Thriving Beyond Fifty – by Will Harlow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve featured this author sometimes in our video section; he’s an over-50s specialist physiotherapist with a lot of very functional advice to offer.
In this book, Harlow focusses heavily on three things: mobility, strength, endurance.
You may not want to be a gymnast, powerlifter, or marathon-runner, but these things are important for us all to maintain to at least a fair degree:
- Mobility can be the difference between tweaking one’s shoulder getting something from a high shelf, or not
- Strength can be the difference between being able to get back up, or not
- Endurance can be the difference between coming back from a long day on your feet and thinking “that was a good day; I’m looking forward to tomorrow now”, or not
One of the greatest strengths of this book is its comprehensive troubleshooting aspect; if you have a weak spot, chances are this book has the remedy.
As for the style, it’s quite casual/conversational in tone, but without skimping on science and detail. It’s clear, explanatory, and helpful throughout.
Bottom line: if you’d like to maintain/improve mobility, strength, and endurance, then this book is a very recommendable resource.
Click here to check out Thriving Beyond Fifty, and keep thriving at every age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Horse Sedative Use Among Humans Spreads in Deadly Mixture of ‘Tranq’ and Fentanyl
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
TREASURE ISLAND, Fla. — Andrew McClave Jr. loved to lift weights. The 6-foot-4-inch bartender resembled a bodybuilder and once posed for a photo flexing his muscles with former pro wrestler Hulk Hogan.
“He was extremely dedicated to it,” said his father, Andrew McClave Sr., “to the point where it was almost like he missed his medication if he didn’t go.”
But the hobby took its toll. According to a police report, a friend told the Treasure Island Police Department that McClave, 36, suffered from back problems and took unprescribed pills to reduce the pain.
In late 2022, the friend discovered McClave in bed. He had no pulse. A medical examiner determined he had a fatal amount of fentanyl, cocaine, and xylazine, a veterinary tranquilizer used to sedate horses, in his system, an autopsy report said. Heart disease was listed as a contributing factor.
McClave is among more than 260 people across Florida who died in one year from accidental overdoses involving xylazine, according to a Tampa Bay Times analysis of medical examiner data from 2022, the first year state officials began tracking the substance. Numbers for 2023 haven’t been published.
The death toll reflects xylazine’s spread into the nation’s illicit drug supply. Federal regulators approved the tranquilizer for animals in the early 1970s and it’s used to sedate horses for procedures like oral exams and colic treatment, said Todd Holbrook, an equine medicine specialist at the University of Florida. Reports of people using xylazine emerged in Philadelphia, then the drug spread south and west.
What’s not clear is exactly what role the sedative plays in overdose deaths, because the Florida data shows no one fatally overdosed on xylazine alone. The painkiller fentanyl was partly to blame in all but two cases in which the veterinary drug was included as a cause of death, according to the Times analysis. Cocaine or alcohol played roles in the cases in which fentanyl was not involved.
Fentanyl is generally the “800-pound gorilla,” according to Lewis Nelson, chair of the emergency medicine department at Rutgers New Jersey Medical School, and xylazine may increase the risk of overdose, though not substantially.
But xylazine appears to complicate the response to opioid overdoses when they do happen and makes it harder to save people. Xylazine can slow breathing to dangerous levels, according to federal health officials, and it doesn’t respond to the overdose reversal drug naloxone, often known by the brand name Narcan. Part of the problem is that many people may not know they are taking the horse tranquilizer when they use other drugs, so they aren’t aware of the additional risks.
Lawmakers in Tallahassee made xylazine a Schedule 1 drug like heroin or ecstasy in 2016, and several other states including Pennsylvania, Ohio, and West Virginia have taken action to classify it as a scheduled substance, too. But it’s not prohibited at the federal level. Legislation pending in Congress would criminalize illicit xylazine use nationwide.
The White House in April designated the combination of fentanyl and xylazine, often called “tranq dope,” as an emerging drug threat. A study of 20 states and Washington, D.C., found that overdose deaths attributed to both illicit fentanyl and xylazine exploded from January 2019 to June 2022, jumping from 12 a month to 188.
“We really need to continue to be proactive,” said Amanda Bonham-Lovett, program director of a syringe exchange in St. Petersburg, “and not wait until this is a bigger issue.”
‘A Good Business Model’
There are few definitive answers about why xylazine use has spread — and its impact on people who consume it.
The U.S. Drug Enforcement Administration in September said the tranquilizer is entering the country in several ways, including from China and in fentanyl brought across the southwestern border. The Florida attorney general’s office is prosecuting an Orange County drug trafficking case that involves xylazine from a New Jersey supplier.
Bonham-Lovett, who runs IDEA Exchange Pinellas, the county’s anonymous needle exchange, said some local residents who use drugs are not seeking out xylazine — and don’t know they’re consuming it.
One theory is that dealers are mixing xylazine into fentanyl because it’s cheap and also affects the brain, Nelson said.
“It’s conceivable that if you add a psychoactive agent to the fentanyl, you can put less fentanyl in and still get the same kick,” he said. “It’s a good business model.”
In Florida, men accounted for three-quarters of fatal overdoses involving xylazine, according to the Times analysis. Almost 80% of those who died were white. The median age was 42.
Counties on Florida’s eastern coast saw the highest death tolls. Duval County topped the list with 46 overdoses. Tampa Bay recorded 19 fatalities.
Cocaine was also a cause in more than 80 cases, including McClave’s, the Times found. The DEA in 2018 warned of cocaine laced with fentanyl in Florida.
In McClave’s case, Treasure Island police found what appeared to be marijuana and a small plastic bag with white residue in his room, according to a police report. His family still questions how he took the powerful drugs and is grappling with his death.
He was an avid fisherman, catching snook and grouper in the Gulf of Mexico, said his sister, Ashley McClave. He dreamed of being a charter boat captain.
“I feel like I’ve lost everything,” his sister said. “My son won’t be able to learn how to fish from his uncle.”
Mysterious Wounds
Another vexing challenge for health officials is the link between chronic xylazine use and open wounds.
The wounds are showing up across Tampa Bay, needle exchange leaders said. The telltale sign is blackened, crusty tissue, Bonham-Lovett said. Though the injuries may start small — the size of a dime — they can grow and “take over someone’s whole limb,” she said.
Even those who snort fentanyl, instead of injecting it, can develop them. The phenomenon is unexplained, Nelson said, and is not seen in animals.
IDEA Exchange Pinellas has recorded at least 10 cases since opening last February, Bonham-Lovett said, and has a successful treatment plan. Staffers wash the wounds with soap and water, then dress them.
One person required hospitalization partly due to xylazine’s effects, Bonham-Lovett said. A 31-year-old St. Petersburg woman, who asked not to be named due to concerns over her safety and the stigma of drug use, said she was admitted to St. Anthony’s Hospital in 2023. The woman, who said she uses fentanyl daily, had a years-long staph infection resistant to some antibiotics, and a wound recently spread across half her thigh.
The woman hadn’t heard of xylazine until IDEA Exchange Pinellas told her about the drug. She’s thankful she found out in time to get care.
“I probably would have lost my leg,” she said.
This article was produced in partnership with the Tampa Bay Times.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
As Nuns Disappear, Many Catholic Hospitals Look More Like Megacorporations
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ST. LOUIS — Inside the more than 600 Catholic hospitals across the country, not a single nun can be found occupying a chief executive suite, according to the Catholic Health Association.
Nuns founded and led those hospitals in a mission to treat sick and poor people, but some were also shrewd business leaders. Sister Irene Kraus, a former chief executive of Daughters of Charity National Health System, was famous for coining the phrase “no margin, no mission.” It means hospitals must succeed — generating enough revenue to exceed expenses — to fulfill their original mission.
The Catholic Church still governs the care that can be delivered to millions in those hospitals each year, using religious directives to ban abortions and limit contraceptives, in vitro fertilization, and medical aid in dying.
But over time, that focus on margins led the hospitals to transform into behemoths that operate for-profit subsidiaries and pay their executives millions, according to hospital tax filings. These institutions, some of which are for-profit companies, now look more like other megacorporations than like the charities for the destitute of yesteryear.
The absence of nuns in the top roles raises the question, said M. Therese Lysaught, a Catholic moral theologist and professor at Loyola University Chicago: “What does it mean to be a Catholic hospital when the enterprise has been so deeply commodified?”
The St. Louis area serves as the de facto capital of Catholic hospital systems. Three of the largest are headquartered here, along with the Catholic hospital lobbying arm. Catholicism is deeply rooted in the region’s culture. During Pope John Paul II’s only U.S. stop in 1999, he led Mass downtown in a packed stadium of more than 100,000 people.
For a quarter century, Sister Mary Jean Ryan led SSM Health, one of those giant systems centered on St. Louis. Now retired, the 86-year-old said she was one of the last nuns in the nation to lead a Catholic hospital system.
Ryan grew up Catholic in Wisconsin and joined a convent while in nursing school in the 1960s, surprising her family. She admired the nuns she worked alongside and felt they were living out a higher purpose.
“They were very impressive,” she said. “Not that I necessarily liked all of them.”
Indeed, the nuns running hospitals defied the simplistic image often ascribed to them, wrote John Fialka in his book “Sisters: Catholic Nuns and the Making of America.”
“Their contributions to American culture are not small,” he wrote. “Ambitious women who had the skills and the stamina to build and run large institutions found the convent to be the first and, for a long time, the only outlet for their talents.”
This was certainly true for Ryan, who climbed the ranks, working her way from nurse to chief executive of SSM Health, which today has hospitals in Illinois, Missouri, Oklahoma, and Wisconsin.
The system was founded more than a century ago when five German nuns arrived in St. Louis with $5. Smallpox swept through the city and the Sisters of St. Mary walked the streets offering free care to the sick.
Their early foray grew into one of the largest Catholic health systems in the country, with annual revenue exceeding $10 billion, according to its 2023 audited financial report. SSM Health treats patients in 23 hospitals and co-owns a for-profit pharmacy benefit manager, Navitus, that coordinates prescriptions for 14 million people.
But Ryan, like many nuns in leadership roles in recent decades, found herself confronted with an existential crisis. As fewer women became nuns, she had to ensure the system’s future without them.
When Ron Levy, who is Jewish, started at SSM as an administrator, he declined to lead a prayer in a meeting, Ryan recounted in her book, “On Becoming Exceptional.”
“Ron, I’m not asking you to be Catholic,” she recalled telling him. “And I know you’ve only been here two weeks. So, if you’d like to make it three, I suggest you be prepared to pray the next time you’re asked.”
Levy went on to serve SSM for more than 30 years — praying from then on, Ryan wrote.
In Catholic hospitals, meetings are still likely to start with a prayer. Crucifixes often adorn buildings and patient rooms. Mission statements on the walls of SSM facilities remind patients: “We reveal the healing presence of God.”
Above all else, the Catholic faith calls on its hospitals to treat everyone regardless of race, religion, or ability to pay, said Diarmuid Rooney, a vice president of the Catholic Health Association. No nuns run the trade group’s member hospitals, according to the lobbying group. But the mission that compelled the nuns is “what compels us now,” Rooney said. “It’s not just words on a wall.”
The Catholic Health Association urges its hospitals to evaluate themselves every three years on whether they’re living up to Catholic teachings. It created a tool that weighs seven criteria, including how a hospital acts as an extension of the church and cares for poor and marginalized patients.
“We’re not relying on hearsay that the Catholic identity is alive and well in our facilities and hospitals,” Rooney said. “We can actually see on a scale where they are at.”
The association does not share the results with the public.
At SSM Health, “our Catholic identity is deeply and structurally ingrained” even with no nun at the helm, spokesperson Patrick Kampert said. The system reports to two boards. One functions as a typical business board of directors while the other ensures the system abides by the rules of the Catholic Church. The church requires the majority of that nine-member board to be Catholic. Three nuns currently serve on it; one is the chair.
Separately, SSM also is required to file an annual report with the Vatican detailing the ways, Kampert said, “we deepen our Catholic identity and further the healing ministry of Jesus.” SSM declined to provide copies of those reports.
From a business perspective, though, it’s hard to distinguish a Catholic hospital system like SSM from a secular one, said Ruth Hollenbeck, a former Anthem insurance executive who retired in 2018 after negotiating Missouri hospital contracts. In the contracts, she said, the difference amounted to a single paragraph stating that Catholic hospitals wouldn’t do anything contrary to the church’s directives.
To retain tax-exempt status under Internal Revenue Service rules, all nonprofit hospitals must provide a “benefit” to their communities such as free or reduced-price care for patients with low incomes. But the IRS provides a broad definition of what constitutes a community benefit, which gives hospitals wide latitude to justify not needing to pay taxes.
On average, the nation’s nonprofit hospitals reported that 15.5% of their total annual expenses were for community benefits in 2020, the latest figure available from the American Hospital Association.
SSM Health, including all of its subsidiaries, spent proportionately far less than the association’s average for individual hospitals, allocating roughly the same share of its annual expenses to community efforts over three years: 5.1% in 2020, 4.5% in 2021, and 4.9% in 2022, according to a KFF Health News analysis of its most recent publicly available IRS filings and audited financial statements.
A separate analysis from the Lown Institute think tank placed five Catholic systems — including the St. Louis region’s Ascension — on its list of the 10 health systems with the largest “fair share” deficits, which means receiving more in tax breaks than what they spent on the community. And Lown said three St. Louis-area Catholic health systems — Ascension, SSM Health, and Mercy — had fair share deficits of $614 million, $235 million, and $92 million, respectively, in the 2021 fiscal year.
Ascension, Mercy, and SSM disputed Lown’s methodology, arguing it doesn’t take into account the gap between the payments they receive for Medicaid patients and the cost of delivering their care. The IRS filings do.
But, Kampert said, many of the benefits SSM provides aren’t reflected in its IRS filings either. The forms reflect “very simplistic calculations” and do not accurately represent the health system’s true impact on the community, he said.
Today, SSM Health is led by longtime business executive Laura Kaiser. Her compensation in 2022 totaled $8.4 million, including deferred payments, according to its IRS filing. Kampert defended the amount as necessary “to retain and attract the most qualified” candidate.
By contrast, SSM never paid Ryan a salary, giving instead an annual contribution to her convent of less than $2 million a year, according to some tax filings from her long tenure. “I didn’t join the convent to earn money,” Ryan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Meditation That You’ll Actually Enjoy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Meditation That You’ll Actually Enjoy
We previously wrote about…
No-Frills, Evidence-Based Mindfulness
this is a great primer, by the way, for the science and simplicity of mindfulness, along with the simplest mindfulness meditation to get you going.
Today, we’re going to have some fun with meditation.
First: The Problem
Once the usefulness and health benefits of meditation have been established, often people want to meditate, but complain they don’t have the time.
But that’s not the real reason, though, is it?
Let’s face it, a basic meditation can give benefits within two minutes. Or within two breaths, for that matter. So, it’s not really for a lack of time.
The real reason is because it doesn’t feel productive, and it’s not fun. For us to feel motivated to do a thing, usually we need at least one or the other. And even if we know it really is productive, it not feeling that way will hobble us.
So instead, let us make things a little more fun, with…
Meditation games!
As it turns out, there are good kinds of meditation with which one can have a little fun.
Catch the next thought
A common feature of many meditative practices is the experience of having fewer, or ideally no, thoughts.
But it’s hard to enact a negative, and thoughts keep coming.
So instead, make yourself comfortable, settle in, and lie in wait for thoughts. When one comes along, pounce on it in your mind. And then release it, and wait for the next.
At first, your thoughts may be coming thick and fast, but soon, you’ll find the pauses between them lengthening, and you have moments of contented not-knowing of what the next thought will be before it comes along.
This state of relaxed, ready alertness, calm and receptive, is exactly what we’re hoping to find here. But don’t worry about that while you’re busy lying in wait for the next wild thought to come along
Counting breaths
Many meditative practices involve focus on one’s breath. But it’s easy for attention to wander!
This game is a simple one. Count your breaths, not trying to change your rate of breathing at all, just letting it be, and see how high you can get before you lose count.
Breathing in and out, once, counts as one breath, by the way.
You may find that your rate of breathing naturally slows while you’re doing this. That’s fine; let it. It’ll add to the challenge of the game, because before long there will be lengthy pauses between each number.
If you lose count, just start again, and see if you can beat your high score.
This meditation game is an excellent exercise to build for sustained focus, while also improving the quality of breathing (as a side-effect of merely paying attention to it).
Hot spot, cold spot
The above two meditation games were drawn from Japanese and Chinese meditative practices, zen and qigong respectively; this one’s from an Indian meditative practice, yoga nidra. But for now, just approach it with a sense of playful curiosity, for best results.
Make yourself comfortable, lying on your back, arms by your sides.
Take a moment first to pay attention to each part of your body from head to toe, and release any tension that you may be holding along the way.
First part: mentally scan your body for where it feels warmest, or most active, or most wanting of attention (for example if there is pain, or an itch, or some other sensation); that’s your “hot spot” for the moment.
Second part: mentally scan your body for where it feels coolest, or most inert, or almost like it’s not a part of your body at all; that’s your “cold spot” for the moment.
Now, see if you can flip them. Whether you can or can’t, notice if your “hot spot” or “cold spot” moves, or if you can move them consciously.
This meditation game is a great exercise to strengthen interoception and somatic awareness in general—essential for being able to “listen to your body”!
Closing thoughts
All three practices above have very serious reasons and great benefits, but make sure you don’t skip enjoyment of the fun aspects!
Being “young at heart” is, in part, to do with the ability to enjoy—literally, to take joy in—the little things in life.
With that in mind, all we have left to say here is…
Enjoy!
Share This Post
Related Posts
-
Laugh Often, To Laugh Longest!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Putting The Abs Into Absurdity
We’ve talked before about the health benefits of a broadly positive outlook on life:
Optimism Seriously Increases Longevity!
…and we’re very serious about it, but that’s about optimistic life views in general, and today we’re about not just keeping good humor in questionable circumstances, but actively finding good humor in the those moments—even when the moments in question might not be generally described as good!
After all, laughter really can be the best medicine, for example:
From the roots
First a quick recap on de-toothing the psychological aspect of threats, no matter how menacing they may be:
Hello, Emotions: Time For Radical Acceptance!
…which we can then take a step further:
What’s The Worst That Could Happen?
Choose your frame
Do you remember when that hacker hacked and publicized the US Federal no-fly list, after already hacking a nationwide cloud-based security camera company, getting access to more than 150,000 companies’ and private individuals’ security cameras, amongst various other cyber crimes, mostly various kinds of fraud and data theft?
Imagine how she (age 21) must have felt, when being indicted. What do you suppose this hacker had to say for itself under such circumstances?
❝congress is investigating now 🙂
but i stay silly :3 ❞
…the latter half of which, usually rendered “but I stay silly” or “but we stay silly” has since entered popular Gen-Z parlance, usually after expressing some negative thing, often in a state of powerlessness.
Which is an important life skill if powerlessness is something that is often likely.
It’s important for many Gen-Zs with negligible life prospects economically; it’s equally important for 60-somethings getting cancer diagnoses (statistically the most likely decade to find out one has cancer, by the way), and many other kinds of people younger, older, and in between.
Because at the end of the day, we all start powerless and we all end powerless.
Learned helplessness (two kinds)
In psychology, “learned helplessness” occurs when a person or creature gives up after learning that all and any attempts to resist a Bad Thing™ fail, perhaps even badly. A lab rat may just shut down and sit there getting electroshocked, for example. A person subjected to abuse may stop trying to improve their situation, and just go with the path of least resistance.
But, there’s another kind, wherein someone in a position of absolute powerlessness not only makes their peace with that, but also, decides that the one thing the outside world can’t control, is how they take it. Like the hacker we mentioned earlier.
Sometimes the gallows humor is even more literal, laughing at one’s own impending death. Not as a matter of bravado, but genuinely seeing the funny side.
But how?
Unfortunately, fortunately
The trick here is to “find a silver lining” that is nowhere near enough to compensate for the bad thing—and it may even be worse! But that’s fine:
“Unfortunately, I didn’t have time to do the dishes before leaving for my vacation. Fortunately, I also forgot to turn the oven off, so the house burning down covered up my messy kitchen”
Writer’s personal less drastic example: today I set my espresso machine to press me an espresso; it doesn’t have an auto-off and I got distracted and it overflowed everywhere; my immediate reaction was “Oh! I have been blessed with an abundance of coffee!”
This kind of silly little thing, on a daily basis, builds a very solid habit for life that allows one to see the funny side in even the most absurd situations, even matters of life and death (can confirm: been there enough times personally—so far so good, still alive to find the remembered absurdity silly).
The point is not to genuinely value the “silver lining”, because half the time it isn’t even one, really, and it is useless to pretend, in seriousness.
But to pretend in silliness? Now we’re onto something, and the real benefit is in the laughs we had along the way.
Because those worst moments? Are probably when we need it the most, so it’s good to get some practice in!
Want more ways to find the funny and make it a life habit?
We reviewed a good book recently:
The Humor Habit: Rewire Your Brain To Stress Less, Laugh More, And Achieve More’er – by Paul Osincup
Stay silly!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
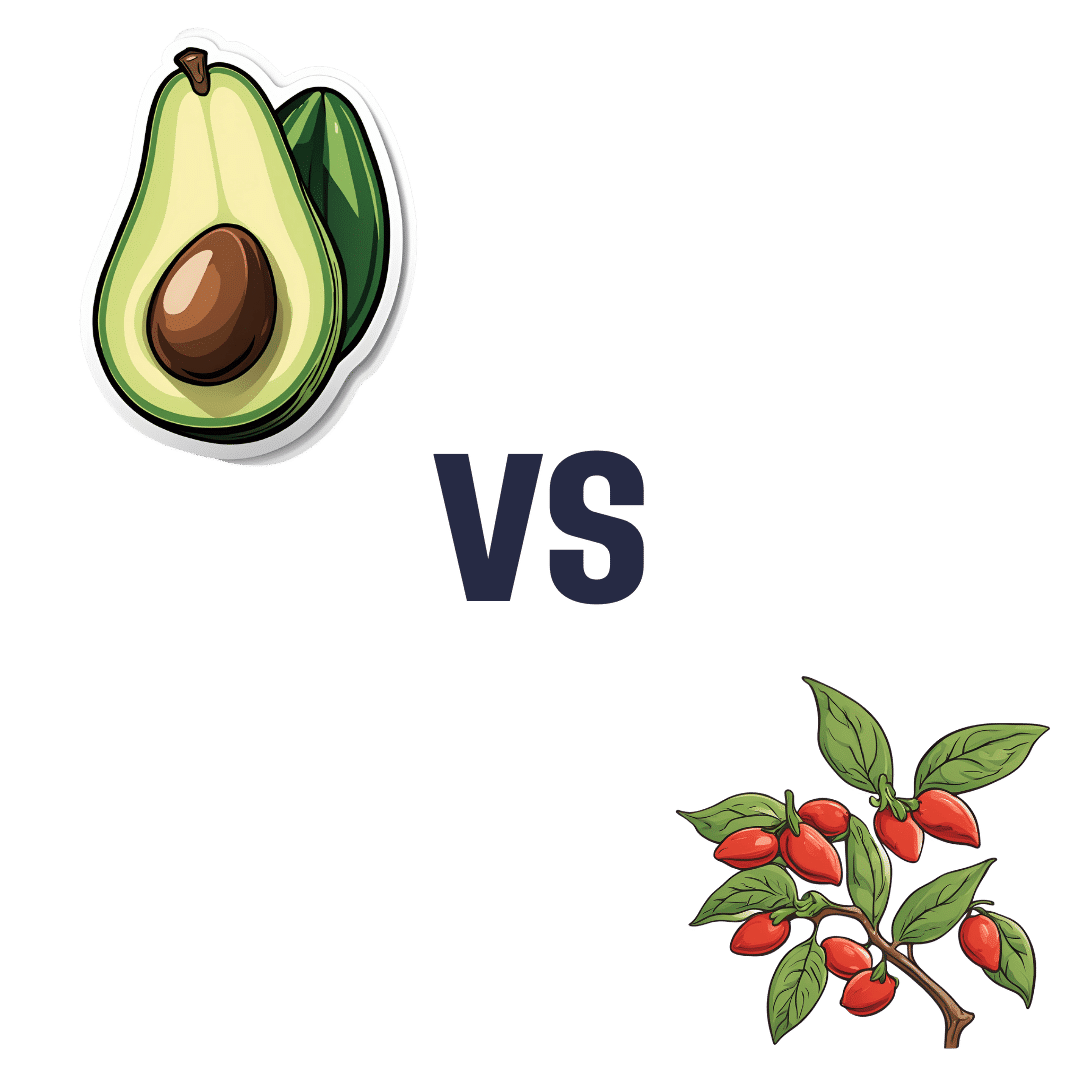
Avocado vs Goji Berries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to goji berries, we picked the avocado.
Why?
It takes a special non-dried food to beat a dried food for nutritional density, but avocado manages it!
In terms of macros, avocados have more (famously health) fat; mostly monounsaturated with some polyunsaturated and a little bit of saturated, with some omega-3 and omega-6, in a healthy ratio. Meanwhile, goji berries have more fiber, carbs, and protein. As for glycemic indices, avocados are low GI (40), but goji berries are zero-GI, or, functionally, a negative glycemic index as (notwithstanding their sugar content!) they have an overall lowering effect on blood sugars. In short, both of these fruits have very different things to offer in the macros category, so we’re declaring this round a tie.
In the category of vitamins, avocados have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, E, K, and choline, while goji berries have more vitamin C. A clear win for avocados!
When it comes to minerals, avocados have more copper, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while goji berries have more calcium and iron. Another win for avocados!
In short, enjoy either or both (diversity is good), but for overall nutritional density, avocados win this superfood showdown today.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aging Is Inevitable… Or is it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aging is inevitable… Or is it?
We’ve talked before about how and why aging happens. We’ve also talked about the work to tackle aging as basically an engineering problem, with the premise that our bodies are biological machines, and machines can be repaired. We also recommended a great book about this, by the way. But that’s about interfering with the biological process of aging. What about if the damage is already done?
“When the damage is done, it’s done”
We can do a lot to try to protect ourselves from aging, and we might be able to slow down the clock, but we can’t stop it, and we certainly can’t reverse it… right?
Wrong! Or at least, so we currently understand, in some respects. Supplementation with phosphatidylserine, for example, has shown promise for not just preventing, but treating, neurodegeneration (such as that caused by Alzheimer’s disease). It’s not a magic bullet and so far the science is at “probably” and “this shows great promise for…” and “this appears to…”
Phosphatidylserene does help slow neurodegeneration
…because of its role in allowing your cells to know whether they have permission to die.
This may seem a flippant way of putting it, but it’s basically how cell death works. Cells do need to die (if they don’t, that’s called cancer) and be replaced with new copies, and those copies need to be made before too much damage is accumulated (otherwise the damage is compounded with each new iteration). So an early cell death-and-replacement is generally better for your overall health than a later one.
However, neurons are tricky to replace, so phosphatidylserine effectively says “not you, hold on” to keep the rate of neuronal cell death nearer to the (slow) rate at which they can be replaced.
One more myth to bust…
For the longest time we thought that adults, especially older adults, couldn’t make new brain cells at all, that we grew a certain number, then had to hang onto them until we died… suffering diminished cognitive ability with age, on account of losing brain cells along the way.
It’s partly true: it’s definitely easier to kill brain cells than to grow them… Mind you, that’s technically true of people, too, yet the population continues to boom!
Anyway, new research showing that adults do, in fact, grow new braincells was briefly challenged by a 2018 study that declared: Human hippocampal neurogenesis drops sharply in children to undetectable levels in adults after all, never mind, go back to your business.
So was adult neurogenesis just a myth to be busted after all? Nope.
It turned out, the 2018 study had a methodological flaw!
To put it in lay terms: they had accidentally melted the evidence.
A 2019 study overcame this flaw by using a shorter fixation time for the cell samples they wanted to look at, and found that there were tens of thousands of “baby neurons” (again with the lay terms), newly-made brain cells, in samples from adults ranging from 43 to 87.
Now, there was still a difference: the samples from the youngest adult had 30% more newly-made braincells than the 87-year-old, but given that previous science thought brain cell generation stopped in childhood, the fact that an 87-year-old was generating new brain cells 30% less quickly than a 43-year-old is hardly much of a criticism!
As an aside: samples from patients with Alzheimer’s also had a 30% reduction in new braincell generation, compared to samples from patients of the same age without Alzheimer’s. But again… Even patients with Alzheimer’s were still growing some new brain cells.
Read it for yourself: Adult hippocampal neurogenesis is abundant in neurologically healthy subjects and drops sharply in patients with Alzheimer’s disease
In a nutshell…
- We can’t fully hit pause on aging just yet, but we can definitely genuinely slow it
- We can also, in some very specific ways, reverse it
- We can slow the loss of brain cells
- We can grow new brain cells
- We can reduce our risk of Alzheimer’s, and at least somewhat mitigate it if it appears
- We know that phosphatidylserine supplementation may help with most (if not all) of the above
- We don’t sell that (or anything else) but for your convenience, here it is on Amazon if you’re interested
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: