Potatoes & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝My other half considers potatoes a wonder food, except when fried. I don’t. I find, when I am eating potatoes I put on weight; and, when I’m not eating them, I lose it. Also, although I can’t swear to it, potatoes also make me feel a little anxious (someone once told me it could have something to do with where they are on the “glycemic index”). What does the science say?❞
The glycemic index of potatoes depends on the kind of potato (obviously) and also, less obviously, how it’s prepared. For a given white potato, boiling (which removes a lot of starch) might produce a GI of around 60, while instant mash (basically: potato starch) can be more like 80. For reference, pure glucose is 100. And you probably wouldn’t take that in the same quantity you’d take potato, and expect to feel good!
So: as for anxiety, it could be, since spiked blood sugars can cause mood swings, including anxiety.
Outside of the matter of blood sugars, the only reference we could find for potatoes causing anxiety was fried potatoes specifically:
❝frequent fried food consumption, especially fried potato consumption, is strongly associated with 12% and 7% higher risk of anxiety and depression, respectively❞
…which heavily puts the blame not on the potatoes themselves, but on acrylamide (the orange/brown stuff that is made by the Maillard reaction of cooking starches in the absence of water, e.g. by frying, roasting, etc).
Here’s a very good overview of that, by the way:
A Review on Acrylamide in Food: Occurrence, Toxicity, and Mitigation Strategies
Back on the core topic of potatoes and GI and blood sugar spikes and anxiety, you might benefit from a few tweaks that will allow you to enjoy potatoes without spiking blood sugars:
10 Ways To Balance Blood Sugars
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ageless Athletes – by Dr. Jim Madden
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an approach to strength and fitness training specifically for the 50+ crowd, and/but even more specifically for the 50+ crowd who do not wish to settle for mediocrity. In short, it’s for those who not only wish to stay healthy and have good mobility, but also who wish to be and remain athletic.
It does not assume extant athleticism, but nor does it assume complete inexperience. It provides a fairly ground-upwards entry to a training program that then quickly proceeds to competitive levels of athleticism.
The author himself details his own journey from being in his 30s, overweight and unfit, to being in his 50s and very athletic, with before and after photos. Granted, those are 20 years in between, but all the same, it’s a good sign when someone gets stronger and fitter with age, rather than declining.
The style of the book is quite casual, and/but after the introductory background and pep talk, is quite pragmatic and drops the additional fluff. In particular, older readers may enjoy the “Old Workhorse” protocol, as a tailored measured progression system.
In terms of expected equipment by the way, some is bodyweight and some is with weights; kettlebells in particular feature strongly, since this is about functional strength and not bodybuilding.
In the category of criticism, he does refer to his other books and generally assumes the reader is reading all his work, so it may not be for everyone as a standalone book.
Bottom line: if you’re 50+ and are wondering how to gain/maintain a high level athleticism, this book can definitely help with that.
Click here to check out Ageless Athlete, and go from strength to strength!
Share This Post
-
Coconut vs Avocado – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing coconut to avocado, we picked the avocado.
Why?
In terms of macros, avocado is lower in carbs and also in net carbs—coconut’s a little higher in fiber, but not enough to make up for the difference in carbs nor, when it comes to glycemic index and insulin index, the impact of coconut’s much higher fat content on insulin responses too. On which note, while coconut’s fats are broadly considered healthy (its impressive saturated fat content is formed of medium-chain triglycerides which, in moderation, are heart-healthy), avocado’s fats are even healthier, being mostly monounsaturated fat with some polyunsaturated (and about 15x less saturated fat). All in all, a fair win for avocado on the macros front, but coconut isn’t bad in moderation.
When it comes to vitamins, avocados are higher in vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline. Most of those differences are by very large margins. Coconuts are not higher in any vitamins. A huge, easy, “perfect score” win for avocados.
In the category of minerals, however, it’s coconut’s turn to sweep with more calcium, copper, iron, magnesium, manganese, phosphorus, zinc, and selenium—though the margins are mostly not nearly as impressive as avocado’s vitamin margins. Speaking of avocados, they do have more potassium than coconuts do, but the margin isn’t very large. A compelling win for coconut’s mineral content.
Adding up the sections, we get to a very credible win for avocados, but coconuts are also very respectable. So, as ever, enjoy both (although we do recommend exercising moderation in the case of coconuts, mainly because of the saturated fat content), and if you’re choosing between them for some purpose, then avocado will generally be the best option.
Want to learn more?
You might like to read:
- Can Saturated Fats Be Healthy? ← defying Betteridge’s Law here!
- Avocado, Coconut & Lime Crumble Pots ← if you do want to enjoy both, here’s a fabulous way to do so in style
Take care!
Share This Post
-
Ketogenic Diet: Burning Fat Or Burning Out?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
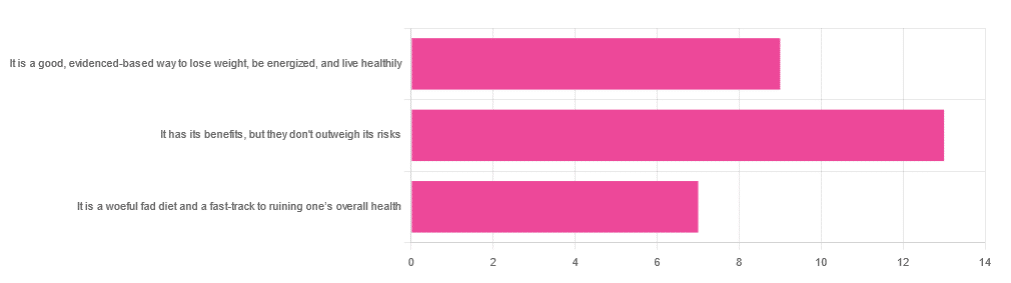
In Wednesday’s newsletter, we asked you for your opinion of the keto diet, and got the above-depicted, below-described set of responses:
- About 45% said “It has its benefits, but they don’t outweigh the risks”
- About 31% said “It is a good, evidence-based way to lose weight, be energized, and live healthily”
- About 24% said “It is a woeful fad diet and a fast-track to ruining one’s overall health”
So what does the science say?
First, what is the ketogenic diet?
There are two different stories here:
- Per science, it’s a medical diet designed to help treat refractory epilepsy in children.
- Per popular lore, it’s an energizing weight loss diet for Instagrammers and YouTubers.
Can it be both? The answer is: yes, but with some serious caveats, which we’ll cover over the course of today’s feature.
The ketogenic diet works by forcing the body to burn fat for energy: True or False?
True! This is why it helps for children with refractory epilepsy. By starving the body (including the brain) of glucose, the liver must convert fat into fatty acids and ketones, which latter the brain (and indeed the rest of the body) can now use for energy instead of glucose, thus avoiding one of the the main triggers of refractory epilepsy in children.
See: The Ketogenic Diet: One Decade Later | Pediatrics
Even the pediatric epilepsy studies, however, conclude it does have unwanted side effects, such as kidney stones, constipation, high cholesterol, and acidosis:
Source: Dietary Therapies for Epilepsy
The ketogenic diet is good for weight loss: True or False?
True! Insofar as it does cause weight loss, often rapidly. Of course, so do diarrhea and vomiting, but these are not usually held to be healthy methods of weight loss. As for keto, a team of researchers recently concluded:
❝As obesity rates in the populace keep rising, dietary fads such as the ketogenic diet are gaining traction.
Although they could help with weight loss, this study had a notable observation of severe hypercholesterolemia and increased risk of atherosclerotic cardiovascular disease among the ketogenic diet participants.❞
~ Dr. Shadan Khdher et al.
On which note…
The ketogenic diet is bad for the heart: True or False?
True! As Dr. Joanna Popiolek-Kalisz concluded recently:
❝In terms of cardiovascular mortality, the low-carb pattern is more beneficial than very low-carbohydrate (including the ketogenic diet). There is still scarce evidence comparing ketogenic to the Mediterranean diet.
Other safety concerns in cardiovascular patients such as adverse events related to ketosis, fat-free mass loss, or potential pharmacological interactions should be also taken into consideration in future research.❞
~ Dr. Joanna Popiolek-Kalisz
Read in full: Ketogenic diet and cardiovascular risk: state of the art review
The ketogenic diet is good for short-term weight loss, but not long-term maintenance: True or False?
True! Again, insofar as it works in the short term. It’s not the healthiest way to lose weight and we don’t recommend it, but it did does indeed precipitate short-term weight loss. Those benefits are not typically observed for longer than a short time, though, as the above-linked paper mentions:
❝The ketogenic diet does not fulfill the criteria of a healthy diet. It presents the potential for rapid short-term reduction of body mass, triglycerides level, Hb1Ac, and blood pressure.
Its efficacy for weight loss and the above-mentioned metabolic changes is not significant in long-term observations.❞
~ Ibid.
The ketogenic diet is a good, evidence-based way to lose weight, be energized, and live healthily: True or False?
False, simply, as you may have gathered from the above, but we’ve barely scratched the surface in terms of the risks.
That said, as mentioned, it will induce short-term weight loss, and as for being energized, typically there is a slump-spike-slump in energy:
- At first, the body is running out of glucose, and so naturally feels weak and tired.
- Next, the body enters ketosis, and so feels energized and enlivened ← this is the part where the popular enthusiastic reviews come from
- Then, the body starts experiencing all the longer-term problems associated with lacking carbohydrates and having an overabundance of fat, so becomes gradually more sick and tired.
Because of this, the signs of symptoms of being in ketosis (aside from: measurably increased ketones in blood, breath, and urine) are listed as:
- Bad breath
- Weight loss
- Appetite loss
- Increased focus and energy
- Increased fatigue and irritability
- Digestive issues
- Insomnia
The slump-spike-slump we mentioned is the reason for the seemingly contradictory symptoms of increased energy and increased fatigue—you get one and then the other.
Here’s a small but illustrative study, made clearer by its participants being a demographic whose energy levels are most strongly affected by dietary factors:
The ketogenic diet is a woeful fad diet and a fast-track to ruining one’s overall health: True or False?
True, subjectively in the first part, as it’s a little harsher than we usually go for in tone, though it has been called a fad diet in scientific literature. The latter part (ruining one’s overall health) is observably true.
One major problem is incidental-but-serious, which is that a low-carb diet is typically a de facto low-fiber diet, which is naturally bad for the gut and heart.
Other things are more specific to the keto diet, such as the problems with the kidneys:
However, kidney stones aren’t the worst of the problems:
Is Losing Weight Worth Losing Your Kidney: Keto Diet Resulting in Renal Failure
We’re running out of space and the risks associated with the keto diet are many, but for example even in the short term, it already increases osteoporosis risk:
❝Markers of bone modeling/remodeling were impaired after short-term low-carbohydrate high-fat diet, and only one marker of resorption recovered after acute carbohydrate restoration❞
~ Dr. Ida Heikura et al.
A Short-Term Ketogenic Diet Impairs Markers of Bone Health in Response to Exercise
Want a healthier diet?
We recommend the Mediterranean diet.
See also: Four Ways To Upgrade The Mediterranean
(the above is about keeping to the Mediterranean diet, while tweaking one’s choices within it for a specific extra health focus such as an anti-inflammatory upgrade, a heart-healthy upgrade, a gut-healthy upgrade, and a brain-healthy upgrade)
Enjoy!
Share This Post
Related Posts
-
5 Self-Care Trends That Are Actually Ruining Your Mental Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ok, some of these are trends; some are more perennial to human nature. For example, while asceticism is not a new idea, the “dopamine detox” is, and “bed rotting” is not a trend that this writer has seen recommended anywhere, but on the other hand, there are medieval illustrations of it—there was no Netflix in sight in the medieval illustrations, but perhaps a label diagnosing it as “melancholy”, for example.
So without further ado, here are five things to not do…
Don’t fall into these traps
The 5 things to watch out for are:
- Toxic positivity: constantly promoting positivity regardless of the reality of a situation can shame or invalidate genuine emotions, preventing people from processing their real feelings and leading to negative mental health outcomes—especially if it involves a “head in sand” approach to external problems as well as internal ones (because then those problems will never actually get dealt with).
- Self-indulgence: excessive focus on personal desires can make you more self-centered, less disciplined, and ultimately dissatisfied, which hinders personal growth and mental wellness.
- Bed rotting: spending prolonged time in bed for relaxation or entertainment can decrease motivation, productivity, and lead to (or worsen) depression rather than promoting genuine rest and rejuvenation.
- Dopamine detox: abstaining from pleasurable activities to “reset” the brain simply does not work and can lead to loneliness, boredom, and worsen mental health, especially when done excessively.
- Over-reliance on self-help: consuming too much self-help content or relying on material possessions for well-being can lead to information overload, unrealistic expectations, and the constant need for self-fixing, rather than fostering self-acceptance and authentic growth. Useful self-help can be like taking your car in for maintenance—counterproductive self-help is more like having your car always in for maintenance and never actually on the road.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read, and yes these are pretty much one-for-one with the 5 items above, doing a deeper dive into each in turn,
- How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
- Self-Care That’s Not Just Self-Indulgence
- The Mental Health First-Aid That You’ll Hopefully Never Need
- The Dopamine Myth
- Behavioral Activation Against Depression & Anxiety
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Weight Vests Against Osteoporosis: Do They Really Build Bone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Doug Lucas is a dual board-certified physician specializing in optimizing healthspan and bone health for women experiencing osteoporosis, perimenopause, and menopause. Here, he talks weight vests:
Worth the weight?
Dr. Lucas cites “Wolf’s Law”—bones respond to stress. A weighted vest adds stress, to help build bone density. That said, they may not be suitable for everyone (for example, in cases of severe osteoporosis or a recent vertebral fracture).
He also cites some studies:
- Erlanger Fitness Study (2004): participants with a weighted vest maintained or improved bone density compared to a control group, but there was no group with exercise alone, making it unclear if the vest itself had the biggest impact.
- Newer studies (2016, 2017): showed improved outcomes for groups wearing a weighted vest, but again lacked an exercise-only group for comparison.
- 2012 study: included three groups (control, weighted vest, exercise only). Results showed no significant bone density difference between vest and exercise-only groups, though the vest group showed better balance and motor control.
Dr. Lucas concludes that weighted vests are a useful tool while nevertheless not being a magic bullet for bone health. In other words, they can complement exercise but you will also be fine without. If you do choose to level-up your exercise by using a weight vest, then starting with 5–10% of body weight in a vest is often recommended, but it depends on individual circumstances. If in doubt, start low and build up. Wearing the vest for daily activities can be effective, but improper use (awkward positions or improper impact training) can increase injury risk, so do be careful with that.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Osteoporosis & Exercises: Which To Do (And Which To Avoid)
- One More Resource Against Osteoporosis!
- The Osteoporosis Breakthrough – by Dr. Doug Lucas ← we reviewed his book a while back!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Olive oil is healthy. Turns out olive leaf extract may be good for us too
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Olive oil is synonymous with the Mediterranean diet, and the health benefits of both are well documented.
Olive oil reduces the risk of heart disease, cancer, diabetes and premature death. Olives also contain numerous healthy nutrients.
Now evidence is mounting about the health benefits of olive leaves, including from studies in a recent review.
Here’s what’s in olive leaves and who might benefit from taking olive leaf extract.
mtphoto19/Shutterstock What’s in olive leaves?
Olive leaves have traditionally been brewed as a tea in the Mediterranean and drunk to treat fever and malaria.
The leaves contain high levels of a type of antioxidant called oleuropein. Olives and olive oil contain this too, but at lower levels.
Generally, the greener the leaf (the less yellowish) the more oleuropein it contains. Leaves picked in spring also have higher levels compared to ones picked in autumn, indicating levels of oleuropein reduce as the leaves get older.
Olive leaves also contain other antioxidants such as hydroxytyrosol, luteolin, apigenin and verbascoside.
Antioxidants work by reducing the oxidative stress in the body. Oxidative stress causes damage to our DNA, cell membranes and tissues, which can lead to chronic diseases such as cancer and heart disease.
Are olive leaves healthy?
One review and analysis combined data from 12 experimental studies with 819 participants in total. Overall, olive leaf extract improved risk factors for heart disease. This included healthier blood lipids (fats) and lowering blood pressure.
The effect was greater for people who already had high blood pressure.
Most studies in this review gave olive leaf extract as a capsule, with daily doses of 500 milligrams to 5 grams for six to 48 weeks.
Another review and analysis published late last year looked at data from 12 experimental studies, with a total of 703 people. Some of these studies involved people with high blood lipids, people with high blood pressure, people who were overweight or obese, and some involved healthy people.
Daily doses were 250-1,000mg taken as tablets or baked into bread.
Individual studies in the review showed significant benefits in improving blood glucose (sugar) control, blood lipid levels and reducing blood pressure. But when all the data was combined, there were no significant health effects. We’ll explain why this may be the case shortly.
Olive leaves can be brewed into tea. Picture Partners/Shutterstock Another review looked at people who took oleuropein and hydroxytyrosol (the antioxidants in olive leaves). This found significant improvement in body weight, blood lipid profiles, glucose metabolism and improvements in bones, joints and cognitive function.
The individual studies included tested either the two antioxidants or olive leaf incorporated into foods such as bread and cooking oils (but not olive oil). The doses were 6-500mg per day of olive leaf extract.
So what can we make of these studies overall? They show olive leaf extract may help reduce blood pressure, improve blood lipids and help our bodies handle glucose.
But these studies show inconsistent results. This is likely due to differences in the way people took olive leaf extract, how much they took and how long for. This type of inconsistency normally tells us we need some more research to clarify the health effects of olive leaves.
Can you eat olive leaves?
Olive leaves can be brewed into a tea, or the leaves added to salads. Others report grinding olive leaves into smoothies.
However the leaves are bitter, because of the antioxidants, which can make them hard to eat, or the tea unpalatable.
Olive leaf extract has also been added to bread and other baked goods. Researchers find this improves the level of antioxidants in these products and people say the foods tasted better.
Olive leaves can taste bitter, which can put people off. But you can bake the extract into bread. Repina Valeriya/Shutterstock Is olive leaf extract toxic?
No, there seem to be no reported toxic effects of eating or drinking olive leaf extract.
It appears safe up to 1g a day, according to studies that have used olive leaf extract. However, there are no official guidelines about how much is safe to consume.
There have been reports of potential toxicity if taken over 85mg/kg of body weight per day. For an 80kg adult, this would mean 6.8g a day, well above the dose used in the studies mentioned in this article.
Pregnant and breastfeeding women are recommended not to consume it as we don’t know if it’s safe for them.
What should I do?
If you have high blood pressure, diabetes or raised blood lipids you may see some benefit from taking olive leaf extract. But it is important you discuss this with your doctor first and not change any medications or start taking olive leaf extract until you have spoken to them.
But there are plenty of antioxidants in all plant foods, and you should try to eat a wide variety of different coloured plant foods. This will allow you to get a range of nutrients and antioxidants.
Olive leaf and its extract is not going to be a panacea for your health if you’re not eating a healthy diet and following other health advice.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: