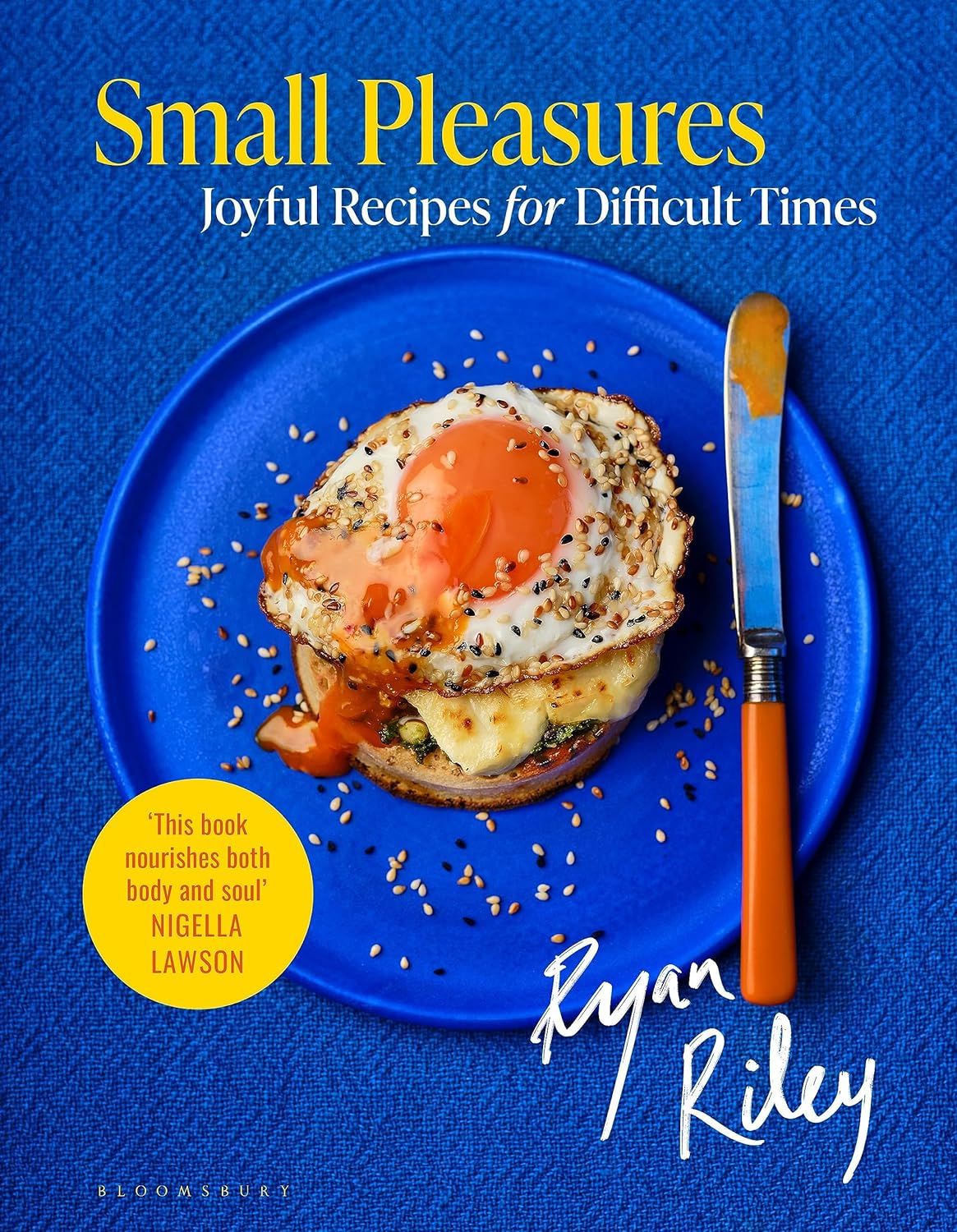
Small Pleasures – by Ryan Riley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Hippocrates said “let food be thy medicine, and let medicine be thy food”, he may or may not have had this book in mind.
In terms of healthiness, this one’s not the very most nutritionist-approved recipe book we’ve ever reviewed. It’s not bad, to be clear!
But the physical health aspect is secondary to the mental health aspects, in this one, as you’ll see. And as we say, “mental health is also just health”.
The book is divided into three sections:
- Comfort—for when you feel at your worst, for when eating is a chore, for when something familiar and reassuring will bring you solace. Here we find flavor and simplicity; pastas, eggs, stews, potato dishes, and the like.
- Restoration—for when your energy needs reawakening. Here we find flavors fresh and tangy, enlivening and bright. Things to make you feel alive.
- Pleasure—while there’s little in the way of health-food here, the author describes the dishes in this section as “a love letter to yourself; they tell you that you’re special as you ready yourself to return to the world”.
And sometimes, just sometimes, we probably all need a little of that.
Bottom line: if you’d like to bring a little more joie de vivre to your cuisine, this book can do that.
Click here to check out Small Pleasures, and rekindle joy in your kitchen!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Keep On Keeping On?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Keep On Keeping On… Long Term!
For many when it comes to health-related goals and practices, it’s easy to find ourselves in a bit of a motivational dip around this time of year. The enthusiasm of new year’s resolutions has been and gone, and there’s not yet much of a drive to “get a beach body” or “be summer-ready”.
A word to the wise on those before moving on, though:
- How to get a beach body: take your body to a beach. Voilà. Beach body.
- Remember: the beach is there for your pleasure and entertainment, not the other way around!
- How to be summer-ready: the real question is, will summer be ready for you?
But what is this, demotivational rhetoric to discourage you from getting fit and healthy?
Not at all, but rather, to be sure that you’re pursuing your own goals and not just what you feel might be expected of you.
All that in mind, let’s get to the tips…
Focus on adding health
It can be tempting (and even, good) to cut down on unhealthy things. But when it comes to motivation, it’s harder to stay motivated for deprivation, than it is for some healthy addition to life.
So for example, this philosophy would advocate for:
- Instead of counting calories, count steps! Or even…
- Instead of counting calories, count colors! Eat the rainbow and all that. No, skittles do not count, but eating a variety of naturally different-colored foods will tend to result in adding different nutrients to your diet.
- Instead of cutting out sugar, add fruit! How many per day will you go for? If you don’t eat much fruit as it is, consider making it a goal to have even just one piece of fruit a day, then build up from there. Find fruit you like! If you pick the fruit you want instead of the fruit you think you “should” have, it’s basically a dessert snack.
We’ve recommended it before, and we’ll recommend it again, but if you’re interested in “adding health”, you should definitely check out:
Dr. Greger’s Daily Dozen (checklist, plus app if you want it)
More details: it’s a checklist of 12 things you should try to include in your diet, with a free streak-tracking app, if you want it, all based on the same scientific research as the best-selling book “How Not To Die”.
“Minimum effort!”
Did you see the movie “Deadpool”? The protagonist has a catch-phrase as he goes into battle, saying to himself “Maximum effort!”.
And, that’s all very well and good if your superpower is immediate recovery from pretty much anything, but for the rest of us, sometimes it’s good to hold ourselves to “minimum effort!”.
Sometimes, something worth doing is worth doing just a little a bit. It’s always better than nothing! Even if feels like you gained nothing from it, it’s the foundation of a habit, and the habit will grow and add up. Sometimes it may even take you by surprise…
Don’t feel like doing 20 bodyweight squats? Do literally just one. Make a deal with yourself: do just one, then you can stop if you like. Then after you’ve done one, you might think to yourself “huh, that wasn’t so bad”, and you try out a few more. Maybe after 5 you can feel your blood pumping a bit and you think “you know what, that’s enough for now”, and great, you did 5x as much exercise as you planned! Wonder what you’ll do tomorrow!
(personal note from your writer here: I’ve managed to “just extend this exercise a little bit more than last time” my way into hour-long exercise sessions before now; I started with “just 10 squats” or “just one sun salutation” etc, to get myself out of a no-exercise period that I’d slipped into, and it’s amazing how quickly adding just a little bit to the previous day’s “minimum effort!” adds up to a very respectable daily exercise session)
Wondering what a good, easy, respectable short term goal could be?
Check Out, For Example: The Seven-Minute Workout
(You might have heard of this one before; it’s an incredibly efficient well-optimized short complete workout that requires no special equipment, just a bit of floorspace and a wall—the above app allows for customizations of it per your preferences, but the basic routine is an excellent starting point for most people)
Commit to yourself (and do any self-negotiation up-front)
Really commit, though. No “or I will look silly because I told people I’d do it”, no “or I will donate x amount to charity” etc, just “I will do it and that’s that”. If you find yourself second-guessing yourself or renegotiating with yourself, just shut that down immediately and refuse to consider it.
Note: you should have break-clauses in this contract with yourself, though. For example, “unless I am ill or injured” is a sensible rule to have in advance for most exercise regimes that weren’t undertaken with your illness or injury in mind.
Make a “To-Don’t” list
Much like how addicts are often advised to not try to quit more than one thing at once, we must also be mindful of not taking on too much at once. It can be very tempting to think:
“I will turn my life around, now! I’ll quit alcohol and animal products and sugar and refined grains, and I’ll go for a run each morning, and I’ll do this and that and there, I’ve got it, here is the blueprint for my healthy perfect life from this day forth!”
And, it’s great to have any and all of that as your end goal if you want, but please, pick one or two things at most to start with, focus on those, and when those have become second nature to you and just a normal part of your life, then choose the next thing to work on.
(You can plan out the whole thing in advance if you want! i.e., I’ll do this, then this, then this, but just… make sure that you’ve really got each one down to a matter of comfort and ease before you take up the next one)
In summary:
- Focus on adding health, whatever that looks like to you
- Figure out what “minimum effort!” is for you, and let that be your baseline
- Commit to yourself (and do any self-negotiation up-front, not later)
- Decide what you’re not going to do yet, and stick to that, too.
Share This Post
- How to get a beach body: take your body to a beach. Voilà. Beach body.
-
Beyond “Make Your Bed”—life lessons from experience
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beyond “Make Your Bed”—life lessons from experience
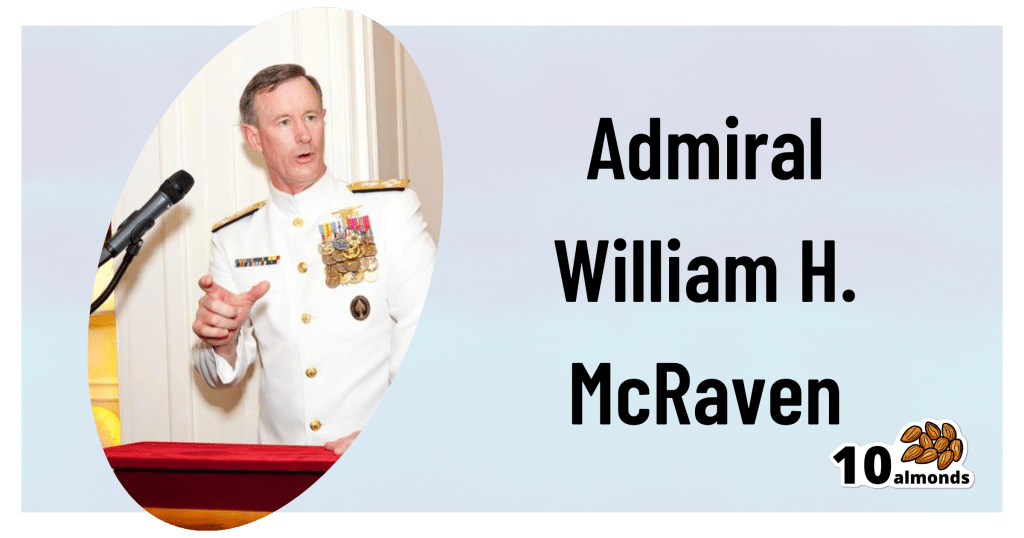
This is Admiral William H. McRaven, a former United States Navy four-star admiral who served as the ninth commander of the United States Special Operations Command.
So, for those of us whose day-to-day lives don’t involve coordinating military operations, what does he have to offer?
Quick note: 10almonds’ mission statement is “to make health and productivity crazy simple”.
We tend to focus on the health side of this, and in the category of productivity, it’s often what most benefits our mental health.
We’re writing less for career-driven technopreneurs in the 25–35 age bracket and more for people with a more holistic view of productivity and “a good life well-lived”.
So today’s main feature is more in that vein!
Start each day with an accomplishment
McRaven famously gave a speech (and wrote a book) that began with the advice, “make your bed”. The idea here doesn’t have to be literal (if you’ll pardon the pun). Indeed, if you’re partnered, then depending on schedules and habits, it could be you can’t (sensibly) make your bed first thing because your partner is still in it. But! What you can do is start the day with an accomplishment—however small. A short exercise routine is a great example!
Success in life requires teamwork
We’re none of us an island (except in the bathtub). The point is… Nobody can do everything alone. Self-sufficiency is an illusion. You can make your own coffee, but could you have made the coffee machine, or even the cup? How about, grown the coffee? Transported it? So don’t be afraid to reach out for (and acknowledge!) help from others. Teamwork really does make the dream work.
It’s what’s inside that counts
It’s a common trap to fall into, getting caught up the outside appearance of success, rather than what actually matters the most. We need to remember this when it comes to our own choices, as well as assessing what others might bring to the table!
A setback is only permanent if you let it be
No, a positive attitude won’t reverse a lifelong degenerative illness, for example. But what we can do, is take life as comes, and press on with the reality, rather than getting caught up in the “should be”.
Use failure to your advantage
Learn. That’s all. Learn, and improve.
Be daring in life
To borrow from another military force, the SAS has the motto “Who dares, wins”. Caution has it place, but if we’ve made reasonable preparations*, sometimes being bold is the best (or only!) way forward.
*Meanwhile the Parachute Regiment, from which come 80% of all SAS soldiers, has the motto “Utrinque paratus”, “prepared on all sides”.
Keep courage close
This is about not backing down when we know what’s right and we know what we need to do. Life can be scary! But if we don’t overcome our fears, they can become self-realizing.
Writer’s note: a good example of this is an advice I sometimes gave during my much more exciting (military) life of some decades ago, and it pertains to getting into a knife-fight (top advice for civilians: don’t).
But, if you’re in one, you need to not be afraid of getting cut.
Because if you’re not afraid of getting cut, you will probably get cut.
But if you are afraid of getting cut, you will definitely get cut.
Hopefully your life doesn’t involve knives outside of the kitchen (mine doesn’t, these days, and I like it), but the lesson applies to other things too.
Sometimes the only way out is through.
Be your best at your worst
Sometimes life is really, really hard. But if we allow those moments to drive us forwards, they’re also a place we can find more strength than we ever knew we had.
Keep on swimming
It’s said that the majority in life is about showing up—and often it is. But you have to keep showing up, day after day. So make what you’re doing sustainable for you, and keep on keeping on.
Share This Post
-
All In Your Head (Which Is Where It’s Supposed To Be)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s news is all about things above the neck, and mostly in the brain. From beating depression to beating cognitive decline, from mindfulness against pain to dentistry nightmares to avoid:
Transcranial ultrasound stimulation
Transcranial magnetic stimulation is one of those treatments that sounds like it’s out of a 1950s sci-fi novel, and yet, it actually works (it’s very well-evidenced against treatment-resistant depression, amongst other things). However, a weakness of it is that it’s difficult to target precisely, making modulation of most neurological disorders impossible. Using ultrasound instead of a magnetic field allows for much more finesse, with very promising initial results across a range of neurological disorders
Read in full: Transcranial ultrasound stimulation: a new frontier in non-invasive brain therapy
Related: Antidepressants: Personalization Is Key!
This may cause more pain and damage, but at least it’s more expensive too…
While socialized healthcare systems sometimes run into the problem of not wanting to spend money where it actually is needed, private healthcare systems have the opposite problem: there’s a profit incentive to upsell to more expensive treatments. Here’s how that’s played out in dentistry:
Read in full: Dentists are pulling healthy and treatable teeth to profit from implants, experts warn
Related: Tooth Remineralization: How To Heal Your Teeth Naturally
Mindfulness vs placebo, for pain
It can be difficult with some “alternative therapies” to test against placebo, for example “and control group B will merely believe that they are being pierced with needles”, etc. However, in this case, mindfulness meditation was tested as an analgesic vs sham meditation (just deep breathing) and also vs placebo analgesic cream, vs distraction (listening to an audiobook). Mindfulness meditation beat all of the other things:
Read in full: Mindfulness meditation outperforms placebo in reducing pain
Related: No-Frills, Evidence-Based Mindfulness
Getting personal with AI doctors
One of the common reasons that people reject AI doctors is the “lack of a human touch”. However, human and AI doctors may be meeting in the middle nowadays, as humans are pressed to see more patients in less time, and AI is trained to be more personal—not just a friendlier affect, but also, such things as remembering the patient’s previous encounters (again, something with which overworked human doctors sometimes struggle). This makes a big difference to patient satisfaction:
Read in full: Personalization key to patient satisfaction with AI doctors
Related: AI: The Doctor That Never Tires?
Combination brain therapy against cognitive decline
This study found that out of various combinations trialled, the best intervention against cognitive decline was a combination of 1) cognitive remediation (therapeutic interventions designed to improve cognitive functioning, like puzzles and logic problems), and 2) transcranial direct current stimulation (tDCS), a form of non-invasive direct brain stimulation, similar to the magnetic or ultrasound methods we mentioned earlier today. Here’s how it worked:
Read in full: Study reveals effective combination therapy to slow cognitive decline in older adults
Related: How To Reduce Your Alzheimer’s Risk
Take care!
Share This Post
Related Posts
-
Bath vs Shower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing bathing to showering, we picked the shower.
Why?
For the basic task of getting your body clean, the shower is better as it is an entirely one-way process. Clean water hits your body, dirty water leaves it, and no dirt is making its way back.
Baths do not have this advantage, and if you enter a bath dirty, you will then be sitting in dirty water. You will leave it a lot cleaner than you entered it (because a lot of the dirt stayed in the bathwater to be drained away after the bath), but not as clean as if you had showered.
One could argue soap or equivalent will prevent the dirt re-sticking, and that’s true, but it’s true for soap in the shower too, so it doesn’t offset anything.
Additionally, being immersed in water for more than 15 minutes can start to have a (paradoxically) dehydrating effect on the skin; this happens not only because of losing skin oils to the water, but also because of osmosis, the resultant mild edema, the body’s homeostatic response to the mild edema, then getting out the bath and drying, leaving one with the response having now just caused dehydrated skin.
Baths do have some health advantages! And these come primarily from the mental health benefits of relaxation in warm water and/or generally pampering oneself. Additionally, some bath oils or bath salts can be beneficial in a way that couldn’t be administered the same way in the shower.
Best of both worlds?
In some parts of the world (Thailand and Turkey come to mind; doubtlessly there are many others) there are traditions of first taking a shower to get clean, and then taking a bath for the rest of the bathing experience. As a bonus, the bathing experience is then all the more pleasant for the water remaining just as clean as it was to start with.
However, if you do have to pick one (and for the purpose of our “This or That” exercise, we do), then it’s the shower, hands-down.
Want to read more?
You might want to also take into account how it’s still possible to have too much of a good thing:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Four Ways To Upgrade The Mediterranean Diet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Four Ways To Upgrade The Mediterranean Diet
The Mediterranean Diet is considered by many to be the current “gold standard” of healthy eating, and with good reason. With 10,000+ studies underpinning it and counting, it has a pretty hefty weight of evidence.
(For contrast, the Ketogenic Diet for example has under 5,000 studies at time of writing, and many of those include mentioning the problems with it. That’s not to say the Keto is without its merits! It certainly can help achieve some short term goals, but that’s a topic for another day)
Wondering what the Mediterranean Diet consists of? We outlined it in a previous main feature, so here it is for your convenience 😎
To get us started today, we’ll quickly drop some links to a few of those Mediterranean Diet studies from the top:
- Definition of the Mediterranean Diet; a Literature Review
- Mediterranean Diet In Healthy Aging
- Cancer and Mediterranean Diet: A Review
- Impact of Mediterranean Diet on Chronic Non-Communicable Diseases and Longevity
- Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies
- Adherence to Mediterranean diet and health status: meta-analysis
The short version is: it glows, in a good way.
The anti-inflammatory upgrade
One thing about the traditional Mediterranean Diet is… where are the spices?!
A diet focusing on fruits and non-starchy vegetables, healthy oils and minimal refined carbs, can be boosted by adding uses of spices such as chili, turmeric, cumin, fenugreek, and coriander:
The gut-healthy upgrade:
The Mediterranean Diet already gives for having a small amount of dairy, mostly in the form of cheeses, but this can be tweaked:
Mediterranean diet with extra dairy could be a gut gamechanger
The heart-healthy upgrade
The Mediterranean Diet is already highly recommended for heart health, and it offers different benefits to different parts of cardiovascular health:
The DASH (Dietary Approaches to Stop Hypertension) diet can boost it further, specifically in the category of, as the name suggests, lowering blood pressure.
It’s basically the Mediterranean Diet with a few tweaks. Most notably, red meat no longer features (the Mediterranean Diet allows for a small amount of red meat), and fish has gone up in the list:
Description of the DASH Eating Plan
The brain-healthy upgrade:
The MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet combines several elements from the above, as the name suggests. It also adds extra portions of specific brain-foods, that already exist in the above diets, but get a more substantial weighting in this one:
MIND and Mediterranean diets linked to fewer signs of Alzheimer’s brain pathology
See also: The cognitive effects of the MIND diet
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Heal And Regrow Receding Gums
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝So, I have a topic that I’d love you guys to discuss: green tea. I used to try + drink it years ago but I always got an allergic reaction to it. So the question I’d like answered is: Will I still get the same allergic reaction if I take the capsules ? Also, because it’s caffeinated, will taking it interfere with iron pills, other vitamins + meds ? I read that the health benefits of the decaffeinated tea/capsules are not as great as the caffeinated. Any info would be greatly appreciated !! Thanks much !!❞
I’ll answer this one in the first person as I’ve had a similar issue:
I found long ago that taking any kind of tea (not herbal infusions, but true teas, e.g. green tea, black tea, red tea, etc) on an empty stomach made me want to throw up. The feeling would subside within about half an hour, but I learned it was far better to circumvent it by just not taking tea on an empty stomach.
However! I take an l-theanine supplement when I wake up, to complement my morning coffee, and have never had a problem with that. Of course, my physiology is not your physiology, and this “shouldn’t” be happening to either of us in the first place, so it’s not something there’s a lot of scientific literature about, and we just have to figure out what works for us.
I’d hypothesize that the reason tea causes a problem but the supplement doesn’t, is because the reaction is not to the l-theanine, but rather to the tannins in the tea.
This last Monday I wrote (inspired in part by your query) about l-theanine supplementation, and how it doesn’t require caffeine to unlock its benefits after all, by the way. So that’s that part in order.
I can’t speak for interactions with your other supplements or medications without knowing what they are, but I’m not aware of any known issue, beyond that l-theanine will tend to give a gentler curve to the expression of some neurotransmitters. So, if for example you’re talking anything that affects that (e.g. antidepressants, antipsychotics, ADHD meds, sleepy/wakefulness meds, etc) then checking with your doctor is best.
❝Can you do something on collagen and keep use posted on pineapple, and yes love and look forward to each issue❞
Glad you’re enjoying! We did write a main feature on collagen a little while back! Here it is:
We Are Such Stuff As Fish Are Made Of
As for pineapple, there’s not a lot to keep you posted about! Pineapple’s protein-digesting, DNA-unzipping action is well-established and considered harmless (if your mouth feels weird when you eat pineapple or drink pineapple juice, this is why, by the way) because no meaningful damage was done.
For example:
- Pineapple’s bromelain action is akin to taking apart a little lego model brick by brick (easy to fix)
- Clastogenic genotoxicity is more like taking a blowtorch to the lego model (less easy to fix)
Fun fact: pineapple is good against inflammation, because of the very same enzyme!
❝I never knew anything about the l- tea. Where can I purchase it?❞
You can get it online quite easily! Here’s an example on Amazon
❝The 3 most important exercises don’t work if you can’t get on the floor. I’m 78, and have knee replacements. What about 3 best chair yoga stretches? Love your articles!❞
Here are six!
We turn the tables and ask you a question!
We’ll then talk about this tomorrow:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: