The Web That Has No Weaver – by Ted Kaptchuk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we have a strong “stick with the science” policy, and that means peer-reviewed studies and (where such exists) scientific consensus.
However, in the spirit of open-minded skepticism (i.e., acknowledging what we don’t necessarily know), it can be worth looking at alternatives to popular Western medicine. Indeed, many things have made their way from Traditional Chinese Medicine (or Ayurveda, or other systems) into Western medicine in any case.
“The Web That Has No Weaver” sounds like quite a mystical title, but the content is presented in the cold light of day, with constant “in Western terms, this works by…” notes.
The author walks a fine line of on the one hand, looking at where TCM and Western medicine may start and end up at the same place, by a different route; and on the other hand, noting that (in a very Daoist fashion), the route is where TCM places more of the focus, in contrast to Western medicine’s focus on the start and end.
He makes the case for TCM being more holistic, and it is, though Western medicine has been catching up in this regard since this book’s publication more than 20 years ago.
The style of the writing is very easy to follow, and is not esoteric in either mysticism or scientific jargon. There are diagrams and other illustrations, for ease of comprehension, and chapter endnotes make sure we didn’t miss important things.
Bottom line: if you’re curious about Traditional Chinese Medicine, this book is the US’s most popular introduction to such, and as such, is quite a seminal text.
Click here to check out The Web That Has No Weaver, and enjoy learning about something new!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Avocado vs Jackfruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to jackfruit, we picked the avocado.
Why?
In terms of macros, avocado is higher in fats (famously healthy ones, including a good dose of omega-3), fiber (nearly 5x more), and protein (despite jackfruit being more often used as a meaty element in recipes, avocado has slightly more). Meanwhile, jackfruit is about 3x higher in carbs. All in all, a clear win for avocado.
Looking at vitamins, avocado has more of vitamins A, B2, B3, B5, B7, B9, E, K, and choline, while jackfruit has more of vitamins B1, B6, and C. Another win for avocado in this category.
In the category of minerals, avocado has more copper, iron, manganese, phosphorus, potassium, selenium, and zinc, while jackfruit has more calcium. One more win for avocado.
Adding up the sections makes for an easy overall win for avocado, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Jackfruit vs Durian – Which is Healthier? ← including some fun durian facts (such as how to pick a good one, and what happens if you eat durian and drink alcohol)
Enjoy!
Share This Post
-
Grains: Bread Of Life, Or Cereal Killer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Going Against The Grain?
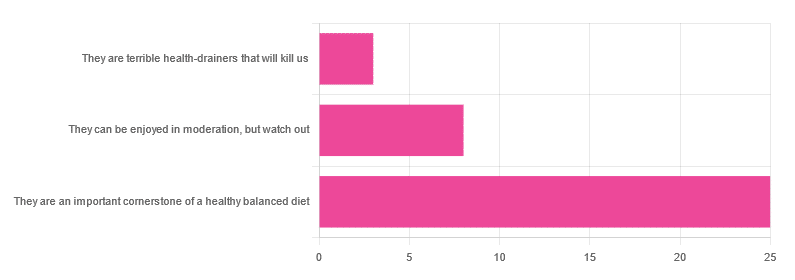
In Wednesday’s newsletter, we asked you for your health-related opinion of grains (aside from any gluten-specific concerns), and got the above-depicted, below-described, set of responses:
- About 69% said “They are an important cornerstone of a healthy balanced diet”
- About 22% said “They can be enjoyed in moderation, but watch out”
- About 8% said “They are terrible health-drainers that will kill us”
So, what does the science say?
They are terrible health-drainers that will kill us: True or False?
True or False depending on the manner of their consumption!
There is a big difference between the average pizza base and a bowl of oats, for instance. Or rather, there are a lot of differences, but what’s most critical here?
The key is: refined and ultraprocessed grains are so inferior to whole grains as to be actively negative for health in most cases for most people most of the time.
But! It’s not because processing is ontologically evil (in reality: some processed foods are healthy, and some unprocessed foods are poisonous). although it is a very good general rule of thumb.
So, we need to understand the “why” behind the “key” that we just gave above, and that’s mostly about the resultant glycemic index and associated metrics (glycemic load, insulin index, etc).
In the case of refined and ultraprocessed grains, our body gains sugar faster than it can process it, and stores it wherever and however it can, like someone who has just realised that they will be entertaining a houseguest in 10 minutes and must tidy up super-rapidly by hiding things wherever they’ll fit.
And when the body tries to do this with sugar from refined grains, the result is very bad for multiple organs (most notably the liver, but the pancreas takes quite a hit too) which in turn causes damage elsewhere in the body, not to mention that we now have urgently-produced fat stored in unfortunate places like our liver and abdominal cavity when it should have gone to subcutaneous fat stores instead.
In contrast, whole grains come with fiber that slows down the absorption of the sugars, such that the body can deal with them in an ideal fashion, which usually means:
- using them immediately, or
- storing them as muscle glycogen, or
- storing them as subcutaneous fat
👆 that’s an oversimplification, but we only have so much room here.
For more on this, see:
Glycemic Index vs Glycemic Load vs Insulin Index
And for why this matters, see:
Which Sugars Are Healthier, And Which Are Just The Same?
And for fixing it, see:
They can be enjoyed in moderation, but watch out: True or False?
Technically True but functionally False:
- Technically true: “in moderation” is doing a lot of heavy lifting here. One person’s “moderation” may be another person’s “abstemiousness” or “gluttony”.
- Functionally false: while of course extreme consumption of pretty much anything is going to be bad, unless you are Cereals Georg eating 10,000 cereals each day and being a statistical outlier, the issue is not the quantity so much as the quality.
Quality, we discussed above—and that is, as we say, paramount. As for quantity however, you might want to know a baseline for “getting enough”, so…
They are an important cornerstone of a healthy balanced diet: True or False?
True! This one’s quite straightforward.
3 servings (each being 90g, or about ½ cup) of whole grains per day is associated with a 22% reduction in risk of heart disease, 5% reduction in all-cause mortality, and a lot of benefits across a lot of disease risks:
❝This meta-analysis provides further evidence that whole grain intake is associated with a reduced risk of coronary heart disease, cardiovascular disease, and total cancer, and mortality from all causes, respiratory diseases, infectious diseases, diabetes, and all non-cardiovascular, non-cancer causes.
These findings support dietary guidelines that recommend increased intake of whole grain to reduce the risk of chronic diseases and premature mortality.❞
~ Dr. Dagfinn Aune et al.
We’d like to give a lot more sources for the same findings, as well as papers for all the individual claims, but frankly, there are so many that there isn’t room. Suffice it to say, this is neither controversial nor uncertain; these benefits are well-established.
Here’s a very informative pop-science article, that also covers some of the things we discussed earlier (it shows what happens during refinement of grains) before getting on to recommendations and more citations for claims than we can fit here:
Harvard School Of Public Health | Whole Grains
“That’s all great, but what if I am concerned about gluten?”
There certainly are reasons you might be, be it because of a sensitivity, allergy, or just because perhaps you’d like to know more.
Let’s first mention: not all grains contain gluten, so it’s perfectly possible to enjoy naturally gluten-free grains (such as oats and rice) as well as gluten-free pseudocereals, which are not actually grains but do the same job in culinary and nutritional terms (such as quinoa and buckwheat, despite the latter’s name).
Finally, if you’d like to know more about gluten’s health considerations, then check out our previous mythbusting special:
Enjoy!
Share This Post
-
Can You Repair Your Own Teeth At Home?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I liked your article on tooth remineralization, I saw a “home tooth repair kit”, and wondered if it is as good as what dentists do, or at least will do the job well enough to save a dentist visit?❞
Firstly, for any wondering about the tooth remineralization, here you go:
Tooth Remineralization: How To Heal Your Teeth Naturally
Now, to answer your question, we presume you are talking about something like this kit available on Amazon. In which case, some things to bear in mind:
- This kind of thing is generally intended as a stop-gap measure until you see a dentist, because you cracked your tooth or lost a filling or something today, and will see the dentist next week, say.
- This kind of thing is not what Dr. Michelle Jorgensen was talking about in another video* that we wrote about; rather, it is using a polymer filler to rebuild what is missing. The key difference is: this is using plastic, which is not what your teeth are made of, so it will never “take” as part of the tooth, as some biomimetic dentistry options can do.
- Yes, this does also mean you are putting microplastics (because the powder is usually micronized polymer beads with zinc oxide, to which you add a liquid to create a paste that will set) in your mouth and quite possibly right next to an open blood supply depending on what’s damaged and whether capillaries were reaching it.
- Because of the different material and application method, the adhesion is nothing like professional fillings (be they metal or resin), and thus the chances of it coming out again or so high that it’s more a question of when, rather than if.
- If you have damage under there (as we presume you do in any scenario where you are using this), then if it’s not professionally cleaned before the filling goes in, then it can get infected, and (less dramatically, but still importantly) any extant decay can also get worse. We say “professionally”, because you will not be able to do an adequate job with your toothbrush, floss, etc at home, and even if you got dentist’s tools (which you can buy, by the way, but we don’t recommend), you will no more be able to do the same quality job as a dentist who has done that many times a day every day for the past 20 years, as buying expensive paintbrushes would make you able to restore a Renaissance painting without messing it up.
*See: Dangers Of Root Canals And Crowns, & What To Do Instead ← what she recommends instead is biomimetic dentistry, which is also more prosaically called “conservative restorative dentistry”, i.e. it tries to conserve as much as possible, replace lost material on a like-for-like basis, and generally end up with a result that’s as close to natural as possible.
In other words, the short answer to your question is “no, sorry, it isn’t and it won’t”
However! A just like it’s good to have a first aid kit in the house even if it won’t do the same job as an ambulance crew, it can be good to have a tooth repair kit (essentially, a tooth first-aid kit) in the house, precisely to use it just as a stop-gap measure in the event that you one day crack a tooth or lose a filling or such, and don’t want to leave it open to all things in the meantime.
(The results of this sort of kit are so not long-term in nature that it will be quick and easy for your dentist to remove it to do their own job once you get there)
If in doubt, always see your dentist as soon as possible, as many things are a lot less work to treat now, than to treat later. Just, make sure to advocate for yourself and what you actually want/need, and don’t let them upsell you on something you didn’t come in for while you’re sitting in their chair—that’s a conversation to be had in advance with a clear head and no pressure (and nobody’s hands in your mouth)!
See also: Dentists Are Pulling ‘Healthy’ and Treatable Teeth To Profit From Implants, Experts Warn
Take care!
Share This Post
Related Posts
-
Black Cohosh vs The Menopause
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Black Cohosh, By Any Other Name…
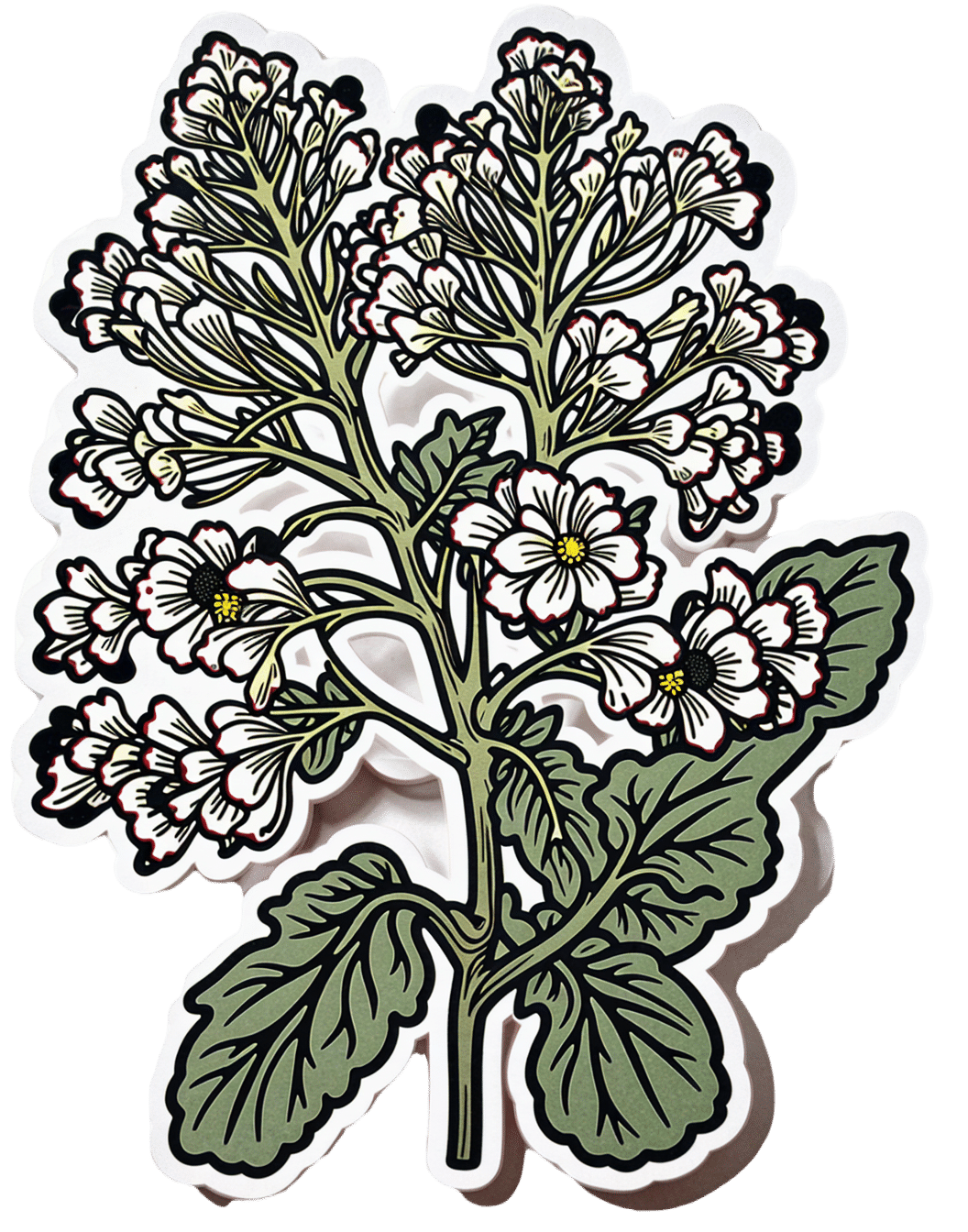
Black cohosh is a flowering plant whose extracts are popularly used to relieve menopausal (and postmenopausal) symptoms.
Note on terms: we’ll use “black cohosh” in this article, but if you see the botanical names in studies, the reason it sometimes appears as Actaea racemosa and sometimes as Cimicfuga racemosa, is because it got changed and changed back on account of some disagreements between botanists. It’s the same plant, in any case!
Read: Reclassification of Actaea to include Cimicifuga and Souliea (Ranunculaceae)
Does it work?
In few words: it works for physical symptoms, but not emotional ones, based on this large (n=2,310) meta-analysis of studies:
❝Black cohosh extracts were associated with significant improvements in overall menopausal symptoms (Hedges’ g = 0.575, 95% CI = 0.283 to 0.867, P < 0.001), as well as in hot flashes (Hedges’ g = 0.315, 95% CIs = 0.107 to 0.524, P = 0.003), and somatic symptoms (Hedges’ g = 0.418, 95% CI = 0.165 to 0.670, P = 0.001), compared with placebo.
However, black cohosh did not significantly improve anxiety (Hedges’ g = 0.194, 95% CI = -0.296 to 0.684, P = 0.438) or depressive symptoms (Hedges’ g = 0.406, 95% CI = -0.121 to 0.932, P = 0.131)❞
~ Dr. Ryochi Sadahiro et al., 2023
Source: Black cohosh extracts in women with menopausal symptoms: an updated pairwise meta-analysis
Here’s an even larger (n=43,759) one that found similarly, and also noted on safety:
❝Treatment with iCR/iCR+HP was well tolerated with few minor adverse events, with a frequency comparable to placebo. The clinical data did not reveal any evidence of hepatotoxicity.
Hormone levels remained unchanged and estrogen-sensitive tissues (e.g. breast, endometrium) were unaffected by iCR treatment.
As benefits clearly outweigh risks, iCR/iCR+HP should be recommended as an evidence-based treatment option for natural climacteric symptoms.
With its good safety profile in general and at estrogen-sensitive organs, iCR as a non-hormonal herbal therapy can also be used in patients with hormone-dependent diseases who suffer from iatrogenic climacteric symptoms.❞
~ Dr. Castelo-Branco et al., 2020
(iCR = isopropanolic Cimicifuga racemosa)
So, is this estrogenic or not?
This is the question many scientists were asking, about 20 or so years ago. There are many papers from around 2000–2005, but here’s a good one that’s quite representative:
❝These new data dispute the estrogenic theory and demonstrate that extracts of black cohosh do not bind to the estrogen receptor in vitro, up-regulate estrogen-dependent genes, or stimulate the growth of estrogen-dependent tumors❞
Source: Is Black Cohosh Estrogenic?
(the abstract is a little vague, but if you click on the PDF icon, you can read the full paper, which is a lot clearer and more detailed)
The short answer: no, black cohosh is not estrogenic
Is it safe?
As ever, check with your doctor as everyone’s situation can vary, but broadly speaking, yes, it has a very good safety profile—including for breast cancer patients, at that. See for example:
- Black cohosh efficacy and safety for menopausal symptoms: the Spanish Menopause Society statement
- Black cohosh (Cimicifuga racemosa): safety and efficacy for cancer patients
- The safety of black cohosh (Actaea racemosa, Cimicifuga racemosa)
Where can I get some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Banana Bread vs Bagel – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing banana bread to bagel, we picked the bagel.
Why?
Unlike most of the items we compare in this section, which are often “single ingredient” or at least highly standardized, today’s choices are rather dependent on recipe. Certainly, your banana bread and your bagels may not be the same as your neighbor’s. Nevertheless, to compare averages, we’ve gone with the FDA’s Food Central Database for reference values, using the most default average recipes available. Likely you could make either or both of them a little healthier, but as it is, this is how we’ve gone about making it a fair comparison. With that in mind…
In terms of macros, bagels have more than 2x the protein and about 4x the fiber, while banana bread has slightly higher carbs and about 7x more fat. You may be wondering: are the fats healthy? And the answer is, it could be better, could be worse. The FDA recipe went with margarine rather than butter, which lowered the saturated fat to being only ¼ of the total fat (it would have been higher, had they used butter) whereas bagels have no saturated fat at all—which characteristic is quite integral to bagels, unless you make egg bagels, which is rather a different beast. All in all, the macros category is a clear win for bagels, especially when we consider the carb to fiber ratio.
In the category of vitamins, bagels have on average more vitamin B1, B3, B5, and B9, while banana bread has on average more of vitamins A and C. A modest win for bagels.
When it comes to minerals, bagels are the more nutrient dense with more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while banana bread is not higher in any minerals. An obvious and easy win for bagels.
Closing thoughts: while the micronutrient profile quite possibly differs wildly from one baker to another, something that will probably stay more or less the same regardless is the carb to fiber ratio, and protein to fat. As a result, we’d weight the macros category as the more universally relevant. Bagels won in all categories today, as it happened, but it’s fairly safe to say that, on average, a baker who makes bagels and banana bread with the same levels of conscientiousness for health (or lack thereof) will tend to make bagels that are healthier than banana bread, based on the carb to fiber ratio, and the protein to fat ratio.
Enjoy!
Want to learn more?
You might like to read:
- Should You Go Light Or Heavy On Carbs?
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Wholewheat Bread vs Seeded White – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reduce Your Stroke Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❝Each year in the U.S., over half a million people have a first stroke; however, up to 80% of strokes may be preventable.❞
~ American Stroke Association
Source: New guideline: Preventing a first stroke may be possible with screening, lifestyle changes
So, what should we do?
Some of the risk factors are unavoidable or not usefully avoidable, like genetic predispositions and old age, respectively (i.e. it is possible to avoid old age—by dying young, which is not a good approach).
Some of the risk factors are avoidable. Let’s look at the most obvious first:
You cannot drink to your good health
While overall, the World Health Organization has declared that “the only safe amount of alcohol is zero”, when it comes to stroke risk specifically, it seems that low consumption is not associated with stroke, while moderate to high consumption is associated with a commensurately increased risk of stroke:
Alcohol Intake as a Risk Factor for Acute Stroke
Note: there are some studies out there that say that a low to moderate consumption may decrease the risk compared to zero consumption. However, any such study that this writer has seen has had the methodological flaw of not addressing why those who do not drink alcohol, do not drink it. In many cases, someone who drinks no alcohol at all does so because either a) it would cause problems with some medication(s) they are taking, or b) they used to drink heavily, and quit. In either case, their reasons for not drinking alcohol may themselves be reasons for an increased stroke risk—not the lack of alcohol itself.
Smoke now = stroke later
This one is straightforward; smoking is bad for pretty much everything, and that includes stroke risk, as it’s bad for your heart and brain both, increasing stroke risk by 200–400%:
Smoking and stroke: the more you smoke the more you stroke
So, the advice here of course is: don’t smoke
Diet matters
The American Stroke Association’s guidelines recommend, just for a change, the Mediterranean Diet. This does not mean just whatever is eaten in the Mediterranean region though, and there are specifically foods that are included and excluded, and the ratios matter, so here’s a run-down of what the Mediterranean Diet does and doesn’t include:
The Mediterranean Diet: What Is It Good For? ← what isn’t it good for?!
You can outrun stroke
Or out-walk it; that’s fine too. Most important here is frequency of exercise, more than intensity. So basically, getting those 150 minutes moderate exercise per week as a minimum.
See also: The Doctor Who Wants Us To Exercise Less & Move More
Which is good, because it means we can get a lot of exercise in that doesn’t feel like “having to do” exercise, for example:
Do You Love To Go To The Gym? No? Enjoy These “No-Exercise Exercises”!
Your brain needs downtime too
Your brain (and your heart) both need you to get good regular sleep:
Sleep Disorders in Stroke: An Update on Management
We sometimes say that “what’s good for your heart is good for your brain” (because the heart feeds the brain, and also ultimately clears away detritus), and that’s true here too, so we might also want to prioritize sleep regularity over other factors, even over duration:
How Regularity Of Sleep Can Be Even More Important Than Duration ← this is about adverse cardiovascular events, including ischemic stroke
Keep on top of your blood pressure
High blood pressure is a very modifiable risk factor for stroke. Taking care of the above things will generally take care of this, especially the DASH variation of the Mediterranean diet:
Hypertension: Factors Far More Relevant Than Salt
However, it’s still important to actually check your blood pressure regularly, because sometimes an unexpected extra factor can pop up for no obvious reason. As a bonus, you can do this improved version of the usual blood pressure test, still using just a blood pressure cuff:
Try This At Home: ABI Test For Clogged Arteries
Consider GLP-1 receptor agonists (or…)
GLP-1 receptor agonists (like Ozempic et al.) seem to have cardioprotective and neuroprotective (thus: anti-stroke) activity independent of their weight loss benefits:
Of course, GLP-1 RAs aren’t everyone’s cup of tea, and they do have their downsides (including availability, cost, and the fact benefits reverse themselves if you stop taking them), so if you want a similar effect from a natural approach, there are some foods that work on the body’s incretin responses in the same way as GLP-1 RAs do:
5 Foods That Naturally Mimic The “Ozempic Effect”
Better to know sooner rather than too late
Rather than waiting until one half of our face is drooping to know that there was a stroke risk, here are things to watch out for to know about it before it’s too late:
6 Signs Of Stroke (One Month In Advance)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: