Homeopathy: Evidence So Tiny That It’s Not there?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Homeopathy: Evidence So Tiny That It’s Not There?
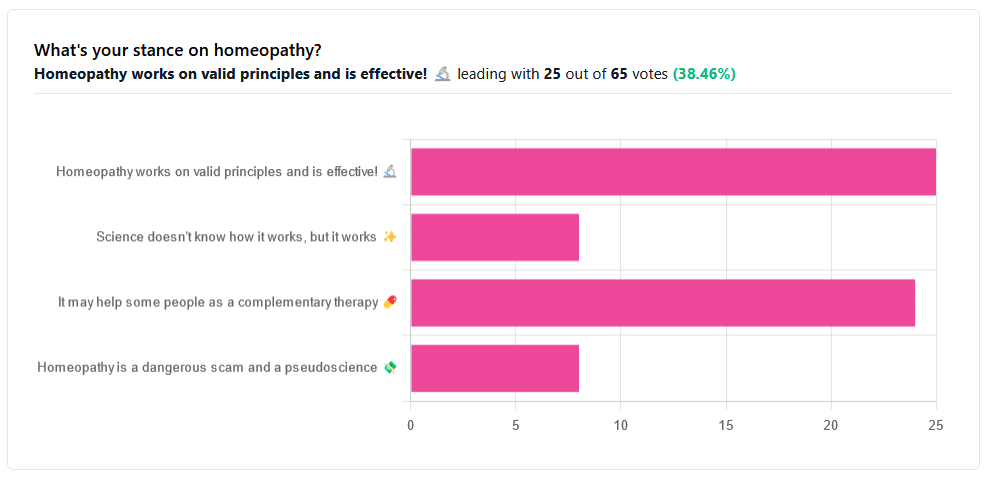
Yesterday, we asked you your opinions on homeopathy. The sample size of responses was a little lower than we usually get, but of those who did reply, there was a clear trend:
- A lot of enthusiasm for “Homeopathy works on valid principles and is effective”
- Near equal support for “It may help some people as a complementary therapy”
- Very few people voted for “Science doesn’t know how it works, but it works”; this is probably because people who considered voting for this, voted for the more flexible “It may help some people as a complementary therapy” instead.
- Very few people considered it a dangerous scam and a pseudoscience.
So, what does the science say?
Well, let us start our investigation by checking out the position of the UK’s National Health Service, an organization with a strong focus on providing the least expensive treatments that are effective.
Since homeopathy is very inexpensive to arrange, they will surely want to put it atop their list of treatments, right?
❝Homeopathy is a “treatment” based on the use of highly diluted substances, which practitioners claim can cause the body to heal itself.
There’s been extensive investigation of the effectiveness of homeopathy. There’s no good-quality evidence that homeopathy is effective as a treatment for any health condition.❞
The NHS actually has a lot more to say about that, and you can read their full statement here.
But that’s just one institution. Here’s what Australia’s National Health and Medical Research Council had to say:
❝There was no reliable evidence from research in humans that homeopathy was effective for treating the range of health conditions considered: no good-quality, well-designed studies with enough participants for a meaningful result reported either that homeopathy caused greater health improvements than placebo, or caused health improvements equal to those of another treatment❞
You can read their full statement here.
The American FDA, meanwhile, have a stronger statement:
❝Homeopathic drug products are made from a wide range of substances, including ingredients derived from plants, healthy or diseased animal or human sources, minerals and chemicals, including known poisons. These products have the potential to cause significant and even permanent harm if they are poorly manufactured, since that could lead to contaminated products or products that have potentially toxic ingredients at higher levels than are labeled and/or safe, or if they are marketed as substitute treatments for serious or life-threatening diseases and conditions, or to vulnerable populations.❞
You can read their full statement here.
Homeopathy is a dangerous scam and a pseudoscience: True or False?
False and True, respectively, mostly.
That may be a confusing answer, so let’s elaborate:
- Is it dangerous? Mostly not; it’s mostly just water. However, two possibilities for harm exist:
- Careless preparation could result in a harmful ingredient still being present in the water—and because of the “like cures like” principle, many of the ingredients used in homeopathy are harmful, ranging from heavy metals to plant-based neurotoxins. However, the process of “ultra-dilution” usually removes these so thoroughly that they are absent or otherwise scientifically undetectable.
- Placebo treatment has its place, but could result in “real” treatment going undelivered. This can cause harm if the “real” treatment was critically needed, especially if it was needed on a short timescale.
- Is it a scam? Probably mostly not; to be a scam requires malintent. Most practitioners probably believe in what they are practising.
- Is it a pseudoscience? With the exception that placebo effect has been highly studied and is a very valid complementary therapy… Yes, aside from that it is a pseudoscience. There is no scientific evidence to support homeopathy’s “like cures like” principle, and there is no scientific evidence to support homeopathy’s “water memory” idea. On the contrary, they go against the commonly understood physics of our world.
It may help some people as a complementary therapy: True or False?
True! Not only is placebo effect very well-studied, but best of all, it can still work as a placebo even if you know that you’re taking a placebo… Provided you also believe that!
Science doesn’t know how it works, but it works: True or False?
False, simply. At best, it performs as a placebo.
Placebo is most effective when it’s a remedy against subjective symptoms, like pain.
However, psychosomatic effect (the effect that our brain has on the rest of our body, to which it is very well-connected) can mean that placebo can also help against objective symptoms, like inflammation.
After all, our body, directed primarily by the brain, can “decide” what immunological defenses to deploy or hold back, for example. This is why placebo can help with conditions as diverse as arthritis (an inflammatory condition) or diabetes (an autoimmune condition, and/or a metabolic condition, depending on type).
Here’s how homeopathy measures up, for those conditions:
(the short answer is “no better than placebo”)
Homeopathy works on valid principles and is effective: True or False?
False, except insofar as placebo is a valid principle and can be effective.
The stated principles of homeopathy—”like cures like” and “water memory”—have no scientific basis.
We’d love to show the science for this, but we cannot prove a negative.
However, the ideas were conceived in 1796, and are tantamount to alchemy. A good scientific attitude means being open-minded to new ideas and testing them. In homeopathy’s case, this has been done, extensively, and more than 200 years of testing later, homeopathy has consistently performed equal to placebo.
In summary…
- If you’re enjoying homeopathic treatment and that’s working for you, great, keep at it.
- If you’re open-minded to enjoying a placebo treatment that may benefit you, be careful, but don’t let us stop you.
- If your condition is serious, please do not delay seeking evidence-based medical treatment.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid Slipping Into (Bad) Old Habits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Treating Bad Habits Like Addictions
How often have you started a healthy new habit (including if it’s a “quit this previous thing” new habit), only to find that you slip back into your old ways?
We’ve written plenty on habit-forming before, so here’s a quick recap before we continue:
How To Really Pick Up (And Keep!) Those Habits
…and even how to give them a boost:
How To Keep On Keeping On… Long Term!
But how to avoid the relapses that are most likely to snowball?
Borrowing from the psychology of addiction recovery
It’s well known that someone recovering from substance addiction should not have even a small amount of the thing they were addicted to. Not one sip of champagne at a wedding, not one drag of a cigarette, and so forth.
This can go for other bad habits too; make one exception, and suddenly you have a whole string of “exceptions”, and before you know it, it’s not the exception anymore; it’s the new rule—again.
Three things that can help guard against this are:
- Absolutely refuse to romanticize the bad habit. Do not fall for its marketing! And yes, everything has marketing even if not advertising; for example, consider the Platonic ideal of a junk-food-eating couch-potato who is humble, unassuming, agreeable, the almost-holy idea of homely comfort, and why shouldn’t we be comfortable after all, haven’t we earned our chosen hedonism, and so on. It’s seductive, and we need to make the choice to not be seduced by it. In this case for example, yes pleasure is great, but being sick tired and destroying our bodies is not, in fact, pleasurable in the long run. Which brings us to…
- Absolutely refuse to forget why you dropped that behavior in the first place. Remember what it did to you, remember you at your worst. Remember what you feared might become of you if you continued like that. This is something where journaling helps, by the way; remembering our low points helps us to avoid finding ourselves in the same situation again.
- Absolutely refuse to let your guard down due to an overabundance of self-confidence in your future self. We all can easily feel that tomorrow is a mystical land in which all productivity is stored, and also where we are strong, energized, iron-willed, and totally able to avoid making the very mistakes that we are right now in the process of making. Instead, be that strong person now, for the benefit of tomorrow’s you. Because after all, if it’s going to be easy tomorrow, it’s easy now, right?
The above is a very simple, hopefully practical, set of rules to follow. If you like hard science more though, Yale’s Dr. Steven Melemis offers five rules (aimed more directly at addiction recovery, so this may be a big “heavy guns” for some milder habits):
- change your life
- be completely honest
- ask for help
- practice self-care
- don’t bend the rules
You can read his full paper and the studies it’s based on, here:
Relapse Prevention and the Five Rules of Recovery
“What if I already screwed up?”
Draw a line under it, now, and move forwards in the direction you actually want to go.
Here’s a good article, that saves us taking up more space here; it’s very well-written so we do recommend it:
The Abstinence Violation Effect and Overcoming It
this article gives specific, practical advices, including CBT tools to use
Take care!
Share This Post
-
From immunotherapy to mRNA vaccines – the latest science on melanoma treatment explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More than 16,000 Australians will be diagnosed with melanoma each year. Most of these will be caught early, and can be cured by surgery.
However, for patients with advanced or metastatic melanoma, which has spread from the skin to other organs, the outlook was bleak until the advent of targeted therapies (that attack specific cancer traits) and immune therapies (that leverage the immune system). Over the past decade, these treatments have seen a significant climb in the number of advanced melanoma patients surviving for at least five years after diagnosis, from less than 10% in 2011 to around 50% in 2021.
While this is great news, there are still many melanoma patients who cannot be treated effectively with current therapies. Researchers have developed two exciting new therapies that are being evaluated in clinical trials for advanced melanoma patients. Both involve the use of immunotherapy at different times and in different ways.
The first results from these trials are now being shared publicly, offering insight into the future of melanoma treatment.
Svitlana Hulko/Shutterstock Immunotherapy before surgery
Immunotherapy works by boosting the power of a patient’s immune system to help kill cancer cells. One type of immunotherapy uses something called “immune checkpoint inhibitors”.
Immune cells carry “immune checkpoint” proteins, which control their activity. Cancer cells can interact with these checkpoints to turn off immune cells and hide from the immune system. Immune checkpoint inhibitors block this interaction and help keep the immune system activated to fight the cancer.
Results from an ongoing phase 3 trial using immune checkpoint inhibitors were recently published in the New England Journal of Medicine.
This trial used two types of immune checkpoint inhibitors: nivolumab, which blocks an immune checkpoint called PD-1, and ipilimumab, which blocks CTLA-4.
More than 16,000 Australians are diagnosed with melanoma each year. Delovely Pics/Shutterstock Some 423 patients (including many from Australia) were enrolled in the trial, and participants were randomly assigned to one of two groups.
The first group had surgery to remove their melanoma, and were then given immunotherapy (nivolumab) to help kill any remaining cancer cells. Giving a systemic (whole body) therapy such as immunotherapy after surgery is a standard way of treating melanoma. The second group received immunotherapy first (nivolumab plus ipilimumab) and then underwent surgery. This is a new approach to treating these cancers.
Based on previous observations, the researchers had predicted that giving patients immunotherapy while the whole tumour was still present would activate the tumour-fighting abilities of the patient’s immune system much better than giving it once the tumour had been removed.
Sure enough, 12 months after starting therapy, 83.7% of patients who received immunotherapy before surgery remained cancer-free, compared to 57.2% in the control group who received immunotherapy after surgery.
Based on these results, Australian of the year Georgina Long – who co-led the trial with Christian Blank from The Netherlands Cancer Institute – has suggested this method of immunotherapy before surgery should be considered a new standard of treatment for higher risk stage 3 melanoma. She also said a similar strategy should be evaluated for other cancers.
The promising results of this phase 3 trial suggest we might see this combination treatment being used in Australian hospitals within the next few years.
mRNA vaccines
Another emerging form of melanoma therapy is the post-surgery combination of a different checkpoint inhibitor (pembrolizumab, which blocks PD-1), with a messenger RNA vaccine (mRNA-4157).
While checkpoint inhibitors like pembrolizumab have been around for more than a decade, mRNA vaccines like mRNA-4157 are a newer phenomenon. You might be familiar with mRNA vaccines though, as the biotechnology companies Pfizer-BioNTech and Moderna released COVID vaccines based on mRNA technology.
mRNA-4157 works basically the same way – the mRNA is injected into the patient and produces antigens, which are small proteins that train the body’s immune system to attack a disease (in this case, cancer, and for COVID, the virus).
However, mRNA-4157 is unique – literally. It’s a type of personalised medicine, where the mRNA is created specifically to match a patient’s cancer. First, the patient’s tumour is genetically sequenced to figure out what antigens will best help the immune system to recognise their cancer. Then a patient-specific version of mRNA-4157 is created that produces those antigens.
The latest results of a three-year, phase 2 clinical trial which combined pembrolizumab and mRNA-4157 were announced this past week. Overall, 2.5 years after starting the trial, 74.8% of patients treated with immunotherapy combined with mRNA-4157 post-surgery remained cancer-free, compared to 55.6% of those treated with immunotherapy alone. These were patients who were suffering from high-risk, late-stage forms of melanoma, who generally have poor outcomes.
It’s worth noting these results have not yet been published in peer-reviewed journals. They’re available as company announcements, and were also presented at some cancer conferences in the United States.
Based on the results of this trial, the combination of pembrolizumab and the vaccine progressed to a phase 3 trial in 2023, with the first patients being enrolled in Australia. But the final results of this trial are not expected until 2029.
It is hoped this mRNA-based anti-cancer vaccine will blaze a trail for vaccines targeting other types of cancer, not just melanoma, particularly in combination with checkpoint inhibitors to help stimulate the immune system.
Despite these ongoing advances in melanoma treatment, the best way to fight cancer is still prevention which, in the case of melanoma, means protecting yourself from UV exposure wherever possible.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, WEHI (Walter and Eliza Hall Institute of Medical Research) and John (Eddie) La Marca, Senior Research Officer, Blood Cells and Blood Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Considering taking Wegovy to lose weight? Here are the risks and benefits – and how it differs from Ozempic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The weight-loss drug Wegovy is now available in Australia.
Wegovy is administered as a once-weekly injection and is approved specifically for weight management. It’s intended to be used in combination with a reduced-energy diet and increased physical activity.
So how does Wegovy work and how much weight can you expect to lose while taking it? And what are the potential risks – and costs – for those who use it?
Let’s look at what the science says.
Halfpoint/Shutterstock What is Wegovy?
Wegovy is a brand name for the medication semaglutide. Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1RA). This means it makes your body’s own glucagon-like peptide-1 hormone, called GLP-1 for short, work better.
Normally when you eat, the body releases the GLP-1 hormone which helps signal to your brain that you are full. Semaglutides enhance this effect, leading to a feeling of fullness, even when you haven’t eaten.
Another role of GLP-1 is to stimulate the body to produce more insulin, a hormone which helps lower the level of glucose (sugar) in the blood. That’s why semaglutides have been used for several years to treat type 2 diabetes.
Wegovy is self-injected once a week. S Becker/Shutterstock How does Wegovy differ from Ozempic?
Like Wegovy, Ozempic is a semaglutide. The way Wegovy and Ozempic work in the body are essentially the same. They’re made by the same pharmaceutical company, Novo Nordisk.
But there are two differences:
1) They are approved for two different (but related) reasons.
In Australia (and the United States), Ozempic is approved for use to improve blood glucose levels in adults with type 2 diabetes. By managing blood glucose levels effectively, the medication aims to reduce the risk of major complications, such as heart disease.
Wegovy is approved for use alongside diet and exercise for people with a body mass index (BMI) of 30 or greater, or 27 or greater but with other conditions such as high blood pressure.
Wegovy can also be used in people aged 12 years and older. Like Ozempic, Wegovy aims to reduce the risk of future health complications, including heart disease.
2) They are both injected but come in different strengths.
Ozempic is available in pre-loaded single-dose pens with varying dosages of 0.25 mg, 0.5 mg, 1 mg, or 2 mg per injection. The dose can be slowly increased, up to a maximum of 2 mg per week, if needed.
Wegovy is available in prefilled single-dose pens with doses of 0.25 mg, 0.5 mg, 1 mg, 1.7 mg, or 2.4 mg. The treatment starts with a dose of 0.25 mg once weekly for four weeks, after which the dose is gradually increased until reaching a maintenance dose of 2.4 mg weekly.
While it’s unknown what the impact of Wegovy’s introduction will be on Ozempic’s availability, Ozempic is still anticipated to be in low supply for the remainder of 2024.
Is Wegovy effective for weight loss?
Given Wegovy is a semaglutide, there is very strong evidence it can help people lose weight and maintain this weight loss.
A recent study found that over four years, participants taking Wevovy as indicated experienced an average weight loss of 10.2% body weight and a reduction in waist circumference of 7.7cm.
For those who stop taking the medication, analyses have shown that about two-thirds of weight lost is regained.
Wegovy can help people lose weight and maintain their weight loss – while they take the drug. Mladen Mitrinovic/Shutterstock What are the side effects of Wegovy?
The most common side effects are nausea and vomiting.
However, other serious side effects are also possible because of the whole-of-body impact of the medication. Thyroid tumours and cancer have been detected as a risk in animal studies, yet are rarely seen in human scientific literature.
In the four-year Wegovy trial, 16.6% of participants who received Wegovy (1,461 people) experienced an adverse event that led to them permanently discontinuing their use of the medication. This was higher than the 8.2% of participants (718 people) who received the placebo (with no active ingredient).
Side effects included gastrointestinal disorders (including nausea and vomiting), which affected 10% of people who used Wegovy compared to 2% of people who used the placebo.
Gallbladder-related disorders occurred in 2.8% of people who used Wegovy, and 2.3% of people who received the placebo.
Recently, concerns about suicidal thoughts and behaviours have been raised, after a global analysis reviewed more than 36 million reports of adverse events from semaglutide (Ozempic or Wegovy) since 2000.
There were 107 reports of suicidal thoughts and self-harm among people taking semaglutide, sadly including six actual deaths. When people stopped the medication, 62.5% found the thoughts went away. What we don’t know is whether dose, weight loss, or previous mental health status or use of antidepressants had a role to play.
Finally, concerns are growing about the negative effect of semaglutides on our social and emotional connection with food. Anecdotal and scientific evidence suggests people who use semaglutides significantly reduce their daily dietary intake (as anticipated) by skipping meals and avoiding social occasions – not very enjoyable for people and their loved ones.
How can people access Wegovy?
Wegovy is available for purchase at pharmacists with a prescription from a doctor.
But there is a hefty price tag. Wegovy is not currently subsidised through the Pharmaceutical Benefits Scheme, leaving patients to cover the cost. The current cost is estimated at around A$460 per month dose.
If you’re considering Wegovy, make an appointment with your doctor for individual advice.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
What are ‘collarium’ sunbeds? Here’s why you should stay away
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reports have recently emerged that solariums, or sunbeds – largely banned in Australia because they increase the risk of skin cancer – are being rebranded as “collarium” sunbeds (“coll” being short for collagen).
Commercial tanning and beauty salons in Queensland, New South Wales and Victoria are marketing collariums, with manufacturers and operators claiming they provide a longer lasting tan and stimulate collagen production, among other purported benefits.
A collarium sunbed emits both UV radiation and a mix of visible wavelength colours to produce a pink or red light. Like an old-school sunbed, the user lies in it for ten to 20 minute sessions to quickly develop a tan.
But as several experts have argued, the providers’ claims about safety and effectiveness don’t stack up.
Why were sunbeds banned?
Commercial sunbeds have been illegal across Australia since 2016 (except for in the Northern Territory) under state-based radiation safety laws. It’s still legal to sell and own a sunbed for private use.
Their dangers were highlighted by young Australians including Clare Oliver who developed melanoma after using sunbeds. Oliver featured in the No Tan Is Worth Dying For campaign and died from her melanoma at age 26 in 2007.
Sunbeds lead to tanning by emitting UV radiation – as much as six times the amount of UV we’re exposed to from the summer sun. When the skin detects enough DNA damage, it boosts the production of melanin, the brown pigment that gives you the tanned look, to try to filter some UV out before it hits the DNA. This is only partially successful, providing the equivalent of two to four SPF.
Essentially, if your body is producing a tan, it has detected a significant amount of DNA damage in your skin.
Research shows people who have used sunbeds at least once have a 41% increased risk of developing melanoma, while ten or more sunbed sessions led to a 100% increased risk.
In 2008, Australian researchers estimated that each year, sunbeds caused 281 cases of melanoma, 2,572 cases of squamous cell carcinoma (another common type of skin cancer), and $3 million in heath-care costs, mostly to Medicare.
How are collarium sunbeds supposed to be different?
Australian sellers of collarium sunbeds imply they are safe, but their machine descriptions note the use of UV radiation, particularly UVA.
UVA is one part of the spectrum of UV radiation. It penetrates deeper into the skin than UVB. While UVB promotes cancer-causing mutations by discharging energy straight into the DNA strand, UVA sets off damage by creating reactive oxygen species, which are unstable compounds that react easily with many types of cell structures and molecules. These damage cell membranes, protein structures and DNA.
Evidence shows all types of sunbeds increase the risk of melanoma, including those that use only UVA.
Some manufacturers and clinics suggest the machine’s light spectrum increases UV compatibility, but it’s not clear what this means. Adding red or pink light to the mix won’t negate the harm from the UV. If you’re getting a tan, you have a significant amount of DNA damage.
Collagen claims
One particularly odd claim about collarium sunbeds is that they stimulate collagen.
Collagen is the main supportive tissue in our skin. It provides elasticity and strength, and a youthful appearance. Collagen is constantly synthesised and broken down, and when the balance between production and recycling is lost, the skin loses strength and develops wrinkles. The collagen bundles become thin and fragmented. This is a natural part of ageing, but is accelerated by UV exposure.
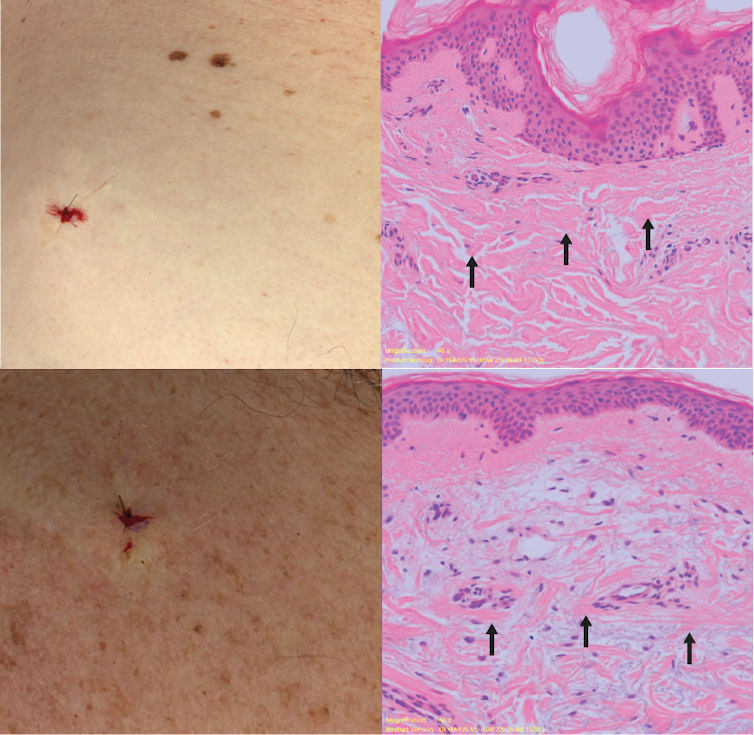
Sun-protected skin (top) has thick bands of pink collagen (arrows) in the dermis, as seen on microscopic examination. Chronically sun-damaged skin (bottom) has much thinner collagen bands.
Katie Lee/UQThe reactive oxygen species generated by UVA light damage existing collagen structures and kick off a molecular chain of events that downgrades collagen-producing enzymes and increases collagen-destroying enzymes. Over time, a build-up of degraded collagen fragments in the skin promotes even more destruction.
While there is growing evidence red light therapy alone could be useful in wound healing and skin rejuvenation, the UV radiation in collarium sunbeds is likely to undo any benefit from the red light.
What about phototherapy?
There are medical treatments that use controlled UV radiation doses to treat chronic inflammatory skin diseases like psoriasis.
The anti-collagen effects of UVA can also be used to treat thickened scars and keloids. Side-effects of UV phototherapy include tanning, itchiness, dryness, cold sore virus reactivation and, notably, premature skin ageing.
These treatments use the minimum exposure necessary to treat the condition, and are usually restricted to the affected body part to minimise risks of future cancer. They are administered under medical supervision and are not recommended for people already at high risk of skin cancer, such as people with atypical moles.
So what happens now?
It looks like many collariums are just sunbeds rebranded with red light. Queensland Health is currently investigating whether these salons are breaching the state’s Radiation Safety Act, and operators could face large fines.
As the 2024 Australians of the Year – melanoma treatment pioneers Georgina Long and Richard Scolyer – highlighted in their acceptance speech, “there is nothing healthy about a tan”, and we need to stop glamorising tanning.
However, if you’re desperate for the tanned look, there is a safer and easy way to get one – out of a bottle or by visiting a salon for a spray tan.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Anne Cust, Professor of Cancer Epidemiology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
More Mediterranean – by American’s Test Kitchen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Regular 10almonds readers will know that we talk about the Mediterranean diet often, and with good reason; it’s been for quite a while now the “Gold Standard” when it comes to scientific consensus on what constitutes a good diet for healthy longevity.
However, it’s easy to get stuck in a rut of cooking the same three meals and thinking “I must do something different, but not today, because I have these ingredients and don’t know what to cook” and then when one is grocery-shopping, it’s “I should have researched a new thing to cook, but since I haven’t, I’ll just get the ingredients for what I usually cook, since we need to eat”, and so the cycle continues.
This book will help break you out of that cycle! With (as the subtitle promises) hundreds of recipes, there’s no shortage of good ideas. The recipes are “plant-forward” rather than plant-based per se (i.e. there are some animal products in them), though for the vegetarians and vegans, it’s nothing that’s any challenge to substitute.
Bottom line: if you’re looking for “delicious and nutritious”, this book is sure to put a rainbow on your plate and a smile on your face.
Click here to check out More Mediterranean, and inspire your kitchen!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tuna vs Catfish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tuna to catfish, we picked the tuna.
Why?
Today in “that which is more expensive and/or harder to get is not necessarily healthier”…
Looking at their macros, tuna has more protein and less fat (and overall, less saturated fat, and also less cholesterol).
In the category of vitamins, both are good but tuna distinguishes itself: tuna has more of vitamins A, B1, B2, B3, B6, and D, while catfish has more of vitamins B5, B9, B12, E, and K. They are both approximately equal in choline, and as an extra note in tuna’s favor (already winning 6:5), tuna is a very good source of vitamin D, while catfish barely contains any. All in all: a moderate, but convincing, win for tuna.
When it comes to minerals, things are clearer still: tuna has more copper, iron, magnesium, phosphorus, potassium, and selenium, while catfish has more calcium, manganese, and zinc. Oh, and catfish is also higher in one other mineral: sodium, which most people in industrialized countries need less of, on average. So, a 6:3 win for tuna, before we even take into account the sodium content (which makes the win for tuna even stronger).
In short: tuna wins the day in every category!
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught (It Makes Quite A Difference)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: