway, it’s sooooooo much better for my back than sitting for hours at a time.). For how to deal with other (i.e. not desk-related) reasons you might be sitting a lot, check out: Stand Up For Your Health (Or Don’t*)
- Take creatine: more than just for strength and muscle-building (and even aside from its brain-benefits that it bestows to older people, but not young ones), creatine also supports mobility and flexibility. Any brand is fine, so long as creatine monohydrate is the sole ingredient. Also, micronized or not is also fine—that’s just to do with whether it’s been pre-compacted into super-tiny beads (so small that it will still effectively be a powder), which helps it to avoid clumping when mixed in a liquid, that’s all. It shouldn’t have any additives either way (so, check labels to ensure it doesn’t).
- Spend more time under tension: no, we’re not talking about texting your spouse “we need to talk”, but rather, this means that when we do stretch, we should spend longer in the stretched position. While dynamic stretching has its place, passive stretching (holding stretches for longer periods) is essential and shouldn’t be overlooked.
- Incorporate “movement snacks”: this is about when we are going about our daily life, we should move more while doing everyday tasks. Get in some shoulder stretches while waiting for the kettle to boil, deep squat while petting the dog, etc. These are very important, because mobility is very much a “use it or lose it” thing, and so moving in many different ways, frequently, is the only way to ensure full coverage (no stretching regimen is going to be able to cover the many compound movements that we do in everyday life).
*That article also covers how to avoid the damage of sitting even if you cannot physically stand!
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility As Though A Sporting Pursuit: Train For The Event Of Your Life!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: