To Medicate or Not? That is the Question! – by Dr. Asha Bohannon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medications are, of course, a necessity of life (literally!) for many, especially as we get older. Nevertheless, overmedication is also a big problem that can cause a lot of harm too, and guess what, it comes with the exact same “especially as we get older” tag too.
So, what does Dr. Bohannon (a doctor of pharmacy, diabetes educator, and personal trainer too) recommend?
Simply put: she recommends starting with a comprehensive health history assessment and analysing one’s medication/supplement profile, before getting lab work done, tweaking all the things that can be tweaked along the way, and—of course—not neglecting lifestyle medicine either.
The book is prefaced and ended with pep talks that probably a person who has already bought the book does not need, but they don’t detract from the practical content either. Nevertheless, it feels a little odd that it takes until chapter 4 to reach “step 1” of her 7-step method!
The style throughout is conversational and energetic, but not overly padded with hype; it’s just a very casual style. Nevertheless, she brings to bear her professional knowledge and understanding as a doctor of pharmacy, to include her insights into the industry that one might not observe from outside of it.
Bottom line: if you’d like to do your own personal meds review and want to “know enough to ask the right questions” before bringing it up with your doctor, this book is a fine choice for that.
Click here to check out To Medicate Or Not, and make informed choices!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
4 Practices To Build Self-Worth That Lasts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Self-worth is internal, based on who you are, not what you do or external validation. It differs from self-esteem, which is more performance-based. High self-worth doesn’t necessarily mean arrogance, but can lead to more confidence and success. Most importantly, it’ll help you to thrive in what’s actually most important to you, rather than being swept along by what other people want.
A stable foundation
A strong sense of self-worth shapes how you handle boundaries, what you believe you deserve, and what you pursue in life. This matters, because life is unpredictable, so having a resilient internal foundation (like a secure “house”) helps you to weather challenges.
- Self-acceptance and compassion:
- Accept both your positive and negative traits with compassion.
- Don’t judge yourself harshly; allow yourself to accept imperfections without guilt or shame.
- Self-trust:
- Trust yourself to make choices that benefit you and create habits that support long-term well-being—especially if those benefits are cumulative!
- Balance self-care with flexibility to enjoy life without being overly rigid.
- Get uncomfortable:
- Growth happens outside your comfort zone. Step into new, challenging experiences to build self-trust.
- However! Small uncomfortable actions lead to greater confidence and a stronger sense of self. Large uncomfortable actions often doing lead anywhere good.
- Separation of tasks:
- Oftentimes we end up overly preoccupying ourselves with things that are not actually our responsibility. Focus instead on tasks that genuinely belong to you, and let go of trying to control others’ perceptions or tasks.
- Seek internal validation, not external praise. Avoid people-pleasing behavior.
Finally, three things to keep in mind:
- Boundaries: respecting your own boundaries strengthens self-worth, avoiding burnout from people-pleasing.
- Validation: self-worth is independent of how others perceive you; focus on your integrity and personal growth.
- Accountability: take responsibility for your actions but recognize that others’ reactions are beyond your control.
For more on all of these things, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Practise Self-Compassion In Your Relationship (But Watch Out!)
Take care!
Share This Post
- Self-acceptance and compassion:
-
Mouthwatering Protein Falafel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Baking falafel, rather than frying it, has a strength and a weakness. The strength: it is less effort and you can do more at once. The weakness: it can easily get dry. This recipe calls for baking them in a way that won’t get dry, and the secret is one of its protein ingredients: peas! Add to this the spices and a tahini sauce, and you’ve a mouthwatering feast that’s full of protein, fiber, polyphenols, and even healthy fats.
You will need
- 1 cup peas, cooked
- 1 can chickpeas, drained and rinsed (keep the chickpea water—also called aquafaba—aside, as we’ll be using some of it later)
- ½ small red onion, chopped
- 1 handful fresh mint, chopped
- 1 tbsp fresh parsley, chopped
- ½ bulb garlic, crushed
- 1 tbsp lemon juice
- 1 tbsp chickpea flour (also called gram flour, besan flour, or garbanzo bean flour) plus more for dusting
- 2 tsp red chili flakes (adjust per heat preferences)
- 2 tsp black pepper, coarse ground
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
For the tahini sauce:
- 2 tbsp tahini
- 2 tbsp lemon juice
- ¼ bulb garlic, crushed
- 5 tbsp aquafaba (if for some reason you don’t have it, such as for example you substituted 1 cup chickpeas that you cooked yourself, substitute with water here)
To serve:
- Flatbreads (you can use our Healthy Homemade Flatbreads recipe if you like)
- Leafy salad
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Blend the peas and chickpeas in a food processor for a few seconds. You want a coarse mixture, not a paste.
3) Add the rest of the main section ingredients except the olive oil, and blend again for a few more seconds. It should still have a chunky texture, or else you will have made hummus. If you accidentally make hummus, set your hummus aside and start again on the falafels.
4) Shape the mixture into balls; if it lacks structural integrity, fold in a little more chickpea flour until the balls stay in shape. Either way, once you have done that, dust the balls in chickpea flour.
5) Brush the balls in a little olive oil, as you put them on a baking tray lined with baking paper. Bake for 15–18 minutes until golden, turning partway through.
6) While you are waiting, making the tahini sauce by combining the tahini sauce ingredients in a high-speed blender and processing on high until smooth. If you do not have a small enough blender (a bullet-style blender should work for this), then do it manually, which means you’ll have to crush the garlic all the way into a smooth paste, such as with a pestle and mortar, or alternatively, use ready-made garlic paste—and then simply whisk the ingredients together until smooth.
7) Serve the falafels warm or cold, on flatbreads with leafy salad and the tahini sauce.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tahini vs Hummus – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored 4/5 today!
Take care!
Share This Post
-
Does intermittent fasting increase or decrease our risk of cancer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Research over the years has suggested intermittent fasting has the potential to improve our health and reduce the likelihood of developing cancer.
So what should we make of a new study in mice suggesting fasting increases the risk of cancer?
Stock-Asso/Shutterstock What is intermittent fasting?
Intermittent fasting means switching between times of eating and not eating. Unlike traditional diets that focus on what to eat, this approach focuses on when to eat.
There are lots of commonly used intermittent fasting schedules. The 16/8 plan means you only eat within an eight-hour window, then fast for the remaining 16 hours. Another popular option is the 5:2 diet, where you eat normally for five days then restrict calories for two days.
In Australia, poor diet contributes to 7% of all cases of disease, including coronary heart disease, stroke, type 2 diabetes, and cancers of the bowel and lung. Globally, poor diet is linked to 22% of deaths in adults over the age of 25.
Intermittent fasting has gained a lot of attention in recent years for its potential health benefits. Fasting influences metabolism, which is how your body processes food and energy. It can affect how the body absorbs nutrients from food and burns energy from sugar and fat.
What did the new study find?
The new study, published in Nature, found when mice ate again after fasting, their gut stem cells, which help repair the intestine, became more active. The stem cells were better at regenerating compared with those of mice who were either totally fasting or eating normally.
This suggests the body might be better at healing itself when eating after fasting.
However, this could also have a downside. If there are genetic mutations present, the burst of stem cell-driven regeneration after eating again might make it easier for cancer to develop.
Polyamines – small molecules important for cell growth – drive this regeneration after refeeding. These polyamines can be produced by the body, influenced by diet, or come from gut bacteria.
The findings suggest that while fasting and refeeding can improve stem cell function and regeneration, there might be a tradeoff with an increased risk of cancer, especially if fasting and refeeding cycles are repeated over time.
While this has been shown in mice, the link between intermittent fasting and cancer risk in humans is more complicated and not yet fully understood.
What has other research found?
Studies in animals have found intermittent fasting can help with weight loss, improve blood pressure and blood sugar levels, and subsequently reduce the risks of diabetes and heart disease.
Research in humans suggests intermittent fasting can reduce body weight, improve metabolic health, reduce inflammation, and enhance cellular repair processes, which remove damaged cells that could potentially turn cancerous.
However, other studies warn that the benefits of intermittent fasting are the same as what can be achieved through calorie restriction, and that there isn’t enough evidence to confirm it reduces cancer risk in humans.
What about in people with cancer?
In studies of people who have cancer, fasting has been reported to protect against the side effects of chemotherapy and improve the effectiveness of cancer treatments, while decreasing damage to healthy cells.
Prolonged fasting in some patients who have cancer has been shown to be safe and may potentially be able to decrease tumour growth.
On the other hand, some experts advise caution. Studies in mice show intermittent fasting could weaken the immune system and make the body less able to fight infection, potentially leading to worse health outcomes in people who are unwell. However, there is currently no evidence that fasting increases the risk of bacterial infections in humans.
So is it OK to try intermittent fasting?
The current view on intermittent fasting is that it can be beneficial, but experts agree more research is needed. Short-term benefits such as weight loss and better overall health are well supported. But we don’t fully understand the long-term effects, especially when it comes to cancer risk and other immune-related issues.
Since there are many different methods of intermittent fasting and people react to them differently, it’s hard to give advice that works for everyone. And because most people who participated in the studies were overweight, or had diabetes or other health problems, we don’t know how the results apply to the broader population.
For healthy people, intermittent fasting is generally considered safe. But it’s not suitable for everyone, particularly those with certain medical conditions, pregnant or breastfeeding women, and people with a history of eating disorders. So consult your health-care provider before starting any fasting program.
Amali Cooray, PhD Candidate in Genetic Engineering and Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
As The Summer Gets Hotter Still…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I would love to see an article about heat dehydrated illness….so much of the US is under hot conditions. I had an fainting sweating episode and now trying to recoup from it. What should we do? Drink water,rest…???❞
We have done some of this, but it’s always a good one to revisit! Last summer (N. Hemisphere summer), we wrote this:
Stay Safe From Heat Exhaustion & Heatstroke!
…and this year, it’s getting hotter still (and is already the hottest summer on record), with certainly much of the US seriously affected, as you say. Next year, it will probably be worse again; climate change is getting predictable like that, and likely will continue until fixed. We are but a health science publication, so we can’t fix the world’s climate, but we can reiterate the above advice, and urge everyone to take it seriously.
Note: heat exhaustion and heatstroke kill. Yes, we’re including heat exhaustion in that, because by the time you get heat exhaustion, you’re often not in the best state of mind to take the correct steps to avoid the heatstroke that follows.
To think otherwise would be akin to thinking “falling never killed anyone; it’s only when you stop falling that it’s dangerous”.
This summer, we did also write this more niche article:
…whose advice won’t apply to everyone, but will be helpful to some, and honestly, some of that advice does go for everyone.
One thing we didn’t write about in those articles that we’ll add here:
Humidity is dangerous:
- Dry heat: you sweat, the sweat evaporates, cooling you. As well as losing heat, you’ve also now lost water and salts, which you’ll need to replenish, but your body is operating correctly.
- Humid heat: you sweat, and now you are just sweaty until further notice. It doesn’t evaporate because the surrounding humidity doesn’t provide the physics for that. Not only are you not losing heat through evaporating sweat, but also, if you’re wearing clothes, that’s now an insulating layer you’re wearing.
…so that means, watch the humidity as carefully as you watch the temperature, and when it’s high, get extra serious about finding ways to keep yourself cool (e.g. shade, rest, cooling showers etc if you can, that kind of thing).
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Does One Test Acupuncture Against Placebo Anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pinpointing The Usefulness Of Acupuncture
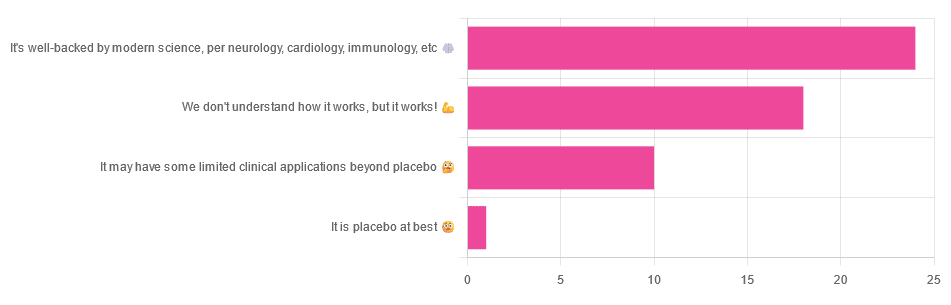
We asked you for your opinions on acupuncture, and got the above-depicted, below-described, set of answers:
- A little under half of all respondents voted for “It’s well-backed by modern science, per neurology, cardiology, immunology, etc”
- Slightly fewer respondents voted for “We don’t understand how it works, but it works!”
- A little under a fifth of respondents voted for “It may have some limited clinical applications beyond placebo”
- One (1) respondent voted for for “It’s placebo at best”
When we did a main feature about homeopathy, a couple of subscribers wrote to say that they were confused as to what homeopathy was, so this time, we’ll start with a quick definition first.
First, what is acupuncture? For the convenience of a quick definition so that we can move on to the science, let’s borrow from Wikipedia:
❝Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine in which thin needles are inserted into the body.
Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientific knowledge, and it has been characterized as quackery.❞
Now, that’s not a promising start, but we will not be deterred! We will instead examine the science itself, rather than relying on tertiary sources like Wikipedia.
It’s worth noting before we move on, however, that there is vigorous debate behind the scenes of that article. The gist of the argument is:
- On one side: “Acupuncture is not pseudoscience/quackery! This has long been disproved and there are peer-reviewed research papers on the subject.”
- On the other: “Yes, but only in disreputable quack journals created specifically for that purpose”
The latter counterclaim is a) potentially a “no true Scotsman” rhetorical ploy b) potentially true regardless
Some counterclaims exhibit specific sinophobia, per “if the source is Chinese, don’t believe it”. That’s not helpful either.
Well, the waters sure are muddy. Where to begin? Let’s start with a relatively easy one:
It may have some clinical applications beyond placebo: True or False?
True! Admittedly, “may” is doing some of the heavy lifting here, but we’ll take what we can get to get us going.
One of the least controversial uses of acupuncture is to alleviate chronic pain. Dr. Vickers et al, in a study published under the auspices of JAMA (a very respectable journal, and based in the US, not China), found:
❝Acupuncture is effective for the treatment of chronic pain and is therefore a reasonable referral option. Significant differences between true and sham acupuncture indicate that acupuncture is more than a placebo.
However, these differences are relatively modest, suggesting that factors in addition to the specific effects of needling are important contributors to the therapeutic effects of acupuncture❞
Source: Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis
If you’re feeling sharp today, you may be wondering how the differences are described as “significant” and “relatively modest” in the same text. That’s because these words have different meanings in academic literature:
- Significant = p<0.05, where p is the probability of the achieved results occurring randomly
- Modest = the differences between the test group and the control group were small
In other words, “significant modest differences” means “the sample sizes were large, and the test group reliably got slightly better results than placebo”
We don’t understand how it works, but it works: True or False
Broadly False. When it works, we generally have an idea how.
Placebo is, of course, the main explanation. And even in examples such as the above, how is placebo acupuncture given?
By inserting acupuncture needles off-target rather than in accord with established meridians and points (the lines and dots that, per Traditional Chinese Medicine, indicate the flow of qi, our body’s vital energy, and welling-points of such).
So, if a patient feels that needles are being inserted randomly, they may no longer have the same confidence that they aren’t in the control group receiving placebo, which could explain the “modest” difference, without there being anything “to” acupuncture beyond placebo. After all, placebo works less well if you believe you are only receiving placebo!
Indeed, a (Korean, for the record) group of researchers wrote about this—and how this confounding factor cuts both ways:
❝Given the current research evidence that sham acupuncture can exert not only the originally expected non-specific effects but also sham acupuncture-specific effects, it would be misleading to simply regard sham acupuncture as the same as placebo.
Therefore, researchers should be cautious when using the term sham acupuncture in clinical investigations.❞
Source: Sham Acupuncture Is Not Just a Placebo
It’s well-backed by modern science, per neurology, cardiology, immunology, etc: True or False?
False, for the most part.
While yes, the meridians and points of acupuncture charts broadly correspond to nerves and vasculature, there is no evidence that inserting needles into those points does anything for one’s qi, itself a concept that has not made it into Western science—as a unified concept, anyway…
Note that our bodies are indeed full of energy. Electrical energy in our nerves, chemical energy in every living cell, kinetic energy in all our moving parts. Even, to stretch the point a bit, gravitational potential energy based on our mass.
All of these things could broadly be described as qi, if we so wish. Indeed, the ki in the Japanese martial art of aikido is the latter kinds; kinetic energy and gravitational potential energy based on our mass. Same goes, therefore for the ki in kiatsu, a kind of Japanese massage, while the ki in reiki, a Japanese spiritual healing practice, is rather more mystical.
The qi in Chinese qigong is mostly about oxygen, thus indirectly chemical energy, and the electrical energy of the nerves that are receiving oxygenated blood at higher or lower levels.
On the other hand, the efficacy of the use of acupuncture for various kinds of pain is well-enough evidenced. Indeed, even the UK’s famously thrifty NHS (that certainly would not spend money on something it did not find to work) offers it as a complementary therapy for some kinds of pain:
❝Western medical acupuncture (dry needling) is the use of acupuncture following a medical diagnosis. It involves stimulating sensory nerves under the skin and in the muscles.
This results in the body producing natural substances, such as pain-relieving endorphins. It’s likely that these naturally released substances are responsible for the beneficial effects experienced with acupuncture.❞
Source: NHS | Acupuncture
Meanwhile, the NIH’s National Cancer Institute recommends it… But not as a cancer treatment.
Rather, they recommend it as a complementary therapy for pain management, and also against nausea, for which there is also evidence that it can help.
Frustratingly, while they mention that there is lots of evidence for this, they don’t actually link the studies they’re citing, or give enough information to find them. Instead, they say things like “seven randomized clinical trials found that…” and provide links that look reassuring until one finds, upon clicking on them, that it’s just a link to the definition of “randomized clinical trial”:
Source: NIH | Nactional Cancer Institute | Acupuncture (PDQ®)–Patient Version
However, doing our own searches finds many studies (mostly in specialized, potentially biased, journals such as the Journal of Acupuncture and Meridian Studies) finding significant modest outperformance of [what passes for] placebo.
Sometimes, the existence of papers with promising titles, and statements of how acupuncture might work for things other than relief of pain and nausea, hides the fact that the papers themselves do not, in fact, contain any evidence to support the hypothesis. Here’s an example:
❝The underlying mechanisms behind the benefits of acupuncture may be linked with the regulation of the hypothalamic-pituitary-gonadal (adrenal) axis and activation of the Wnt/β-catenin and OPG/RANKL/RANK signaling pathways.
In summary, strong evidence may still come from prospective and well-designed clinical trials to shed light on the potential role of acupuncture in preserving bone loss❞
Source: Acupuncture for Osteoporosis: a Review of Its Clinical and Preclinical Studies
So, here they offered a very sciencey hypothesis, and to support that hypothesis, “strong evidence may still come”.
“We must keep faith” is not usually considered evidence worthy of inclusion in a paper!
PS: the above link is just to the abstract, because the “Full Text” link offered in that abstract leads to a completely unrelated article about HIV/AIDS-related cryptococcosis, in a completely different journal, nothing to do with acupuncture or osteoporosis).
Again, this is not the kind of professionalism we expect from peer-reviewed academic journals.
Bottom line:
Acupuncture reliably performs slightly better than sham acupuncture for the management of pain, and may also help against nausea.
Beyond placebo and the stimulation of endorphin release, there is no consistently reliable evidence that is has any other discernible medical effect by any mechanism known to Western science—though there are plenty of hypotheses.
That said, absence of evidence is not evidence of absence, and the logistical difficulty of testing acupuncture against placebo makes for slow research. Maybe one day we’ll know more.
For now:
- If you find it helps you: great! Enjoy
- If you think it might help you: try it! By a licensed professional with a good reputation, please.
- If you are not inclined to having needles put in you unnecessarily: skip it! Extant science suggests that at worst, you’ll be missing out on slight relief of pain/nausea.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ice Cream vs Fruit Sorbet – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing ice cream to fruit sorbet, we picked the ice cream.
Why?
Well, neither are great!
But the deciding factor is simple: ice cream has more nutrients to go with its sugar.
While “fruit is good” is a very reliable truism in and of itself, sorbet tends to be made with fruit juice (or at best, purée, which for these purposes is more or less the same) and sugar. The small vitamin content is nowhere near enough to make up for this. The fiber having been removed by juicing or puréeing, the fruit juice with added sugar is basically shooting glucose and fructose into your veins while doing little else.
Fruit juice (even freshly-pressed) is nowhere near in the same league of healthiness as actual fruit!
See also: Which Sugars Are Healthier, And Which Are Just The Same?
Ice cream, meanwhile, is also not exactly a health food. But it has at least some minerals worth speaking of (mostly: calcium, potassium, phosphorus), and some fat that a) can be used b) helps slightly slow the absorption of the sugars.
In short: please do not consider either of these things to be a health food. But if you’re going to choose one or the other (and are not lactose-intolerant), then ice cream has some small positives to go with its negatives.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: